 |
|
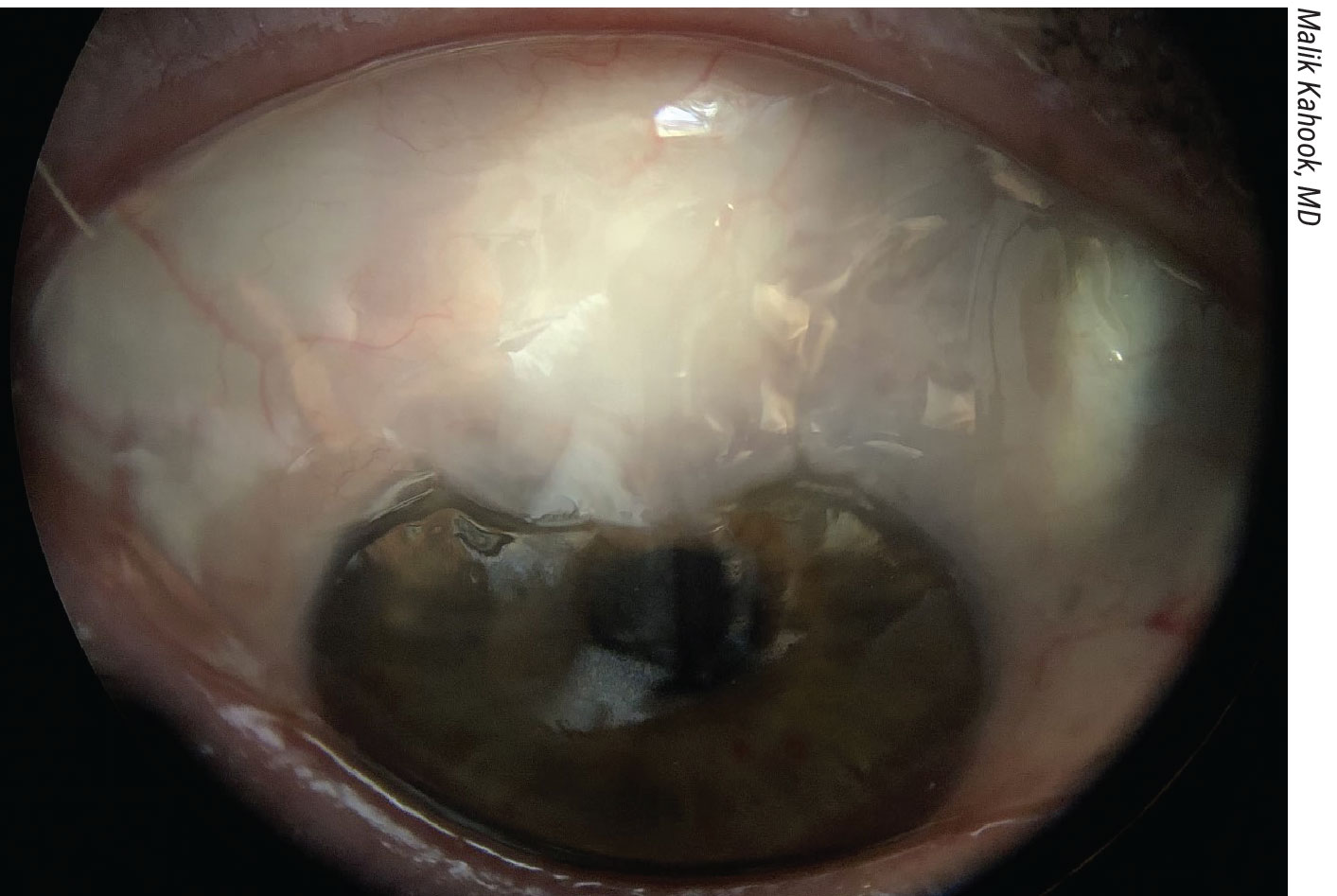
A diffuse filtration bleb post-trabeculectomy with mitomycin C. |
Minimally-invasive glaucoma surgery is typically the procedure of choice for patients who are in the early stages of glaucoma and who have a target pressure in the mid to high teens. For patients who require a lower IOP, trabeculectomy or tube shunts are an effective alternative. Here, glaucoma specialists discuss where these “big guns” of glaucoma surgery still fit in the treatment armamentarium.
