This year, ARVO studies shed light on surgical options and their impact, new ways to deliver drugs to the eye, new ways to use familiar tools such as optical coherence tomography and the Amsler grid, and offer new information regarding the impact of lifestyle and systemic factors on intraocular pressure. (Unless otherwise noted, studies received no commercial support.)
Surgical Option Updates
A randomized study conducted at two universities in Ontario and a medical center in Israel compared the rate of visual recovery after implantation of an Ex-PRESS shunt vs. trabeculectomy. Sixty-four subjects with uncontrolled open-angle glaucoma were randomized to Ex-PRESS (n=33) or trabeculectomy (n=31). Best corrected visual acuity was recorded at baseline, day one, weeks one and two, and months one, three, six and 12. All subjects completed three-month follow-up; 58 completed six months and 43 completed one year.
Although no differences in final visual outcomes were found between groups, visual acuity recovered faster in patients receiving the Ex-PRESS. Specifically, in the Ex-PRESS group visual acuity was significantly decreased compared to baseline at day one (p<0.001) and weeks one and two (p=0.002; p=0.02). However, at one month visual acuity was no longer significantly different from baseline (p=0.42) and it remained non-significant at subsequent visits.
In contrast, visual acuity in the tra-beculectomy group remained significantly lower than baseline at each study visit from day one (p<0.001) to one year (p<0.001). At last follow-up, seven subjects in the trabeculectomy group had lost more than two Snellen lines, compared to only two subjects in the Ex-PRESS group.
Reasons for visual acuity loss in the trabeculectomy group included central retinal vein occlusion, vitreomacular traction and cataract (one subject each) and hypotony (three subjects). Reasons for visual acuity loss in the Ex-PRESS group included one subject with hypotony. (No cause for reduced visual acuity could be determined for one additional subject in each group.)5942
|
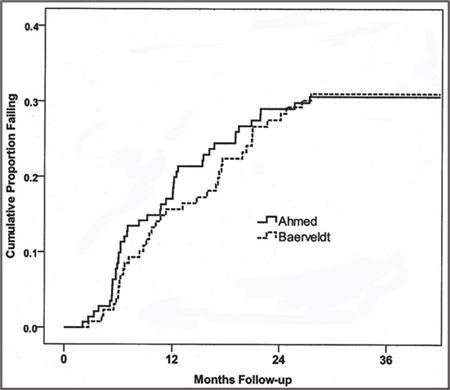
In the study, patients 18 to 85 years of age with an IOP of 18 mmHg or more were randomized to receive either an Ahmed or a Baerveldt implant. The main outcome measures were IOP, visual acuity, use of supplemental medical therapy, complications and failure. Outcomes defined as failure included an IOP greater than 21 mmHg; an IOP not reduced by 20 percent; an IOP less than 5 mmHg; reoperation to treat the glaucoma or remove the implant; and loss of light perception. The data showed:
• Risk of failure was similar for the Ahmed and Baerveldt implants (risk ratio=1, p=0.88, 95 percent CI=0.7, 1.6). (See graph, above.) However, the risk of reoperation for glaucoma was twice as high with the Ahmed implant as with the Baerveldt implant (p=0.074, 95 percent CI=0.9, 4.4).
• At 36 months, mean IOP was 14.3 ±4.9 mmHg in the Ahmed group and 12.9 ±4.4 mmHg in the Baerveldt group (p=0.049).
• The mean number of IOP-lowering medicines was 1.9 ±1.4 in the Ahmed group and 1.5 ±1.4 in the Baerveldt group (p=0.048).
The study authors conclude that there was no difference in failure rates, but the modestly better IOP control seen with the Baerveldt implant compared to the Ahmed implant at the one-year follow-up persisted through three years.6355
A prospective, randomized, double-blinded and placebo-controlled study conducted at multiple sites in Belgium and the Netherlands found that a single intracameral injection of bevacizumab at the end of trabeculectomy improved outcomes. In patients with either primary open-angle glaucoma or normal-tension glaucoma, this protocol was associated with increased absolute success rates, reduced need for postoperative interventions to reach the target IOP, and more diffuse blebs with a lower degree of vascularity.
Between April 2009 and November 2010, 144 consecutive, medically uncontrolled glaucoma patients were divided into POAG and NTG groups. Subjects were randomized to receive 50 µl of either bevacizumab (25 mg/ml) or placebo in the anterior chamber perioperatively. Patients with NTG also received mitomycin-C. Target IOP was between 6 and 18 mmHg for POAG patients and between 6 and 14 mmHg for NTG patients.
