Here, we profile a number of these apps, and Rohit Krishna, MD, an associate professor of ophthalmology and director of glaucoma at the University of Missouri-Kansas City School of Medicine, who helped to create the popular app Eye Handbook (Cloud Nine Development, Overland Park, Kan.), shares some of his thoughts on this topic.
Putting Technology to Use
Dr. Krishna notes that many of the ideas for patient compliance aids come from other areas of medicine. “Ophthalmology is ahead of most specialties in terms of diagnostic tools, but when it comes to helping patients manage their medications, other specialties are ahead of us,” he says. “Helping patients be compliant is an issue because 20 to 30 percent of prescriptions are never filled, and patients have plenty of trouble remembering to use drops—not to mention getting the right amount onto the eye when they do remember. I’ve seen estimates that poor adherence results in $290 billion a year in higher U.S. medical costs. On the other hand, some of these ‘reminder’ technologies have been shown to improve adherence by as much as 40 percent, which is a significant improvement.
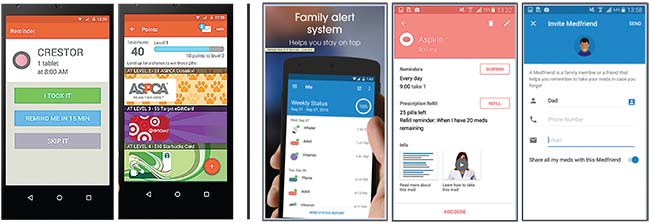 |
| Popular apps that can help patients remember to use medications include MangoHealth (sample screens, above, left) and Medisafe Pill Reminder & Medication Tracker (above right). More than 250 apps are available online, each with different advantages and limitations. |
“An important category of electronic patient management devices today is systems that use mobile phone technology,” he continues. “That includes sending text message reminders, using smartphone apps and having interactive voice-response systems. Using mobile technology to help patients manage their health is referred to as ‘mHealth.’ It’s becoming an increasingly popular way to help patients because smartphones have become ubiquitous, even in developing countries.
“In addition to providing reminders to take medications, a smartphone allows two-way communication with the patient, at the patient’s convenience,” he notes. “Smartphones are easy to use and have few limitations in terms of geography or time. Of course, contacting a patient by telephone is nothing new; doctors have been calling patients to make sure they’re taking their medications or remind them of an upcoming appointment for years. But the computerized capabilities of smartphones allow them to help in ways that a noncomputerized phone can’t. To that end, the Bill and Melinda Gates Foundation has given away a lot of grants to people to help them come up with clever ways to adapt mobile technology for health uses.”
In addition to acting as a reminder, mobile devices can also use psychological principles to try to alter the patient’s behavior in a positive direction. Dr. Krishna notes that one approach to modifying a patient’s behavior is called gamification, which provides the patient with rewards for maintaining the desired behavior. “For example, the patient might receive virtual tokens that can be converted into actual prizes,” he says. “One example of this is the HealthPrize system (HealthPrize Technologies; South Norwalk, Conn.) The patient can win tokens for everything from reporting each use of the medication to taking surveys and answering questionnaires. The app offers multiple types of incentives, including charity donations, gift cards, coupons for local discounts and health-related merchandise as rewards. The company says that its system has been shown to increase prescription refills by an average of 52 percent across all of the current platforms using the system. (You can find out more at Healthprize.com.) Measuring whether or not you’re doing what you’re supposed to do is a key part of this, and that will tie into some of the developments that still lie in the future, like a bottle with an electronic chip in it.”
Although a few compliance apps use some variation on this idea, Dr. Krishna notes that he’s not aware of any ophthalmologist who has tried using this system directly to influence patients—so far. “Right now ophthalmologists just reward you with good care,” he says. “It’s sad that you have to reward people to get them to do things they’ll benefit from, but human beings do respond to being rewarded.”
Some Popular Apps
Here are just a few of the apps available to your patients:
• MangoHealth & Pillboxie. These two apps are straightforward medication-reminder systems. Once you input the schedule the patient should follow, the phone provides a notification when it’s time for an eye drop or pill and displays a picture of the medication that needs to be taken. (A picture can be very helpful if the patient is taking a lot of pills or using multiple drops.) MangoHealth, which uses the gamification principle to reward patients for following instructions, is free and can be downloaded from the Apple App Store or Google Play. (See sample screens, above, left.)Pillboxie is free for the iPhone at the Apple App Store. (For more information, you can visit mangohealth.com or
 |
| The Wills Eye Glaucoma app includes educational videos, appointment reminders, data storage, a visual field tutorial and an IOP tracker. |
• Memotext. Dr. Krishna says the Memotext system (Memotext; Bethesda, Md.) is a good example of a digital health application; it uses the patient’s smartphone to send reminders and interact with the patient.
