Planning the Procedure
In patients with keratoconus, placing intracorneal ring segments shortens the arc length of the corneal curvature and creates an artificial limbus within the cornea. The presence of the ring segments redistributes biomechanical stress forces more evenly, thus helping decrease progression of keratoconus, although not as much as corneal cross-linking. Ring segments also improve topography and reduce corneal irregularity, often improving vision.
Though Intacs placement can be beneficial, it’s not for every patient with keratoconus; it works best when the patient’s condition is neither too mild nor too extreme. In mild cases, the use of Intacs isn’t necessary, and a cross-linking treatment is often enough. On the other hand, in a severe case, the segments don’t provide much benefit and a deep anterior lamellar keratoplasty would be preferable.
The location of the cone will determine the need for one or two segments, or if one should use symmetric or asymmetric segments (i.e., a thick segment and a thin segment). For central or global cones, symmetric segments are useful. For eccentrically located cones, either single-segment placement inferior to the cone or an asymmetric placement with a thicker segment below the cone and a thinner one above it could be useful.
If the cone is centrally located, the ring segments may be centered on the pupil. For an eccentric cone, I try to decenter the Intacs slightly toward the apex of the cone, while still remaining centered within the pupil. Excessive decentration should be avoided to prevent visual symptoms such as glare and haloes in scotopic conditions.
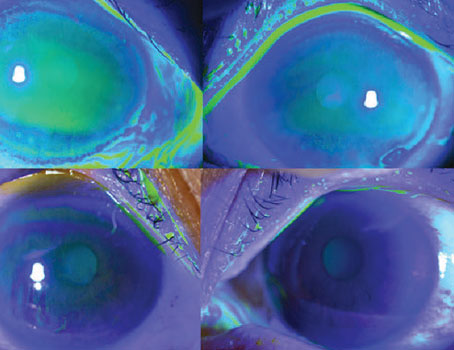
The femtosecond laser is a reliable means to create channels for the Intacs. I program the depth to about 75 to 80 percent of the minimum pachymetry in the implantation zone. The inner and outer diameters will depend on the type and thickness of the segments being implanted. A smaller optic zone as well as thicker segments give a greater flattening effect. Segments that fit well in their channels also have more effect as compared to segments lying in oversized channels. The entry incision is usually placed on the steep axis and oversized by 0.1 mm as compared to the channel thickness.
Proper Insertion
Although the channels are created by a laser, the segments are inserted by hand, so there is an art to it.
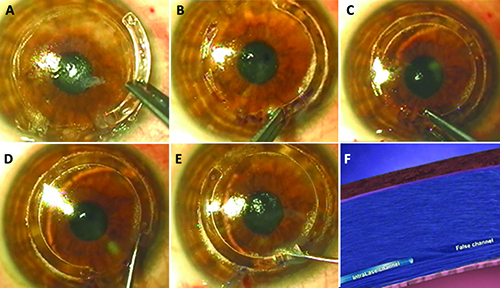 |
| Steps of the turnaround technique. Figure A: A false channel is inadvertently created. B: The segment is turned around and pushed in. C, D: The second segment used as an instrument to push the first forward. E: The final position of both segments. F: When the segment approaches the false channel from the opposite side, it flattens out the obstructing internal lip and thus crosses the point of resistance. |
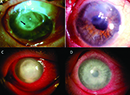
Dealing with False Channels
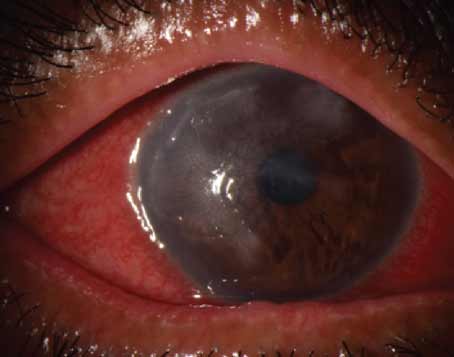
A false channel is where the segment begins tunneling into the corneal tissue adjacent to the actual channel. Signs that you’ve inadvertently created a false channel are increasing resistance to your insertion to the point where it may stop entirely, as well as radiating folds at the edge of the segment. The false channel has an internal lip of tissue that separates it from the laser-created channel, blocking the path. In addition to the obvious concern that the false channel results in the inability to implant the segment, it also invites complications such as neovascularization, segment migration and corneal melt.
All is not lost. By using a maneuver I described, the “turnaround technique,” one can still properly position the segments. On encountering resistance to implantation or on seeing corneal folds at the advancing edge, the surgeon stops trying to push forward. Instead, the segment is removed, turned around, and then inserted into the entry incision from the opposite direction. Since the femtosecond laser channel is a circumferential 360-degree channel, the segment will continue around until it’s fully in. The second Intacs segment is then used as an instrument to push the first segment the rest of the way. When the first segment reaches the location of the false channel, it’s coming from the opposite direction and will therefore flatten the lip and close the false channel. Final positioning can be done with a reverse Sinskey hook used in the positioning hole. In the end, both segments will then lie in their proper positions. (For a video of the technique, visit http://tinyurl.com/h8ugvwf.)
For asymmetric segments, the first segment is pushed in from the opposite side and the second segment is used to push it to its final position.
The segments are always pushed in following the arc of bubbles created by the femtosecond laser. If you’re facing difficulty in inserting the segments, and anticipate a delay in final implantation, it’s wise to mark the channel arc with a fine-tipped marking pen on the surface of the cornea so that even when the bubbles have dissipated completely, the segments can still be pushed in following the inked arc.
False-channel Complications
It’s important to recognize and react to false channels when they occur, as continuing to push a segment into the false channel can end in undesirable final positions, such as the segment straddling the entry incision or being too deep, too superficial or on an uneven plane of implantation. In some situations, implantation may have to be abandoned because of an inability to push the segment. Blind pushing can also lead to anterior or posterior perforation of the segment. Complications that can ensue include stromal necrosis and melt, anterior chamber perforation and neovascularization. Neovascularization generally traverses the entry incision and sometimes tracks down the channel, and it’s generally innocuous unless the patient requires a corneal graft later, in which case it can increase the risk of rejection.
Stromal necrosis and melt can lead to infection, and the best response in such a case may be to remove the segment. Stromal necrosis, though it may be deep, is generally localized over the segment and may require removal of the segment with the application of cyanoacrylate glue over the melt. REVIEW
Dr. Jacob is director of Dr. Agarwal’s Refractive and Cornea Foundation at Dr. Agarwal’s Eye Hospital and Eye Research Center. She has no financial interest in Intacs.