Due to its variable presentation, dry eye can be a multilayered, complex problem, and there are a number of different ways of addressing each aspect of the disease. Typical treatments range from lifestyle changes and OTC and prescription drops to punctal plugs, scleral lenses and devices that stimulate tear production. Here, we’ll discuss treatment strategies, and review the latest drugs and devices for managing the various components of dry eye.
The State of Dry Eye
“When I was a resident, treating dry eye was mainly a matter of giving a patient some drops,” says Douglas K. Grayson, MD, of Omni Eye Services, which has multiple offices in the New Jersey-New York City area. “In the past 10 years, however, it’s been taken more seriously. There are more treatments available today. Multifocal lens use has also made us more conscious of treating dry eye, both preliminarily and afterward. You’re not going to get good results otherwise; dry eye will decrease the accuracy of measurements like keratometry.”
“Dry eye is a tough disease to treat because it’s multifactorial and has many possible causes,” says Sydney L. Tyson, MD, MPH, of Wills Eye Hospital in Philadelphia. “The disease may be related to evaporation, systemic illness or meibomian gland dysfunction, for example. When you have that type of multifactorial issue going on, it makes it difficult to nail down one treatment that will work for everybody.”
That may be one of the reasons dry-eye treatments have been slower to develop, relative to other areas in ophthalmology, Dr. Tyson reasons. “For the longest time, we had cyclosporine, and then we added lifitegrast,” he says. “But dry-eye medications just haven’t had a technological renaissance like cataract surgery or glaucoma with MIGS devices.”
“I think we’re just beginning to understand dry eye,” says Mitchell P. Weikert, MD, MS, professor of ophthalmology at Baylor College of Medicine in Houston. “In the past decade we’ve realized there’s a major inflammatory component to dry eye. That seems to be where several of the breakthroughs have been, in terms of management. Now we have access to different formulations of cyclosporine.”
Cyclosporine has been around for many years and forms the basis for most prescription dry-eye medications such as Klarity-C (ImprimisRx), Restasis (Allergan) and a new drug formulation called Cequa (Sun Ophthalmics), whose novel mechanism of action employs nanomicellar technology to keep the cyclosporine suspended in solution and aid in cell absorption. “Packaging the individual molecules of cyclosporine in micelles is a fairly innovative delivery system for the medication,” Dr. Weikert notes.
A lifitegrast formulation like Xiidra (Novartis) approaches dry eye differently from cyclosporine. “Lifitegrast uses cellular adhesion molecules to interrupt the inflammatory cascade of dry eye,” says Dr. Weikert. “It blocks the interactions between T-cells, ocular surface cells and the antigen-presenting cells to dampen the inflammatory cascade that can happen with dry eye. When you decrease T-cell activation, you decrease the release of pro-inflammatory cytokines.”
“Drops are a first-line therapy for dry eye, but patients have variable responses and side effects,” Dr. Tyson points out. “In addition to occasional burning, drops can be expensive, so we sometimes use compounded medication instead, which is a little less expensive. Some patients report that the drops taste bad. Even though they’re in the eye, these medications can still cause a metallic taste in the mouth. Other options include omega-3 fatty acid pills, which can be taken orally by patients to help dry-eye symptoms as well.”
 |
 |
Treatment Approaches
Treating dry eye is a matter of finding the right combination of therapies, Dr. Tyson explains. “It’s a long-term treatment, not a cure,” he says. “As dry eye worsens, we up the ante in terms of therapy. A stepwise approach is necessary.”
Dr. Weikert divides his dry-eye management strategies into four categories: increase tear production; tear replacement; improve tear quality; and protect the ocular surface. “Anti-inflammatory medication helps to increase tear production,” he says. “In terms of replacing tears, there are many artificial tears available with different compositions, and they’re better than what we had in the past. They don’t address the root cause of inflammation, however.”
Inflammation lies at the heart of most dry-eye disease, physicians say, so identifying the source or sources of inflammation is key to formulating your approach. “Evaporation and meibomian gland dysfunction are two ways that inflammation processes affect the lacrimal gland,” Dr. Tyson explains. For mild to moderate forms of dry eye, Dr. Tyson often turns to artificial tears or punctal plugs.
