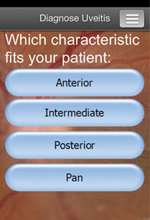
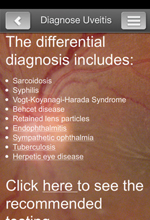
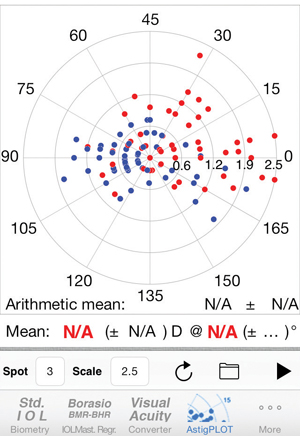
Astig PLOT
Astig PLOT is an app created by Edmondo Borasio, MD, head of cornea and refractive surgery at Moorfield’s Eye Hospital in Dubai, United Arab Emirates, as a handheld method for surgeons to analyze astigmatism in a group of eyes. The application plots preop/postop astigmatism, aggregate astigmatism, surgically induced astigmatism and mean astigmatism. The program also supplies the standard deviation of the mean astigmatism and the surgeon’s SIA.
To use Astig PLOT, the surgeon enters the input values into a comma-separated value file that he uploads to the application. “The surgeon enters pre- and postoperative K values, or refractions, and their respective meridians, or axes, and the program will calculate the mean arithmetic and mean vector SIA,” explains Dr. Borasio. “The program shows the SIA in terms of sphere magnitude, cylinder magnitude and meridian/axis, and also shows the conversion of the SIA to Cartesian (x,y) notation. Cartesian notation is needed when calculating the mean of multiple individual SIAs.”
Dr. Borasio says he developed the application after running into annoying impediments with statistical analysis programs. “I was fed up with using standard statistical analysis programs in which I had to format the graph, change the scale and reformat the axes each time I used them,” he explains. “The Astig PLOT graphs are autoscaling to the highest value in the series, but also allow you to choose a custom scale if, for example, you wish to compare two graphs from two different series. In such a case, you would choose the same value for both graphs.
|
Astig PLOT is available for iOS 4.3 or later on the Apple App Store, and costs $19.99. For information, visit edmondoborasio.com.
Steinert/Oliver Marker
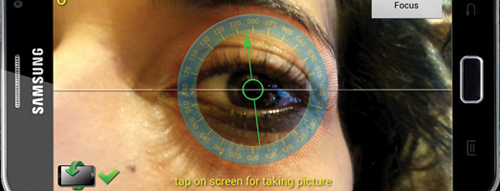
The Steinert/Oliver Smart Phone Marker from Rhein Medical is the brainchild of Stanford University’s Roger Steinert, MD, and Alejandro Oliver, MD, of Timmins and District Hospital in Timmins, Ontario, Canada. Rather than a software application, it’s the fusion of an instrument and a smartphone. “We’d been looking to use smartphones as levels for toric lenses and toyed with several adapters for the different phone brands,” explains Dr. Oliver, “There are so many phones out there, however, that it made it challenging to find one adapter that worked for all of them. So, we got the idea that we can hook the instrument to the earphone jack because, no matter what brand of smartphone you have or which generation it is, it has an earphone jack, and the earphone jacks are exactly the same across the board.”
To use the marker, the surgeon downloads one of many level apps available and plugs the marker into the earphone jack. The level app will indicate when the marker is being held exactly horizontally level, allowing the surgeon to mark the patient’s eye before surgery. “My preference is to mark the zero to 180 axis,” says Dr. Oliver, “So, I basically mark at 3 o’clock and 9 o’clock. I mark this axis bedside after the patient’s been through all the paperwork and before he’s gotten any dilating drops. Then, in the operating room, I use a Mendez ring and a marker to mark the meridian of the astigmatism. You’ll get a very durable mark, but you have to make sure the patient doesn’t rub his eye after you’ve made it. This is especially true if there’s lidocaine gel on the ocular surface. Alternately, you could also use the smartphone to mark the desired IOL axis in one step. To do that, however, you sometimes have to hold your hand in certain awkward positions. But, if you’re OK with holding your hand like that, you can do the mark once and that’s it; you won’t have to bother making additional marks in the OR.”