A 2014 study conducted at the Johns Hopkins University School of Medicine, Baltimore, tested Memotext’s ability to alter behavior. After determining that 70 patients out of 491 were nonadherent to their once-a-day eye-drop medication regimen, 38 were randomized to use the Memotext system. They received daily messages, either text or voice, reminding them to take their medication. The control group received usual care. The median adherence rate in the 38 participants using the system increased from 53 percent to 64 percent (p<0.05). There was no change in the control group.
The study authors noted that one important aspect of this study was that this type of intervention is feasible in terms of the time and cost required from the ophthalmology practice. (The Memotext company estimated the cost to be approximately $20 per year per patient.) Also, the automated reminders were well received by the study participants.2 (You can find out more at memotext.com.)
• Medisafe Pill Reminder & Medication Tracker. Created by Drugs.com, this app is free and available for both iOS and Android. According to iMedicalApps, it had the most functionality of the 272 apps they surveyed (14 different functions). For example, Medisafe can bring family members into the process to remind the patient if a dose is missed. If the patient was due to take a drop at 7 o’clock but forgot, his phone would automatically turn on, and a relative would be alerted that he didn’t take his pill. That relative could call the patient to remind him. Alternatively, the reminder could be automated using a text message or a personalized video of the relative reminding the patient to take the medication or eye drop.
• AlarMeds. This app is only available for Android. It allows customization of your dosing schedule, the medication image, the alarm and other features. According to iMedicalApps, AlarMeds’ seven functions was the most of any app in the group of programs they surveyed that they considered basic rather than advanced. A simple version of the app usable with only one medication is free; a more advanced version is less than $2.
• Wills Eye Glaucoma App. Wills Eye Hospital in Philadelphia has created an app (free at the Apple App Store) designed to help glaucoma patients; it was developed by the Wills Eye Glaucoma Research Center in collaboration with Drexel University. It allows you to program your phone to beep when you’re due for an eye drop, showing you a picture of the correct drop to take. It also provides educational videos, appointment reminders, medical and ocular data storage, a visual field tutorial and an IOP tracker.
A 2016 paper summarized a study evaluating the characteristics and attitudes of patients who were eligible to use the Wills Eye app.3 Of the 50 subjects interviewed (mean age 59.5 ±17.3 years), 88.6 percent of them lived in a household with access to a smartphone or tablet, and 73 percent were receptive to using the automated reminder feature of the app. (Interestingly, however, many of those surveyed said they wouldn’t use the app if they had to pay $3 for it.)
• MyEyeDrops. This option was created by the Singapore National Eye Centre and is available at the Apple App Store. Its reminder alarm shows the patient which drop to take and which eye to put it in, and allows multiple users and caregivers to be alerted of the reminders. It also provides a video showing the correct way to instill eye drops, and a diary to help dry-eye patients monitor the frequency and intensity of their symptoms.
What May Lie Ahead
Eventually, patient reminders may become unnecessary, thanks to two technologies already in the pipeline. The first is extended-release devices that will eliminate the need for drops. A number of different approaches are being tested, including injections of a depot into the subconjunctival space; putting a flexible ring that elutes medication onto the eye; contact lenses and punctal plugs that elute medications; and injecting something such as a nanoparticle or nanowafer inside the eye. Any of these, if effective, could eliminate the need for the patient to remember to take drops.
The other option is a feedback device that monitors factors such as intraocular pressure on an ongoing basis. This would allow treatment to be based on need. The patient might still need to use an eye drop, but use could be limited to times when a sign of trouble was detected. For example, researchers in Germany are developing an intraocular lens that incorporates an IOP sensor. Contact lenses with embedded IOP monitors are already available, although they’re mostly being used for research so far.
To the extent that a drop reminder is still needed, the nature of reminder apps will probably change in the years ahead. For example, Apple is working on ‘augmented reality’ glasses that you might wear all day. It’s not hard to imagine that when it’s time to take your drops, the bottle will appear on the screen in your glasses, along with instructions explaining what to do.
“Today, we’re in the midst of the digital revolution, with new technology appearing every year,” notes Dr. Krishna. “Like other medical specialties, we can harness this technology to improve patient compliance. At the same time, it will improve our ability to monitor both the patient’s compliance and soon, the status of factors such as IOP. All of this has the potential to have a great impact on patient care and produce significant cost savings for our health-care system.” REVIEW
1. Study finds the best medication adherence medical apps. (no author listed) iMedicalApps.com, January 2017.
2. Boland MV, Chang DS, et al. Automated telecommunication-based reminders and adherence with once-daily glaucoma medication dosing: The automated dosing reminder study. JAMA Ophthalmol 2014;132:7:845-850.
3. Waisbourd M, Dhami H, Zhou C, et al . The Wills Eye Glaucoma App: Interest of patients and their caregivers in a smartphone-based and tablet-based glaucoma application. J Glaucoma 2016;
25:9:e787-91.



