Our patients look to us for evidence-based information about these substances. Here, I’d like to review a little bit of what the studies to date have shown, to offer some guidance regarding what you might want to say to your patients when these questions arise.
The Value of Vitamins
It’s not unreasonable to believe that supplements such as vitamins could impact the progression of glaucoma. Doctors dealing with age-related macular degeneration have already demonstrated the potential of this approach. As we all know, the Age- Related Eye Disease Study found that a combination of antioxidants and zinc was able to reduce the progression of disease in macular degeneration patients with intermediate and large drusen by 25 percent,1 so it is possible to find something in the world of complementary and alternative medi-cine that can help address eye disease. In glaucoma, we just haven’t yet found the perfect mixture. The reason for that may be, in part, that glaucoma is actually a cluster of related diseases. Treating it may ultimately involve addressing both pressure issues and neuroprotective issues.
Vitamin supplements that have been posited to have an effect on glaucoma include B1, B3, B12, C, A and E. The chart on the facing page shows some of the studies, pro and con, concerning five of the most commonly taken vitamins. Notably, the results of different studies are often contradictory.
A few observations:
• Vitamin B1 (thiamine). Edward Asregadoo, MD, theorized that B1-deficient patients might be more prone to glaucoma. He noted that low levels of vitamin B1 are associated with increased cortisol, which in turn increases IOP. A study he published did find lower serum thiamine in glaucoma patients.2 However, vitamin B1 didn’t significantly lower IOP, and unfortunately, the study wasn’t well-designed. Other evidence suggests that B1 levels may not impact glau-coma; alcoholics, for example, tend to be deficient in vitamin B1, but there’s no correlation between alcoholism and glaucoma.
• Vitamin C. The evidence for vitamin C’s impact on glaucoma is mixed. One study found that intra-venous vitamin C lowered IOP 20 percent over two hours; it does appear to have a significant osmotic effect, similar to mannitol.3 However, IOP climbs back up over 10 to 12 hours, and it’s not really practical to give someone IV vitamin injections. Other studies, looking at vitamin C supplements, didn’t show much of a change in pressure.4,5 And while vitamin C has a benign reputation, it can cause kidney stones and gastrointestinal upset, and it should be avoided in those with a glucose-6-phosphate dehydrogenase (G6PD) deficiency, B-thalassemia or hemochromatosis.
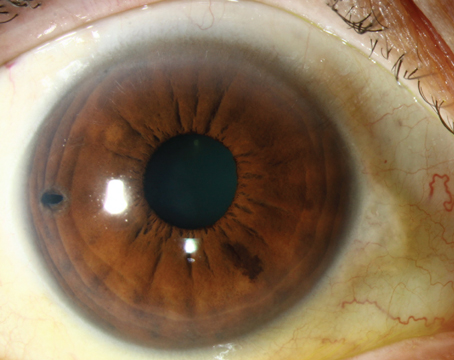
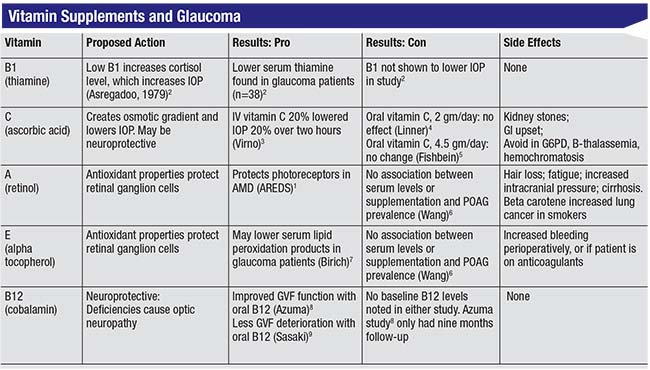 |
• Vitamin A (retinol). As an anti-oxidant, vitamin A might be expected to protect retinal ganglion cells, and the AREDS study did find evidence that it protects photoreceptors in macular degeneration patients. However, a study by Sophia Wang, MD, found no association between vitamin A supplementation or serum levels and primary open-angle glau-coma prevalence.6 Meanwhile, retinol can have side effects including hair loss, fatigue, increased intracranial pressure and cirrhosis.