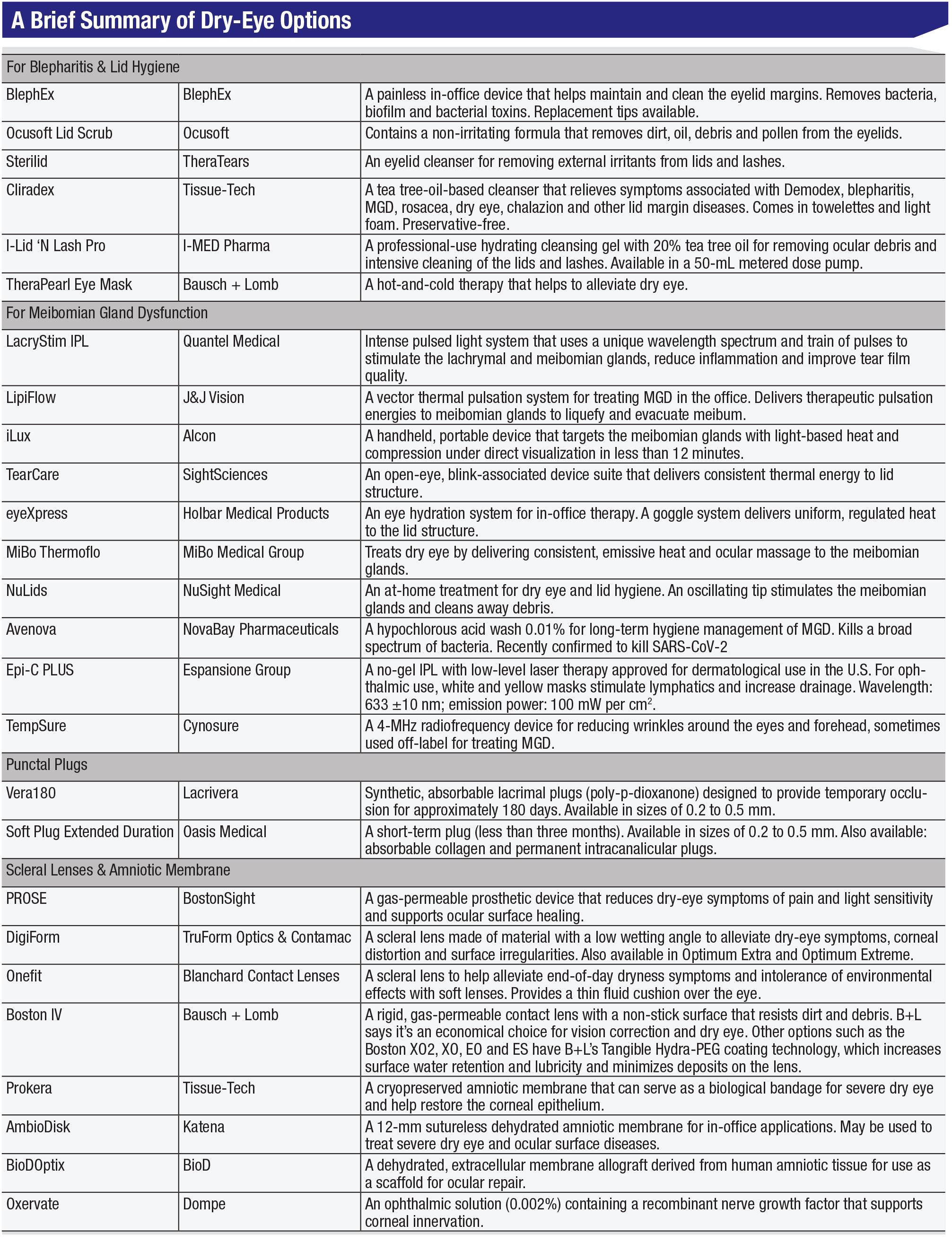
“If the dry eye is related to evaporation, there are only two ways to fix it: You can either increase tear production or increase the supply and retain more tears,” he continues. “That’s where punctal plugs come in. If the dry eye is more of a meibomian gland issue, we do warm compresses, lid hygiene and use devices like BlephEx (BlephEx), which exfoliates the biofilm on the lid surface to remove bacteria and exotoxins. We can also use heating treatments or intense pulsed light therapies like LipiFlow (Johnson & Johnson Vision) or iLux (Alcon) for meibomian gland dysfunction.
“Using tears is a major part of the dry-eye regimen,” agrees Dr. Grayson. “A short course of Lotemax (Bausch + Lomb) or a steroid drop for a while is another option. More serious cases may warrant something like Restasis, Xiidra or Cequa for a few weeks. For very severe cases, you may want to use an amniotic membrane graft such as Prokera (Bio-Tissue) [a cryopreserved AMG] or BioDOptix (BioD) [a dehydrated AMG].” AmbioDisk (Katena) is another dehydrated amniotic membrane option.
