Though it may have taken surgeons a little while to get a feel for presbyopic intraocular lenses and how they could fit into their practices, many of the physicians on our National Panel say they’re pleased with the results they get from these lenses and use them regularly. They also continue to use toric lenses and give them high marks, but they still haven’t fully embraced phakic IOLs.
These are some of the results from our latest National Panel survey. This month, 30 physicians (6 percent) of our 500-physician panel responded with their thoughts on intraocular lenses.
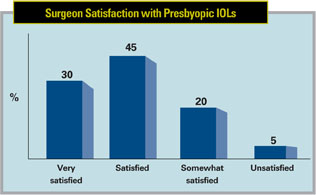 |
Sixty-seven percent of the surgeons say they use some kind of presbyopic lens, be it diffractive, multifocal or pseudo-accommodative. Thirty percent of the presbyopic lens users are very satisfied with their lens of choice, and 45 percent say they’re just satisfied. Only 20 percent say they’re somewhat satisfied, and 5 percent are unsatisfied.
In terms of the lenses that the surgeons implant (they could choose more than one type), 38 percent implant the ReSTOR +3 D lens, 28 percent implant the Tecnis multifocal, 23 percent use the Crystalens AO, 8 percent implant the previous-generation ReSTOR +4 D and 3 percent implant the AMO ReZoom.
Richard Margolies, MD, of Palm Beach Gardens, Fla., says he’s satisfied with the AcrySof ReSTOR +3 D lens. He adds, however, “Rarely—but annoyingly—there’s a glare or halo effect. I’d love to see it reduced.” A surgeon from California’s lens of choice is the Crystalens AO, with which he says he’s somewhat satisfied. “It works great in some people, less so in others,” he adds. An Indiana ophthalmologist and Tecnis multifocal user says, “I have used all of the available presbyopic lenses, and patient satisfaction seems the highest with the Tecnis multifocal.”
Looking ahead, presbyopic lenses appear to have a bright future, as well. Half of the surgeons who don’t currently use a presbyopic lens say they’re somewhat likely to adopt them, and 10 percent say they’re very likely to do so. A fifth of the respondents say that they’re unlikely and 10 percent report that they are very unlikely to start using any kind of presbyopic lens.
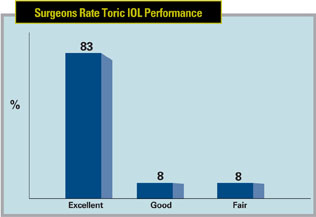 |
Toric IOLs continue to be popular with respondents, with 89 percent of them saying they’ve implanted a toric lens. Eight-three percent of toric users report the lenses’ performance and outcomes as excellent.
“They are a great advance in cataract surgery,” declares a surgeon from Wisconsin. Douglas Liva, MD, of Paramus, N.J., agrees, saying, “The toric IOL is the only premium IOL that consistently meets expectations.” Dr. Margolies says the AcrySof toric lens is his preferred IOL. “It gives exceedingly high patient satisfaction due to a reduction in the conoid of Sturm and superb centration,” he says. “It also has minimal postop shifting.” Robert Green Jr., MD, of San Antonio thinks toric lenses are excellent, and says, “I’ve only had one patient with unwanted images from a point source of light.” A surgeon from Indiana isn’t as quick to heap praise on toric lenses, though. In his experience, he says they only give “partial correction and lackluster performance for a high cost.”
IOLs in General
Of the monofocal lenses recently introduced to the market, aspheric lenses are the most popular variety with the panel’s respondents, being chosen by 90 percent of the surgeons. Specifically, 64 percent use the Alcon aspheric SN60WF, 15 percent use the AMO Tecnis (including the foldable version) and 11 percent prefer the Bausch + Lomb SofPort AO.
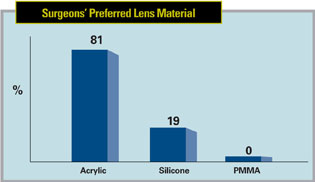 |
When it comes to a preference for lens material, acrylic still sits atop the rankings, with 81 percent of the surgeons choosing it. Silicone was chosen by the remaining 19 percent. Several surgeons like acrylic’s compatibility. “It’s compatible with all patients,” avers a surgeon from Wisconsin, “including diabetics. I also like it because it’s foldable.” A New York surgeon says he prefers acrylic on the off chance there will be “retinal detachment repair with silicone oil” needed in the future. A surgeon from Arizona says an acrylic lens is “soft, involves low inflammation and is easy to insert.” Dr. Margolies likes silicone’s “flexibility, clarity and ease of insertion.”