• Vitamin E (alpha tocopheral). Vitamin E does have antioxidant properties, and one study found that it may lower peroxidation products in glaucoma patients.7 However, the previously mentioned study by Dr. Wang6 found no association between vitamin E and glaucoma prevalence, and vitamin E can potentially cause increased bleeding perioperatively, as well as in patients already taking an anticoagulant.
• Vitamin B12 (cobalamin). B12 is neuroprotective, and we know that deficiencies in B12 are associated with optic neuropathy. Two studies found visual field improvement with vitamin B12 supplementation,8,9 but no baseline B12 levels were done in these studies, and they had very short follow-up.
Other supplements have produced interesting results in animals and in in vitro studies. Vitamin B3 (nicotina-mide), for example, may be neuro-protective. One animal study reported in Science10 found that vitamin B3 could help to mitigate mitochondrial dysfunction, which has been linked to retinal ganglion cell damage and death. In this study, mice were fed a supplement equivalent to 2.5 grams a day in humans; it prevented the structural and functional loss of ganglion cells and nerve axons, and the effect persisted, even with elevated pressure. Furthermore, intravitreal injections of a gene that produces nicotinamide protected 70 percent of mice from glaucomatous damage for 12 months. In addition, combining the two approaches provided more protection than either one alone. So in vitamin B3 we have the potential for an agent that not only has a neuroprotective effect but can also continue having that protective effect in the presence of elevated pressure. The idea that nicotinamide may have beneficial effects has been proposed for further investigation in humans.11 So far, however, this has only been shown in animal studies.
 |
One of the main problems with vitamin studies is that studies tend to involve very small numbers of patients, and a lot of the reports have been anecdotal. The reality is that since the U.S. Food and Drug Admin-istration doesn’t need to approve any of these agents, there’s no incentive for large studies to be conducted, the way there might be with drugs that need FDA approval. As a result, very few large, controlled studies have been done.
There’s also another significant problem: Many of these studies are done in vitro, where, for example, the agent may protect ganglion cells.
But when a person ingests a supplement, it has to go through all of the metabolic processes in the body, so the potency could be significantly diminished by the time it gets to the nerve cells. That makes it difficult to know what the proper dose should be for humans.
Other Supplements & Nutrients
The problem of potency following ingestion is an issue with two non-vitamin supplements that have shown promise with glaucoma: co-enzyme Q and resveratrol. These have been shown to reduce mito-chondrial susceptibility in vitro, and I believe they show promise for neuro-protection.
One study found that topical micelles of co-enzyme Q10 with vita-min E d-a-tocopheryl polyethylene glycol 1000 succinate, twice a day, significantly reduced the number of apoptotic retinal ganglion cells three weeks after induction of ocular hypertension. Furthermore, the effect was independent of IOP.12 Another study found that resveratrol retarded apoptosis of RGS’s in vitro and decreased the level of caspace-3 (a marker of apoptotic events), while stimulating increased quantities of mitochondria.13 Unfortunately, when a person ingests co-enzyme Q or resveratrol in supplement form, the efficacy may be dramatically altered by the metabolizing process. Clinical trials in humans could do a lot to pin down the quantities and con-centrations required to produce simi-lar effects in our patients.