Absolute success was defined as meeting the target IOP at the six-month follow-up visit without IOP-lowering medications or postoperative interventions. Qualified success expanded this group to include subjects that met the target IOP at month six with either IOP-lowering medications and/or postoperative surgical interventions. Bleb photographs were taken in 22 patients and graded by two masked observers.
Of the 144 subjects, 141 reached the six-month follow-up point; 70 received bevacizumab and 71 received placebo. The data showed:
• Qualified success was 99 percent in the bevacizumab group versus 94 percent in the placebo group. The difference was not significant (OR 4, CI 0.3 to 201).
• Bleb needlings were significantly less frequent in the bevacizumab group (11 percent) compared to the placebo group (32 percent), p=0.004. Complication rates were comparable.
• The bevacizumab eyes had significantly more diffuse blebs with a lower degree of vascularity at six months: peripheral bleb area (p=0.04); peripheral bleb vascularity (p=0.002) and non-bleb related peripheral bleb vascularity (p=0.01).2505
It’s widely accepted that cataract surgery, in and of itself, causes a modest reduction in IOP, and many believe that this is the result of increased outflow following the surgery. However, one small study found evidence that in some patients with advanced glaucoma, this may not be the case.
In this pilot study, conducted at Duke University Eye Center in Durham, N.C., tonography was used to measure aqueous outflow before and 90 days after cataract surgery in six end-stage glaucoma patients and six normals. Following instillation of proparacaine, patients were accustomed to the probe with three short trials; then, tonography was recorded for at least four minutes and Po/C ratios were calculated.
The initial data revealed that while all control patients had a decrease in the Po/C ratio following cataract surgery, the end-stage glaucoma patients (with one exception) had an increase in Po/C ratio, indicating a decrease in aqueous outflow. This was contrary to the hypothesis of the study authors.
The authors note that this could be a significant consideration when deciding how to manage some glaucoma patients. They look forward to further studies with a larger sample size.1992
Factors Affecting Risk
Recently, evidence has suggested that pseudoexfoliation glaucoma is more prevalent the farther from the equator a population lives. A study conducted at multiple centers in the United States has provided further support that region of residence is an independent risk factor for pseudoexfoliative glaucoma.
|
The data support the supposition that residence in the northern United States may be an independent risk factor for the development of PXF glaucoma. Other types of glaucoma are much more weakly associated with the U.S. region in which individuals live.4462
A study conducted in London, Baltimore and Guangzhou, China, sought to uncover any associations between angle width and weight, height or body mass index in Chinese adults. Subjects aged 50 and over (n=912) were selected via clustered random sampling using a population-based survey in Liwan district, Guangzhou. Angle width was measured using static gonioscopy; BMI was calculated as weight divided by the square of height. Angle occlusion was defined as pigmented trabecular meshwork not visible under static gonioscopy in three quadrants (definition 1) or two quadrants (definition 2). The subjects didn’t differ significantly in gender or refractive status. The data showed:
• In both univariate and multivariate analysis, BMI was the most important predictor for angle occlusion by either definition of angle occlusion.
• Higher weight was independently associated with lower risk for angle occlusion, and the association remained significant after adjusting for age and gender. (The association between height and angle occlusion was no longer significant after adjusting for age, gender and axial length.)4471
A study conducted at the University of California, San Francisco and Stanford University found a correlation between high supplemental consumption of calcium and iron and glaucoma. The cross-sectional study included data from 3,848 individuals at least 40 years old that participated in the National Health and Nutrition Examination Survey between 2007 and 2008, who specified whether or not they had glaucoma. Participants had been interviewed about their use of dietary supplements and antacids during the prior 30-day period.
The data indicated that participants who consumed at least 800 mg/day of supplementary calcium, or at least 18 mg/day of supplementary iron, had significantly higher odds of self-reported glaucoma compared to no consumption of supplementary calcium or iron. This was after adjustment for demographic characteristics, health-related behaviors, comorbidities and general health condition (OR 2.44, 95 percent CI 1.25 to 4.76 for calcium; OR 3.80, 95 percent CI 1.79 to 8.06 for iron). These nutrient intake levels were equivalent to the highest quintile of calcium intake and the highest two quintiles of iron intake reported in this population.
The study authors hypothesize that because they found that only those with the highest quintiles of supplementary calcium and iron consumption had significantly greater odds of glaucoma, there may be a threshold intake of these oxidants above which there is an increased risk of glaucoma. They note that further research is needed to elucidate potential biological mechanisms that might explain the association, and to determine whether high supplement levels correlate with glaucoma progression.4623
Detecting and Following Disease
A study conducted at Dalhousie University in Nova Scotia and Devers Eye Institute in Portland, Ore., tested the diagnostic capability of a new parameter for use when diagnosing glaucoma via SD-OCT.