The kind of level application the surgeon uses can have an effect on the ease of use, and possibly the accuracy, of marks made with the instrument. “There are a lot of level apps out there for smartphones,” says Dr. Oliver. “My preference is not the bubble-level app, but instead a level app with an actual dial. The bubble app is a little too qualitative for me—you can be off by a few degrees and not be able to really tell. Therefore, a level app that has actual continuous gradations in degrees is ideal, since you get a quantity.”
|
The marker costs $295. For information, visit rheinmedical.com or call 1 (800) 637-4346.
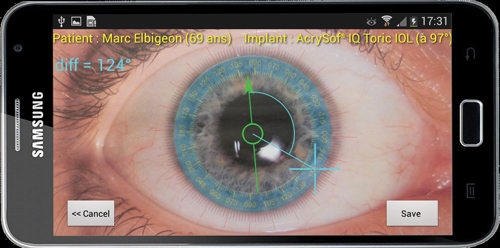
Toreasy
Paris ophthalmologist Damien Gatinel says he developed the non-contact Toreasy astigmatic axis application to try to overcome sources of error that can crop up when patients move or tilt their heads. “When you mark the eye with a pendulum marker, you are trying to align the axis of the marking system with a horizontal orientation as perfectly as you can, so you’ll at least know where the zero/180 axis is,” he says. “But this relies on your marking skills, and the patient will sometimes rotate his head to try to make you more comfortable with your manual marking. But this rotation, unfortunately, introduces more error.”
To try to eliminate having to touch the patient to acquire the axis, Toreasy takes advantage of smartphones’ built-in accelerometers and gravity sensors. “Toreasy will constantly track the zero/180 direction on the screen using a bar that is unaffected by any rotation or tilt that you introduce by holding it. It will always give a level line. So, looking through the phone’s display, you face the patient and ask him to slightly tilt his head until the zero/180 line goes through both pupils. This is the proper head orientation. You then ask the patient to stay still and you zoom in on one eye and take a snapshot. You then examine the picture you’ve taken and find a vessel or other mark on the eye and use an on-screen reticle to mark its position. The app will mark it on the screen and give you the landmark’s position in degrees. If there are no vessels or prominent ocular structures that you can easily find, you can use a pen to place a mark on the eye wherever you want before you capture the image and place the reticle on that. Either way, you’ll know exactly where that mark is in relation to the zero/180 axis in degrees.
|
Dr. Gatinel says that, after having used the Toreasy marking system for a while, he’s learned that the farther away the anatomic landmark is from the center of the image, the more precise the degree mark will be. “If you pull the reticle arrow using your finger farther out into the periphery and then select the degree location, you’ll get extra precision,” he says. “You can make more precise, fine adjustments.”
In terms of centering the Toreasy gauge on the image of the eye, Dr. Gatinel recommends using the patient’s limbus rather than the center of the pupil. “We recommend using the limbus because the IOL won’t be centered if you center the axis measurement on an eccentric pupil,” he says. “The intraocular lens centers in the capsular bag, which is probably more aligned with the limbus than with the pupil, the latter of which tends to sometimes move in a non-concentric way.”
|
Toreasy is available for Android-based devices at the Google Store for $200 ( https://play.google.com/store). It’s also available pre-loaded on a new Samsung S4 Zoom smartphone for $2,500. Dr. Gatinel says it will work on Apple iOS devices but isn’t yet available on the Apple App Store.
Since a lot of the accuracy of the digital marking process with Toreasy relies on the smartphone’s camera, Dr. Gatinel recommends using the application on a device with a high-resolution camera, such as the latest generation of Samsung devices (S4, S4 Zoom and S5, for example). He says a good zoom feature that maintains a sharp image is helpful also, since it makes it easier to locate ocular features. For more information on Toreasy, visit toreasy.com. REVIEW
All of the surgeons interviewed have a financial interest in their respective apps or devices.