“I also use MIGS procedures in more advanced disease when the IOP target is still the mid teens and the goal is lowering dependency on drops and pushing off the need for filtration surgery for as long as possible,” says Malik Kahook, MD, from the University of Colorado School of Medicine in Aurora. “In short, there is still a significant role for all of the surgeries we do now. The main difference over the past decade of practice is that I now have the ability to tailor therapies to specific situations and with confidence that many other options exist if I were to need them.”
Indiana’s Louis Cantor, MD, notes that surgery enters the picture when either a patient’s pressure is too high or there’s rapid progression of visual field loss. “Then, we have to make decisions about what surgical procedure to consider,” he says. “There’s certainly been a rapidly growing adoption of less-invasive MIGS procedures for early glaucoma, mild glaucoma and moderate glaucoma. I think that’s certainly reasonable, but it’s not a one-size-fits-all. There are still many indications for going beyond a MIGS procedure to trabeculectomy or tube shunt. In my opinion, trabeculectomy remains the gold standard against which other procedures are compared.”
Comparing Trabeculectomies and Tubes with MIGS
Trabeculectomies or non-valved tubes may be the best option to achieve an IOP lower than 12 mmHg. “Even though there are many minimally invasive options, it’s very difficult to get sub-12 pressures with other procedures,” says Richard Lehrer, MD, who is in practice in Alliance, Ohio.
The well-known drawback is that complications are much more common with trabeculectomies than with MIGS. “We can have pressures too high, pressures too low, scarring of the trab flap, early leaks, late leaks, bleb infections, hypotony maculopathy, choroidal effusions, and suprachoroidal hemorrhages. There are very few complications that most experienced glaucoma specialists haven’t seen over their careers.”
A recent study compared the efficacy and safety profile of Xen microstent implantation with trabeculectomy in a comparable group of open-angle glaucoma cases in a retrospective, monocentric, single-surgeon setting.1
Each treatment group included 100 eyes of 100 patients. At regular follow-up visits during the first 12 months after surgery, the following assessments were performed and compared: IOP, number of IOP-lowering medications, best-corrected visual acuity and visual field testing. In both groups, the mean IOP was significantly reduced by the procedure. Mean IOP decreased from 24.8 ± 7.8 to 14.8 ± 4 mmHg in the trabeculectomy group and from 24.5 ± 6.7 to 16.6 ± 4.8 mmHg in the Xen group. The number of active compounds in the prescribed medication decreased from 3.3 ± 1.2 to 1.3 ± 1.4 in the trabeculectomy group and from 3.0 ± 1.1 to 1.4 ± 1.5 in the Xen group. Additionally, there was no statistically significant change in best-corrected visual acuity and mean defect of static automated perimetry in either group. Complications were more frequent after trabeculectomy, while postoperative needling was more frequent in the Xen group. Both procedures resulted in a significant reduction of IOP and IOP-lowering medication, while best-corrected visual acuity and visual field indices remained mostly unchanged during the 12-month follow-up.
According to Dr. Cantor, patients are typically candidates for trabeculectomy or a tube shunt because MIGS procedures have failed. “Most often, patients have had a cataract surgery with a MIGS procedure combined, and their pressure is still uncontrolled, they’re on medications, and they’re progressing,” he says. “However, I believe that there are patients in whom a primary trabeculectomy may be indicated even prior to attempting a MIGS procedure. These patients include those with advanced glaucoma who are on multiple medications and are progressing at a rapid rate. These patients—the rapid progressors—become blind from glaucoma. At this point in their disease, there’s a fairly narrow window of opportunity to try to stop the glaucoma and preserve functional vision. Trying a MIGS procedure in a patient with a 0.95 cup with a pressure of 30 mmHg on every known medicine probably doesn’t serve that patient well. The risk-benefit ratio there certainly favors a trabeculectomy or, if you prefer, a tube shunt. Personally, I generally perform trabeculectomy before going to tube shunts.”