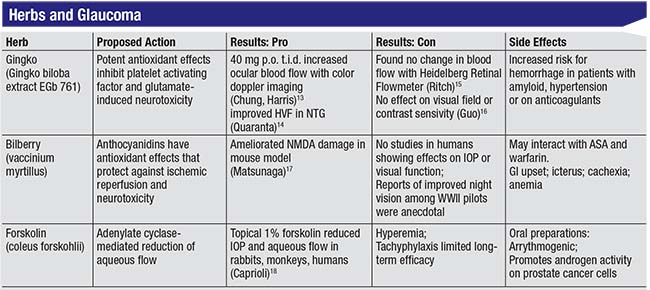
A few herbal supplements are also believed to have positive effects on the eyes and glaucoma. The chart above shows some of the data relating to three popular herbal supplements that sources on the Internet claim will help treat glaucoma.
A few observations about these three herbal supplements:
• Gingko biloba. This is a well-known antioxidant used widely in Europe to treat breathing problems and Reynaud’s phenomenon, which is a vascular disorder. Gingko is known to inhibit glutamate cytotoxicity, which leads to ganglion cell death, and it’s been shown to increase blood flow.14,15 However, these were very small studies, and there were a couple of contrasting studies that found no effect on visual field or contrast sensitivity, as well as one that found no change in blood flow.16,17 One of the challenges when studying gingko’s effect on blood flow is that we still don’t have agreement on the best way to measure ocular blood flow, making it difficult to draw any conclusions about how helpful gingko actually may be.
One other important consideration when suggesting that a patient try gingko: Gingko increases the risk of bleeding. For that reason, you have to make sure your patient is not on warfarin, aspirin or any other blood thinners, because your patient could be prone to getting pretty severe hemorrhages.
• Bilberry (vaccinium myrtillus). The bilberry plant is a cousin of the blueberry. In World War II, fighter pilots took bilberry to increase their night vision, but to date, no study has been done to confirm that this effect is real. As an anthocyanidin, bilberry has a very potent antioxidant effect that can protect against ischemic reperfusion and neurotoxicity, and it’s been shown to decrease retinal ganglion cell damage in a mouse model.18 However, no studies in hu-mans have shown any effect on IOP or visual function. Bilberry can also interact with aspirin and warfarin and potentiate bleeding; and it has been associated with gastrointestinal upset, icterus, cachexia and anemia.
• Forskolin (coleus forskohlii). This herb has been shown to lower IOP in rabbits, monkeys and humans by reducing aqueous flow. This was first demonstrated back in the mid-1980s.19,20 However, further studies were abandoned because forskolin caused significant hyperemia and tachyphylaxis. Furthermore, after a month or two the pressure would shoot back up, so there wasn’t a lot of long-term promise. Oral preparations are available, but when you take forskolin orally it doesn’t have any effect on IOP. Downsides include that forskolin is arrythmogenic, and it can promote androgen activity on prostate cells in patients with prostate cancer.
Some nutrient-rich foods show promise for impacting glaucoma progression. The Osteoporotic Fractures Research Group found that patients who ate three or more servings of fruit such as peaches or oranges, or fruit juices, per day were 79 percent less likely to have POAG. In addition, those who ate more than one serving of collard greens or kale, which are nitrate-rich, leafy green vegetables, per week decreased their odds of having POAG by 57 percent.21,22 The Nurses Health Study and Health Pro-fessionals Follow-up Study found that a greater intake of nitrate-rich foods and leafy green vegetables decreased the risk of POAG by 20 to 30 percent.23 These are large, well-designed population studies. Gran-ted, they were large cohort studies that relied on statistical analysis, and the data was based upon patient self-reporting, so they could contain an element of bias. It’s also possible that individuals eating large quantities of these foods may have a healthier lifestyle overall, and that might be contributing to their reduced POAG. Nevertheless, the statistics are pretty impressive.
One of the take-home messages here is that although we often hope to get relief from supplements in pill form, there may be an advantage to ingesting beneficial nutrients in their natural dietary form. Other pro-nutrients in these vegetables and fruits may also be contributing protective effects.