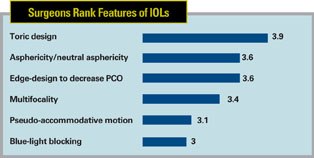 |
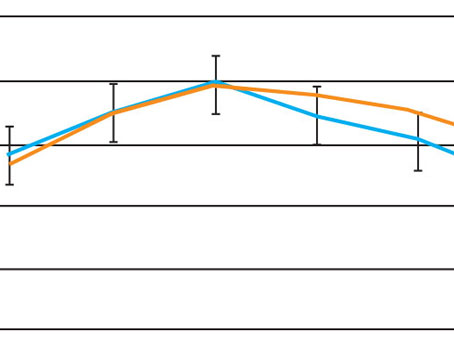
| Surgeons ranked IOL attributes from 6 (most valuable) to 1 (least valuable). Shown here is the average score for each lens attribute from the survey. |
Phakic Foibles
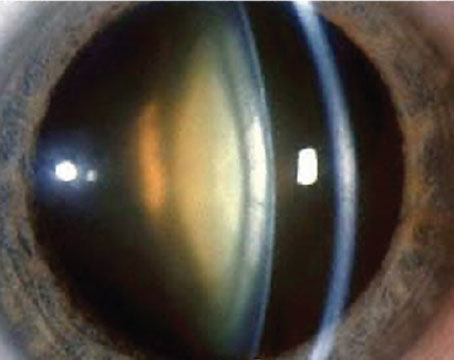
The surgeons on our panel aren’t as interested in implanting a lens in a phakic patient, with only 11 percent reporting that they use phakic lenses. This has the potential to change, however, with a 50/50 split in surgeons who are interested or not interested in implanting phakic lenses sometime in the next two years. “Results are good, but complications are high,” opines a surgeon from Indiana. An Iowa surgeon thinks phakic lenses may be the wave of the future, saying, “The need for them seems to be increasing.” Dr. Margolies feels similarly, saying, “Adjunctive therapies increase our armamentarium for treating refractive errors.” A surgeon from Maryland no longer implants phakic lenses, perhaps due to a complication she experienced. “I used to implant them,” she says. “I got great results but also got one cataract.” A couple of surgeons, however, don’t think phakic lenses are a good option. “The risks outweigh the benefits,” claims a surgeon from Wisconsin. “There’s no real way to measure and match the sulcus diameter,” declares a surgeon from Indiana. San Antonio’s Dr. Green says he’s not interested in them at all, adding, “They’re dangerous. I think the patients with these lenses will develop cataracts.”
Lens Problems
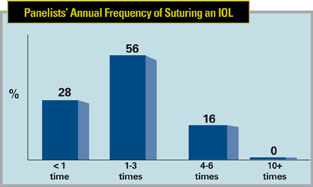
Sometimes, cataract procedures don’t proceed as planned in the operating room, and the surgeon may need to suture an IOL in place or explant one entirely. Surgeons shared their experience with these undesirable situations.
In our survey, 56 percent of the surgeons say they’ve had to suture one to three lenses per year, and 16 percent say they usually have to suture four to six of them. Twenty-eight percent, though, encounter this less than once a year. Some of the reasons the surgeons sutured the lenses include:
- late subluxation of the IOL and bag;
- dislocation;
- referral from another surgeon, with the lens ultimately being sutured to either the iris or the sclera; and
- zonular insufficiency, ultimately fixated with transscleral sutures.
 |
- IOL power errors;
- a patient intolerant of a multifocal lens;
- dysphotopsia;
- poor capsular support;
- late dislocation of the IOL and bag;
- a previous refractive surgery pa--tient with a tricky IOL power calculation;
- a single-piece lens left in the sulcus;
- glare and halo complaints; and
- a malpositioned lens.