Expressing Meibomian Glands
A recently published study of dry-eye disease symptoms found that in the sample population (n=2,346; 77.4 percent female, 87.1 percent Chinese), meibomian gland dysfunction, along with lower forniceal papillary reaction, was the primary determinant of symptoms, contributing significantly to symptom severity compared to traditional dry-eye signs.1
Poor tear quality is often secondary to blepharitis, resulting from blocked meibomian glands. “Doxycycline and azithromycin are classic treatments for blepharitis,” Dr. Weikert says. “They have some anti-inflammatory properties as well.”
Manual therapies are also suitable for blepharitis. Dr. Grayson says he recommends using warm washcloths, baby shampoo or lid-scrub pads to help clear up symptoms.
For more serious cases, heating the meibomian glands with a device is a common way to express the glands and return the meibum to the proper consistency for better tear film quality. “LipiFlow (J&J Vision) clips around the eyelids and heats the meibomian glands to express them and mobilize the oils out of the glands,” says Dr. Weikert. The iLux (Alcon) and the MiBo Thermoflo (MiBo Medical Group) work in a similar manner. The NuLids device, which patients can use at home, also helps treat MGD by massaging the glands.
However, Dr. Weikert points out that in order to improve the meibomian glands and their secretions, your patient has to have meibomian glands. “Those with very advanced blepharitis may have lost their meibomian glands and therefore won’t be candidates for treatment because there’s nothing left to treat, or it’s substantially reduced,” he says.
Supplementing Tears
“Artificial tears still play a valuable role by supplementing tears,” Dr. Weikert says. “They’re a low-cost alternative that can help people with mild dry eye. Some people do get by with only a little tear replacement once a day, but those are very mild cases; anything more than that requires additional therapy.
“We blink every six to 10 seconds, so you need tears that don’t evaporate for at least that amount of time,” Dr. Weikert continues. “Many patients have tear instability, and their tears evaporate in only two to three seconds, so before their next blink, their ocular surface is exposed to the air for several seconds. That exacerbates surface damage.”
Dr. Grayson points out that there’s a new over-the-counter eye drop called Optase, which has hyaluronic acid and artificial tears in it. He has yet to try it out. Optase (Scope) is part of a dry-eye regimen that includes a moist-heat mask and eyelid cleansing wipes along with a dry-eye spray.
Popular among Dr. Grayon and his colleagues is Freshkote (Eyevance), another OTC artificial tear. “It’s more of a milky drop,” Dr. Grayson says. “It has antimicrobial properties as well.” Freshkote consists of a blend of polyvinyl alcohol 2.7% and povidone 2%, which Eyevance says results in a high oncotic pressure on the ocular surface that draws excess water from epithelial cells.
Another way to increase tear production is through nerve stimulation, the mechanism of action behind Allergan’s now-defunct intranasal tear stimulator, TrueTear. The TrueTear device activated the nasolacrimal reflex by delivering electrical currents to the neurons in the nasal cavity to temporarily increase tear production. Allergan stopped manufacturing TrueTear recently and is offering full refunds for devices purchased within the last three years. The company says the decision has nothing to do with the safety or efficacy of the product.
There are also some at-home methods, including a forthcoming medication in development by Oyster Point Pharmaceuticals in the form of a preservative-free nasal spray. This spray is a nicotinic acetylcholine receptor agonist that helps the parasympathetic nervous system promote natural tear-film production and re-establish tear-film homeostasis.
Clinical evidence for a handheld device called iTear (Olympic Ophthalmics) was presented at the virtual meeting of ASCRS this year. The iTear device is a noninvasive tool that stimulates the trigeminal nerve, resulting in activation of the parasympathetic nerve pathway that controls tear-film homeostasis.
Avoiding Preservatives
“Preservatives are very pro-inflammatory and can, in and of themselves, cause ocular surface disease,” Dr. Weikert notes. He says that moving patients off preserved tear formulations can be key for seeing clinical improvement in their dry eye.
“We see this often in our glaucoma patients,” he says. “These patients are usually on multiple drops for years at a time, so their ocular surface is constantly exposed to preservatives, depending on the type of glaucoma drop they’re on. Using multiple drops over the years can change the chemistry of the tear film on the ocular surface, so it’s not unusual to see significant ocular surface disease in these patients. This type of dry eye can be very difficult to manage because the patient may not be able to switch their glaucoma drops to a preservative-free formula.”