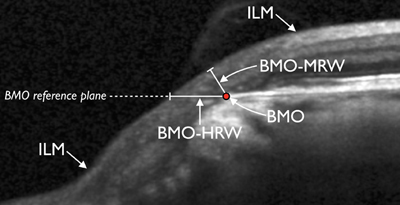
The study authors note that rim assessment based on the clinical disc margin (DM) lacks a solid anatomical basis, for two reasons. 1: The DM is not a reliable outer border of rim tissue because of clinically and photographically invisible extensions of Bruch’s membrane inside the DM; and 2: Rim tissue orientation in the optic nerve head is not taken into account. To surmount these problems, the authors introduced a new parameter: BM opening-minimum rim width (BMO-MRW). (See example, below.) This parameter quantifies the rim from its true anatomical outer border while also accounting for its variable trajectory in the measurement plane.
|
• In controls, BMO-MRW was significantly more correlated to BMO area than the current method (r=-0.46 vs. r=-0.07, p<0.01).
• Global BMO-MRW had consistently higher discrimination than the global current method. At 95 percent specificity, the sensitivity of BMO-MRW was 83 percent; the sensitivity of BMO-HRW was 25 percent. (Both Moorfields regression analyses performed substantially worse.)
The authors conclude that the more than threefold higher sensitivity of BMO-MRW in early glaucoma at 95-percent specificity, compared to current methods, is clinically significant and supports the use of the new structural marker for the detection and risk-profiling of glaucoma.1745
In a prospective cohort study supported by the American Glaucoma Society, Harvard and Pfizer, researchers at three centers in the United States sought to identify the best correlations between visual field defects and SD-OCT structural measurements based on glaucoma severity.
Patients with glaucoma, glaucoma suspects and normal subjects were recruited at two academic centers. Researchers obtained Humphrey visual fields and SD-OCT thickness measurements of the full retina in the macula, the ganglion cell complex and the peripapillary retinal nerve fiber layer. (All structural measurements were normalized for age.) The visual field tests were used to determine the presence and severity of glaucoma based on a previously published Glaucoma Staging System.
After excluding unreliable visual field tests and SD-OCT scans with imaging artifacts, results from 158 eyes were analyzed. Statistically significant correlations were found in the overall group between visual field mean deviation and each of the structural measurements (p<0.01). Further analysis of the structure-function relationship by glaucoma severity revealed that the correlations were slightly stronger in no-glaucoma and moderate-glaucoma groups, when full macular thickness or GCC was used as the structural measure. When the RNFL was used, better correlations were found in no-glaucoma and early-glaucoma groups.
The authors conclude that the strength and character of the structure-function relationship depend on the severity of glaucoma.714
Researchers at four centers in New York state set out to discover whether the Amsler grid could be as effective as 10-2 standard automated perimetry for evaluating central visual field defects in glaucoma. Ninety-six eyes of 48 glaucoma patients were included in the study. Subjects had had either a normal or abnormal 10-2 visual field within the previous four months for both eyes. An abnormal field was defined as having at least three adjacent points at p<0.05 and at least one point p<0.01. (Eyes with known macular disease were excluded.)
| |||
• The 10-2 MD, 10-2 scotoma extent and 10-2 scotoma mean depth were significantly correlated with the Amsler grid scotoma area—all p<0.001.
• The Amsler grid appeared to be more useful in detecting moderate to severe 10-2 VF defects.
The authors conclude that the results of the Amsler grid tests approximate the 10-2 visual field results. The Amsler grid may be a useful supplement to 10-2 visual field testing for evaluating and monitoring central VF loss in glaucoma.177
Advances in Drug Delivery
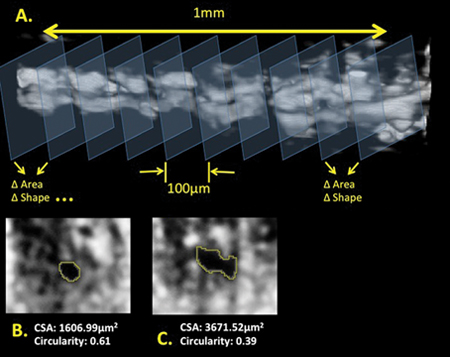
Researchers at the University of Pittsburgh have developed a new way to deliver controlled-release brimonidine tartrate to the eye without the use of drops. This was accomplished through the fabrication of microparticles (7.5 ±2.9 μm in diameter) from polylactic-co-glycolic acid.