Medical Marijuana
The herb patients most often ask about, not surprisingly, is marijuana. Medical marijuana is currently legal in 30 states, including the District of Columbia, and recreational marijuana is legal in a handful of states, most recently California (as of January 1, 2018). The interesting thing about marijuana is that it’s a Schedule I con-trolled substance, while
 |
| Although early studies suggested that marijuana may reduce IOP for a few hours, a host of side effects and practical concerns make its use as a glaucoma treatment controversial at best. |
The original studies on marijuana were done back in the 1970s.24 Those studies, using a small sample of participants, showed a significant reduction in IOP (25 to 30 percent) in 65 percent of patients. However, participants’ eyes got red, tear production decreased, pupils got smaller, and the decrease in pressure only lasted three to four hours. It’s also difficult to evaluate these studies relative to today’s marijuana use because marijuana potency is difficult to verify. In the early studies, individuals were smoking 2% marijuana cigarettes; today the concentration of THC in a marijuana cigarette may be much higher.
A few years later, Keith Green, PhD, did similar studies using oral ingestion (e.g., eating marijuana brownies).25 The results were mixed; in some patients this lowered IOP, but in others it didn’t. In any case, oral ingestion requires larger quantities of the drug to produce the same effect, which makes sense because the drug is being taken in through the gastrointestinal tract where it must be metabolized by the liver, etc. That’s going to decrease the potency and availability of any active compounds.
Of course, marijuana can have numerous side effects. These include ocular side effects such as conjunctival hyperemia, decreased lacrimation, diplopia, impaired accommodation, photophobia, nystagmus and bleph-arospasm. Systemic side effects in the short term may include increased pulse, orthostatic hypotension, and of course, euphoria.26 Over the long term, side effects may include emphy-sema-like lung changes, decreased immune function, decreased cognitive function and potential alterations in the growth of a fetus. (It would be helpful to conduct long-term studies, but as long as marijuana remains a Schedule I agent, that’s unlikely to happen.)
Encouraging patients to smoke marijuana to address glaucoma is controversial at best. Smoking inher-ently carries some risk for emphysema and lung cancer, along with the other aforementioned side effects. The orthostatic hypotension issue may also be significant, because of the likelihood that the drug is decreasing blood flow to the optic nerve, which could be damaging. The CNS side effects are problematic, especially for older patients. Moreover, current topical medications usually have a better efficacy profile for lowering IOP. For all of these reasons, both the American Academy of Ophthalmology and the American Glaucoma Society currently do not recommend the use of marijuana to treat glaucoma.
A promising approach in the future may be the use of cannabinoids, the active compounds found in mari-juana, which are receiving research attention. Cannabinoids such as delta9-THC and cannabidiol have been shown to decrease IOP; they act on cannabinoid receptors in the trabecular meshwork and increase aqueous outflow, and they also have neuroprotective qualities. One study of WIN55212-2 found that it decreased IOP 20 to 30 percent, achieving maximum effect within 60 minutes, although the effect did not last long.27
Some more recent research involving THC prodrugs such as THC-Val-HS has been more promising. Coupling the drug with cyclodextrins and surfactants helps to increase solubility, so there’s more availability and better penetration through the cornea. In a rabbit model this produced a better IOP lowering than timolol, although it had a shorter duration of action, similar to pilocarpine.28
The main point is, while smoking marijuana isn’t something that we as ophthalmologists currently stand behind, cannabinoid agents may have the potential for ocular penetration without the potential for side effects such as orthostatic hypotension and euphoria. In the meantime, the potential for benefits from the occasional adjunctive use of marijuana in addition to prescribed glaucoma treatment regimens, and the effects of marijuana in glaucoma patients who regularly use it for nonmedical reasons, have not been investigated.
Managing Patient Questions
Patients ask me about smoking marijuana all the time; they want me to prescribe it for them. If you haven’t already encountered this, you probably will.
Here are a few strategies that may help you manage this situation when it arises:
• Be aware of the marijuana laws in your state. Use of marijuana, even for medical reasons, is subject to law. To keep yourself and your patients out of trouble, do your homework about the legal ramifications in your state.