Oftentimes, insurance companies push for generic eye drops. Dr. Weikert notes, however, that most generic drops aren’t typically available in preservative-free formulations and often have harsh preservatives such as benzalkonium chloride, which has consistently demonstrated toxic effects in clinical studies. These effects range from tear-film instability and loss of goblet cells to conjunctival squamous metaplasia and apoptosis.2
Autologous Tears
If artificial tears, steroids and medications aren’t working for a patient, autologous serum tears are another option. “It’s their own immune system working for them,” Dr. Grayson says. “Serum tears can be a pain to get, but they work.”
At the Cullen Eye Institute at Baylor College of Medicine, plasma-based tears are frequently used for patients with severe dry eye. “Serum tears are made from plasma, but it’s plasma without clotting factors,” explains Dr. Weikert. “We’re formulating platelet-rich plasma, which has a higher concentration of platelet factors compared to serum tears, so they have some advantages and carry some additional anti-inflammatory components that can help relieve dry eye.
“There aren’t really any side effects to plasma tears,” he continues. “Cost is an issue because they’re typically not covered by insurance. Sometimes the preparations are off-label, and plasma-based tears require a blood draw, so that’s another cost.” Physicians say the process of making the tears is also time-consuming and complex compared to other dry-eye therapies.
Amnion-derived Drops
Another new type of therapeutic eyedrop in the works is derived from amniotic membrane. “Ocular Science has started making amniotic cytokine extract,” Dr. Weikert says. “Amniotic cytokine extract is another tear form that has components from amniotic membrane, which is pro-anti-inflammatory. The drop form helps replace tears.”
There are currently no FDA-regulated amnion-derived drops available in the United States. Noveome Biotherapeutics (formerly Stemnion; Pittsburgh, Pennsylvania) has an amnion-derived cellular cytokine solution for wound healing and dry eye currently in FDA clinical trials. Barcelona Tissue Bank (Catalonia, Spain) has an internationally available amniotic membrane extract for use in dry eye, and Next Biosciences (Johannesburg, South Africa) has an umbilical cord-derived blood serum for severe dry eye.
Protecting the Surface
For severe cases of dry eye, sometimes a bandage lens is necessary to protect the ocular surface. “We’re proponents of contact lenses,” says Dr. Weikert. “Some scleral lenses also work for keeping a constant layer of fluid against the cornea.”
PROSE (BostonSight) is an ocular prosthesis commonly used for treating severe dry eye. “It’s expensive,” Dr. Weikert cautions, “but it’s been life-changing for certain patients, such as those who are dry from graft-versus-host disease. Those who’ve had leukemia and received bone marrow transplants can sometimes contract this disease. The immune cells from the bone marrow transplant trigger the immune system, which can attack the surface of eye, resulting in significant dry eye.”
Dr. Tyson says he rarely uses scleral lenses for treating dry eye. However, he adds, “I find it’s helpful for conditions like filamentary keratitis, where the cornea needs protection from the eyelid. You can use a bandage lens for that as well as amniotic membrane if it’s severe enough.”
Dr. Weikert adds that amniotic membrane is well-suited to a short treatment to get someone over a significant problem, but in terms of dry eye, he says, “I haven’t come across any literature that demonstrates the efficacy of it in a good clinical trial for prolonged relief of dry eye.”
To Keep in Mind ...
Contracting coronavirus through the ocular surface is a concern. “If you have dry eye, the barrier function of the ocular surface can be decreased,” Dr. Weikert says. “We can’t draw any direct conclusions, but we know dry-eye patients are more susceptible. They may want to consider wearing eye protection in addition to a mask.” REVIEW
Drs. Tyson and Grayson have no financial disclosures related to any of the products mentioned. Dr. Weikert has been a diagnostic equipment consultant for Alcon.
1. Teo CHY, Ong HS, Liu Y, et al. Meibomian gland dysfunction is the primary determinant of dry eye symptoms: Analysis of 2,346 patients. The Ocular Surface 2020;18:4:604-612. [Epub ahead of print].
2. Baudouin C, Labbé A, Liang H, et al. Preservatives in eyedrops: The good, the bad and the ugly. Prog Retin Eye Res 2010; 29:4:312-34.