Reay Brown, MD, in practice in Atlanta, adds that some surgeons might choose to bypass MIGS if the pressure is 40 mmHg and the patient is on maximal medical therapy. “In those cases, you might go right to a trabeculectomy or a tube in a setting where there’s visual field loss,” he says. “Then, as you encounter patients with less severe disease, I personally feel like everyone should have a MIGS step before a trab or tube. So, if the patient isn’t too severe and has pressures that aren’t too high, a MIGS procedures is always the best next step. But patients who have more extensive visual field loss, who have higher pressures, who don’t tolerate medical therapy are the ones who need a trabeculectomy or a tube.”
Leonard Seibold, MD, from the University of Colorado School of Medicine in Aurora, agrees. “With the advantages of less-invasive glaucoma procedures that we have available today, such as rapid vision recovery, improved safety profile, and avoidance of serious complications of bleb-forming procedures, I typically will elect for a less-invasive procedure as a first-line surgical method,” he says. “If those fail, I move on to a more traditional surgery like a trab or a tube. But, it also depends on patient-specific characteristics, such as whether the patient has a closed angle or some other feature of their disease that would make an angle-based surgery contraindicated. In some cases, we may elect to perform a more traditional surgery first.”
In addition to being more invasive, trabs and tubes have a longer postoperative recovery time. “Vision recovery sometimes can take months to fully stabilize, and patients require many more postoperative visits,” notes Dr. Seibold. “From a patient perspective, it’s a much larger commitment as far as time, number of visits, risk to the eye and downtime. Additionally, patients are putting themselves at increased risk of serious complications, such as endophthalmitis and hypotony. From a physician perspective, the postoperative recovery can be very erratic. You can have very high and low pressures, often within a couple of days of each other. They also require postoperative manipulations and adjustments, and you’re constantly at the mercy of how the eye decides to heal, so it’s very difficult to predict how each individual eye is going to heal despite doing the exact same surgery each time.”
Comparing Trabeculectomies With Tubes
Dr. Lehrer says that valved tubes are his procedure of choice for patients with neovascular glaucoma or for patients who have failed multiple bleb-forming procedures. “In my practice, I rarely use non-valved tubes,” he says. “Multiple studies have shown that, in conditions like neovascular glaucoma, the rate of vision loss is higher with non-valved tubes than with valved tubes. Even though the pressures don’t get quite as low, the chance of success and of not losing vision is a little bit higher with valved versus non-valved tubes, so that’s generally my tube of choice.”
Dr. Cantor adds that choosing between trabs and tubes depends on the complexity of the case. “If a patient has uveitic, neovascular or traumatic glaucoma, I may forgo a trab for a tube shunt,” he explains. “But, for the standard primary open-angle glaucoma patient or even those with pseudoexfoliation or pigmentary glaucoma, I’ll opt for a trabeculectomy initially before considering a tube shunt, only if the trabeculectomy fails.”
As an example, a recent study found that Baerveldt glaucoma implant surgery had a higher success rate compared with trabeculectomy in patients with neovascular glaucoma for a target IOP of less than 21 mmHg and less than 17 mmHg, while the rates of postoperative complications were similar between both surgical procedures.2 Additionally, another glaucoma procedure was required more frequently after trabeculectomy than after Baerveldt glaucoma implant surgery.
This Japanese study included 304 eyes with neovascular glaucoma: 100 eyes underwent Baerveldt glaucoma implant surgery, and 204 eyes underwent trabeculectomy.