To test the microparticles’ effectiveness, studies were conducted in vivo and in vitro. In vitro release of BT was quantified by incubating a known mass of microparticles in buffer and measuring the absorption. For the in vivo studies, healthy rabbits were randomized to receive microparticles containing no drug, BT-loaded microparticles, or BT drops (Alphagan). Rabbits in both microparticle groups received subconjunctival injection of microparticles suspended in sterile saline on day 0 in one eye.
In the in vitro experiment, the microparticles released an average of 0.62 ±0.34 μg BT/mg particles per day. In the in vivo study the decrease in IOP was significantly less (p<0.05) in the eyes treated with BT drops than in eyes receiving BT microparticles, at all time points. Histological analysis showed no signs of foreign body response to the microparticles.
The authors note that the BT-loaded microparticles delivered more than 28 days of therapeutic levels of BT with a single dose; they effectively reduced IOP with no evidence of irritation or infection. They are currently adapting the microparticle formulation into a clinically relevant dosage form that patients can easily apply, which they will be testing in a rabbit model.1750
Researchers at two universities in Japan tested the IOP-reducing ability and safety of a new drug-delivery system they developed—a latanoprost-binding bio-nanosheet (LBNS). The multi-layered LBNS is composed of layered sheets of chitosan and sodium alginate, created with a process involving polyvinyl alcohol and imbued with latanoprost isopropyl ester. Thickness of the LBNS is approximately 200 nm. LBNSs were placed on the corneas of a small number of rats. The data showed:
• The smallest concentration LBNS, 0.25 μg/cm2, only showed a significant IOP reduction for one day after application. The higher concentrations, 2.5 μg/cm2 and 25 μg/cm2, significantly reduced IOP for seven days.
• IOP reduction rates for the 2.5 μg/cm2 LNBS, at days one, two, four, seven and nine were -27 ±14.8, -22 ±16.7, -25.8 ±18, -22.7 ±20.9, and -6.6 ±17 percent, respectively. Latanoprost in the aqueous humor was detected up to seven days after application.
• Although the 25 μg/cm2 LBNS showed transient hyperemia, other concentrations showed no topical adverse effects throughout the experiment.
Noting that a single application of LBNS on the cornea significantly reduced IOP for up to seven days without severe local complications, the authors propose that LBNS may be a good candidate for a new anti-glaucoma drug delivery device.5017
Systemic and Lifestyle Factors
A retrospective study conducted at Yonsei University in Seoul, South Korea, sought to determine the association between systemic antihypertensive medications and visual field progression in open-angle glaucoma.
Researchers reviewed the charts of 552 OAG patients who had visited their clinics between 2003 and 2007. Eighty patients with five or more reliable Humphrey visual field tests were included in the study.
Subjects with POAG (IOP of 22 mmHg or more) showed a higher progression rate than normal tension glaucoma subjects (IOP of less than 22 mmHg): MD, -0.73 vs. -0.52 dB/year; VFI, -1.95 percent/year vs. -1.05 percent/year. Most notably, POAG patients using antihypertensive medication showed a statistically significant higher rate of progression than those not taking antihypertensive medication: MD, -1.45 dB/year vs. -0.46 dB/year; VFI, -3.27 percent/year vs. -1.47 percent/year.
The authors conclude that systemic antihypertensive medication may be a significant risk factor for a higher rate of visual field progression, especially in conjunction with high IOP status.230
Two researchers at the University of Montreal conducted a meta-analysis of more than 40 years’ worth of studies relating to the impact of aerobic exercise on POAG in order to assess the effects of exercise intensity and duration on IOP.
After reviewing 63 POAG-and-exercise-related studies, the authors selected 10 studies that included sedentary or normally active participants with a normal baseline IOP (10 to 21 mmHg) who completed a single session of mild (40 percent increase in heart rate) to moderate (50 to 70 percent increase in heart rate) aerobic exercise, ranging from two to 60 minutes in duration.
The data revealed a clear effect of exercise, showing a 1- to 5-mmHg reduction in IOP across conditions. Because of the diverse nature of the studies, the authors were unable to compute a global effect size. However, they observed certain patterns in the results:
• There was an almost twofold greater reduction in IOP when exercise was moderate intensity rather than mild intensity.
• The duration of the exercise did not appear to influence the outcome when the exercise was of moderate intensity; however, it did influence the outcome when the exercise was only of mild intensity.
The authors note that the reduction in IOP as a result of exercise is within the range that would be most useful to those at risk of POAG. Prescribing even a mild daily aerobic exercise regime could be an effective way to keep slightly elevated IOP levels within a normal range.5070 REVIEW
Dr. Netland is professor and chairman of the department of ophthalmology at the University of Virginia; Dr. Singh is professor of ophthalmology and director of the Glaucoma Service at Stanford University School of Medicine.