• Be ready with an answer be-fore your patients ask questions. I explain to my patients that so far it’s not clearly defined how marijuana should be used to treat glaucoma. Even though it’s approved for glaucoma treatment here in Florida, there are no guidelines. In addition, the American Academy of Ophthalmology and American Glaucoma Society do not advocate its use for treating glaucoma. For these reasons—among others—the majority of doctors I know won’t prescribe it. (I don’t, either.)
• Educate and inform interested patients regarding the efficacy, side effects and drug interactions associated with marijuana use. Most interested patients have little, if any, idea about this aspect of marijuana use. It’s worth pointing out that while marijuana may lower IOP in the short term, in the long term it may do them more harm than good.
• Consider prescribing an oral cannabinoid like Marinol (dronabinol) instead. Marinol has been used for decades in cancer patients to treat nausea and other gastrointestinal side effects of chemotherapy. The few times I’ve prescribed it for patients, it’s had a modest effect on IOP, lowering it 10 to 15 percent. Notably, it appears that it’s not completely free of the euphoric effects. Some patients complain that they still experience effects such as lightheadedness or confusion—while other patients are not bothered at all. (Hopefully the research into topical cannabinoids will bear fruit, thus taking any systemic side effects off the table.)
Playing It Safe
Given the popularity of supplements and marijuana today, it’s essential that we be prepared to help our patients navigate the rational use of these substances. We have to be ready to educate patients on their efficacy and side effects. A few points worth making:
• Patients should be careful with any of these supplements because even if they may potentially help, no one knows the proper dosage. The reality is, these treatment possibilities haven’t been seriously studied, so we’re making choices based on minimal information.
• Be careful about the purity of the substance in question. Many herbs are sold mixed with other herbs, and some individuals can have pretty dramatic side effects from those additional herbs.
• Do your homework before proceeding. Your patients should talk to their internist if they’re planning on using supplements, to make sure they don’t interact with any prescription drugs they may be taking. Some supplements will interact with blood thinners, or may exacerbate other problems like prostate cancer or gastrointestinal issues. While some supplements may be helpful, they are not totally benign.
• Encourage a healthy diet with antioxidant and nitrate-rich foods including citrus fruits, peaches, salad, kale and collard greens. These foods not only limit the possibility of side effects, they have some of the most impressive supporting evidence in the literature. Citing some of the statistics found in the research may surprise and impress your patients. REVIEW
Dr. Gamell is an associate professor of ophthalmology at the University of South Florida Health Morsani College of Medicine, and Glaucoma Fellowship Director at the USF Eye Institute in Tampa.
1. Age Related Eye Disease Study Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol 2001;119:10:1417-1436.
2. Asregadoo ER. Blood levels of thiamine and ascorbic acid in chronic open-angle glaucoma. Ann Ophthalmol 1979;11:1095–1100.
3. Virno M, Bucci MG, et al. Intravenous glycerol-vitamin C (sodium salt) as osmotic agents to reduce intraocular pressure. Am J Ophthalmol 1966;62:824–833.
4. Linner E. The pressure lowering effect of ascorbic acid in ocular hypertension. Acta Ophthalmol (Copenh) 1969;47:685–689.
5. Fishbein SL, Goodstein S. The pressure lowering effect of ascorbic acid. Ann Ophthalmol 1972;4:487–491.
6. Wang SY, et al. Glaucoma Vitamins A, C, and E supplement intake and serum levels in a population-based sample of the United States. Eye 2013; 27:4:487-494.
7. Birich TV, Birich TA, Marchenko LN: [Vitamin E in multiple-modality treatment of primary glaucoma patients]. Vestn Oftalmol 1984;102:10–3.
8. Azumi I, Kosaki H, Nakatani H. Effects of metcobolamin (Methycobal) on the visual field of chronic glaucoma—a multicenter open study. Folia Ophthalmol Jpn 1983;34:873–878.