According to the study results, the probability of success was significantly higher in patients undergoing Baerveldt glaucoma implant surgery than in those receiving trabeculectomy for a target IOP of less than 21 mmHg and less than 17 mmHg. Additionally, trabeculectomy was significantly associated with surgical failure in the multivariable analysis for target pressures of less than 21 mmHg and less than 17 mmHg. Although the overall incidence of postoperative complications was similar between the two groups, reoperations for glaucoma were required significantly more frequently in the trabeculectomy group than in the Baerveldt glaucoma implant surgery group.
The well-known Tube vs. Trabeculectomy Study found that the success and complication rates of trabeculectomies and tubes were very similar at five years.3 This multicenter randomized clinical trial included 242 eyes in 242 patients with medically uncontrolled glaucoma and no previous incisional ocular surgery: 125 patients were in the tube group, and 117 patients were in the trabeculectomy group. Treatment consisted of a 350-mm2 Baerveldt glaucoma implant or a trabeculectomy with mitomycin C (0.4 mg/mL for two minutes).
Twenty-four patients in the tube group and 40 patients in the trabeculectomy group experienced early postoperative complications. Late postoperative complications developed in 27 patients in the tube group and 32 patients in the trabeculectomy group. Serious complications producing vision loss and/or requiring a reoperation were observed in three patients in the tube group and nine patients in the trabeculectomy group. Cataract progression was seen in 65 patients in the tube group and 52 patients in the trabeculectomy group. Surgical complications weren’t associated with a higher rate of treatment failure, vision loss or cataract progression.
“Both procedures had some serious complications. That’s always been the issue with trabs and tubes—there’s too much risk of infection, bleeding, choroidal detachment, hypotony, and others,” Dr. Brown says. “It’s a disappointment to me, having done this for 40 years, that we don’t have a better option for advanced disease than a trab or a tube. That’s a sad commentary.”
The Future
Dr. Lehrer believes that there will still be a place for trabeculectomies and tubes until there’s a glaucoma treatment that doesn’t involve lowering pressure. “Right now, the only thing we can do to successfully treat glaucoma most of the time is to lower the pressure,” he says. “I wish we were more sophisticated, but we’re really not.”
Dr. Seibold agrees. “Until we have a less-invasive procedure that can consistently provide low pressures, there will always be a place for these procedures,” he says. “As much as we’d like to see them go away completely, we’re still a long way off from eliminating them. I think the number of tubes and trabs that we’re doing will continue to decline more and more as we not only develop newer, less-invasive procedures, but also figure out how to use those better so that we’re more successful with them. However, while this would minimize the need for tubes and trabs, I think there will probably always be a need.”
Dr. Brown is the Chief Medical Officer for Sight Sciences. Dr. Kahook is a consultant to New World Medical, is an owner of SpyGlass Pharma, and receives patent royalties from New World Medical and Alcon. Dr. Lehrer is a consultant to Bausch + Lomb, an investigator for Glaukos, and a consultant to and on the speakers bureau of Alcon. Dr. Seibold is a consultant to New World Medical and Allergan.
1. Theilig T, Rehak M, Busch C, Bormann C, Schargus M, Unterlauft JD. Comparing the efficacy of trabeculectomy and XEN gel microstent implantation for the treatment of primary open-angle glaucoma: A retrospective monocentric comparative cohort study Sci Rep. 2020;10:19337.
2. Iwasaki K, Kojima S, Wajima R, et al. Comparing surgical outcomes in neovascular glaucoma between tube and trabeculectomy: A multicenter study. Ophthalmol Glaucoma 2022;5:6:672-680.
3. Gedde SJ, Feuer WJ, Lim KS, et al; Primary Tube Versus Trabeculectomy Study Group. Postoperative complications in the primary tube versus trabeculectomy study during 5 years of follow-up. Ophthalmology 2022;129:12:1357-1367.