9. Sasaki T, Murata M, Amemiya T. Effect of long-term treatment of glaucoma with vitamin B-12. Glaucoma 1992;14:167–170.
10. Williams PA, et al. Vitamin B3 modulates mitochondrial vulnerability and prevents glaucoma in aged mice. Science 2017;355:756-760.
11. Williams PA, Harder JM, John SW. Glaucoma as a metabolic optic neuropathy: Making the case for nicotinamide treatment in glaucoma. J Glaucoma 2017;26;12;1161-68.
12. Davis BM, et al. Topical Coenzyme Q10 demonstrates mitochondrial-mediated neuroprotection in a rodent model of ocular hypertension. Mitochondrion 2017; 36: 114-123.
13. LiuXQ, Chen MM, et al. Resveratrol Mitigates Rat Retinal Ischemic Injury: The roles of matrix metalloproteinase-9, inducible nitric oxide, and heme oxygenase-1. Jour Oc Pharm Ther 2013;29:1:33-40.
14. Chung HS, Harris A, et al. Ginkgo biloba extract increases ocular blood flow velocity. J Ocul Pharmacol Ther 1999;15:3:233-40.
15. Quaranta LR, et al. Ginkgo biloba extract improves visual field damage in some patients affected by normal-tension glaucoma. Invest Ophth Vis Sci 2014;55:2417.
16. Gurses-Ozden R, Harris A, et al. Ginkgo biloba extract does not alter peripapillary retinal hemodynamics using Heidelberg Retina Flowmetry in open-angle glaucoma. Invest Ophthalmol Vis Sci 2002:42(Suppl)
17. Guo X, et al. Author Response: Effect of Ginkgo biloba on visual field and contrast sensitivity with NTG in Chinese patients: A randomized, crossover clinical trial. Invest Ophth Vis Sci 2014;55:110-116.
18. Matsunaga N, et al. Bilberry and its main constituents have neuroprotective effects against retinal neuronal damage in vitro and in vivo. Mol Nut Food Res 2009;53:7:869-77.
19. Caprioli J and Sears M. Forskolin lowers intraocular pressure in rabbits, monkeys, and man. Lancet 1983;1:958-960.
20. Caprioli J, et al. Forskolin lowers Intraocular pressure by reducing aqueous inflow. Inves Ophthalmol Vis Sci 1984;25:268-277.
21. Coleman AL, Stone KL, Kodjebacheva G, et al. Glaucoma risk and the consumption of fruits and vegetables among older women in the study of osteoporotic fractures. Am J Ophthalmol 2008;145:6:1081–1089.
22. Giaconi JA, et al. The association of consumption of fruits/vegetables with decreased risk of glaucoma among older African–American women in the study of osteoporotic fractures. Amer J Ophthal 2012;154:4:635-644.
23. Kang, JH, et al. Association of dietary nitrate intake with primary open-angle glaucoma, a prospective analysis from the Nurses’ Health Study and Health Professionals Follow-up Study. JAMA Ophthalmology 2016;13:3:294-303.
24. Hepler RS, Frank IR. Marihuana smoking and intraocular pressure. JAMA 1971;217:1392.
25. Green K. Marjuana smoking vs cannabinoids for glaucoma therapy. Arch Ophthalmol 1998;116:1433-1437.
26. Merritt JC, et al. Effect of marijuana on intraocular and blood pressure in glaucoma. Ophthalmology 1980;87:3:222-8.
27. Porcella A, Maxia C, Gessa GL, Pani L. The synthetic cannabinoid WIN55212-2 decreases the intraocular pressure in human glaucoma resistant to conventional therapies. Eur J Neurosci 2001;13:2:409-12.
28. Adelli GR, et. al. Development of a delta9-tetrahydrocannabinol amino acid-dicarboxylate prodrug with improved ocular bioavailability. Inves Ophth Vis Sci 2017;58:4:2167-2179.