SLT’s Acceptance
Though the exact number of surgeons who use SLT as a first-line option is still unclear, studies of utilization of laser trabeculoplasty have shown that physicians are trusting it more all the time. In 2007, Pradeep Ramulu, MD, and his colleagues at Johns Hopkins University analyzed the utilization of glaucoma procedures from 1995 to 2004.1 They found that, from 1995 to 2001, the number of laser trabeculoplasties decreased by 57 percent, from a high of 151,244 in 1995 to a low of 75,647 in 2001, which many ascribe to the emergence of prostaglandins. However, from the time of SLT’s approval in 2001 to 2004, the number of laser trabeculoplasties suddenly more than doubled, from 75,647 to 157,490. A similar phenomenon occurred in Canada. There, a group of researchers found that laser trabeculoplasty use increased by 230 percent from 2001 to 2004.2 “The introduction of SLT has made us re-examine the issue of laser trabeculoplasty as an initial therapy,” says Steve Gedde, MD, of the Bascom Palmer Eye Institute. “I feel that the efficacy and safety of laser trabeculoplasty has prompted many surgeons, including myself, to consider it an initial therapy for glaucoma.”
SLT’s Efficacy
SLT’s efficacy has been analyzed a number of ways in studies over the years, including the following:
• SLT vs. medications. Surgeons say it’s been their experience, both in clinic and in reviewing published studies, that SLT is as good as medical therapy as a first-line treatment. A recent prospective, randomized study comparing SLT to drugs analyzed 127 eyes of 69 patients with open-angle glaucoma or ocular hypertension.3 The patients were randomized to 100 SLT applications encompassing 360 degrees of their trabecular meshwork, or medical therapy with a prostaglandin analog. Fifty-four patients reached the nine to 12 month follow-up point (29 SLT patients and 25 medical-therapy patients). Starting from similar baseline intraocular pressure levels, the mean IOP at the last follow-up was 18.2 mmHg (a 6.3-mmHg pressure reduction) in the SLT group and 17.7 mmHg (7-mmHg reduction) in the medical group. By the last follow-up, 11 percent of the SLT eyes required an additional SLT treatment and 27 percent of the medical group needed additional medication. The researchers say that even though the medical group needed more therapy to reach the target pressure, there was no statistically significant difference between the two groups.
Dr. Gedde says surgeons can expect that about 80 percent of patients will respond to SLT treatment, though it depends on how you define a clinically significant response. “On average, you’ll see a 20- to 30-percent reduction in pressure,” he says. He notes that the main advantage of SLT vs. medications is that, if the patient responds to it, it remains effective independent of compliance. “It will be working 24 hours a day, seven days a week,” he says. In a currently unpublished study of SLT retreatments performed by Doheny Eye Center glaucoma specialist Brian Francis, Dr. Francis found an SLT success rate of between 40 and 50 percent with the first SLT treatment, though he notes he was using strict surgical success criteria from the Tube vs. Trabeculectomy study. “We defined success as a 20 percent pressure reduction or more with a final pressure between 5 and 21 mmHg with no additional glaucoma medications or procedures,” he says. “When you consider that we were applying surgical success criteria to a non-invasive laser, we feel that SLT was pretty effective.”
In terms of how long the effect will last, University of Toronto professor Yvonne Buys, MD, says the duration of SLT varies in the literature, but gives a general rule of thumb: “The last time I closely examined surgeons’ response rates of success, there was a rate of 69 to 92 percent at six months, 52 to 98 percent at a year, 88 percent at two years and 52 to 76 percent at three years,” she says, noting that different studies’ definitions of success varied. Dr. Francis says that, in his study of repeat SLT treatments, most of the patients still had a good effect at two years, but it was quite variable. “We did have some patients for whom it was less than a year between laser treatments,” he says.
 • Chance of success with SLT. To give surgeons an idea of what type of results to expect from SLT and which patients might benefit from it, Cindy Hutnik, MD, PhD, associate professor of ophthalmology and pathology at the University of Western Ontario, took part in a study aimed at formulating a prediction rule for SLT treatment. She and her co-workers tried to isolate the factors that might help predict the likelihood that SLT will be effective.4 In their study, they defined success as a 20 percent or greater reduction in IOP. “We examined everything,” Dr. Hutnik says. “We looked at such factors as the medications the patients were on, whether they had undergone cataract surgery, whether they were on steroids, and the level of pigmentation in their eyes. In the end, the only consistent factor predictive of SLT response was the IOP the patient started off with. As with an eye drop, if the pressure is 32 mmHg and you put the patient on a drop, or in this case, do SLT, you’ll get a nice 30-percent reduction from baseline. And, just like adding an eye drop to someone already on glaucoma medication, if you perform SLT on someone already on a drop, you’re not going to get a 30-percent reduction. The prediction rule analysis reinforced that SLT is really no better or worse than another class of eye drops; you get your biggest response when the pressure’s high and the patient is treatment naïve.” To get an idea of the probability of success with SLT based on Dr. Hutnik’s research, refer to Figure 1.
• Chance of success with SLT. To give surgeons an idea of what type of results to expect from SLT and which patients might benefit from it, Cindy Hutnik, MD, PhD, associate professor of ophthalmology and pathology at the University of Western Ontario, took part in a study aimed at formulating a prediction rule for SLT treatment. She and her co-workers tried to isolate the factors that might help predict the likelihood that SLT will be effective.4 In their study, they defined success as a 20 percent or greater reduction in IOP. “We examined everything,” Dr. Hutnik says. “We looked at such factors as the medications the patients were on, whether they had undergone cataract surgery, whether they were on steroids, and the level of pigmentation in their eyes. In the end, the only consistent factor predictive of SLT response was the IOP the patient started off with. As with an eye drop, if the pressure is 32 mmHg and you put the patient on a drop, or in this case, do SLT, you’ll get a nice 30-percent reduction from baseline. And, just like adding an eye drop to someone already on glaucoma medication, if you perform SLT on someone already on a drop, you’re not going to get a 30-percent reduction. The prediction rule analysis reinforced that SLT is really no better or worse than another class of eye drops; you get your biggest response when the pressure’s high and the patient is treatment naïve.” To get an idea of the probability of success with SLT based on Dr. Hutnik’s research, refer to Figure 1.
• The typical first-line SLT patient. As for the typical SLT patient, Dr. Francis says that as long as the patient has open-angle glaucoma, or is even a severe-risk ocular hypertensive, he’s a candidate. “Basically anyone with an open angle whom you’d treat with medical therapy,” he avers. There are a few exceptions, however. “There are patients on maximal medications with pressures that are so high you wouldn’t expect success with SLT,” Dr. Francis says. Dr. Buys says it might be prudent to avoid patients with inflammatory glaucoma. “Also, be careful in patients with a heavily pigmented trabecular meshwork such as those with pigmentary glaucoma and pseudoexfoliation,” she says. “There have been reports that those patients can have significant pressure rises afterward, and some suggest that they may be better served with an ALT due to all of the pigmentation.” Dr. Hutnik, however, says that she hasn’t experienced pressure spikes with pseudoexfoliation—only in pigment dispersion cases.
Dr. Gedde says he would add to the list of contraindications certain secondary open-angle glaucomas where the angle is open but the patient still isn’t a good candidate. “For instance, glaucoma due to elevated episcleral venous pressure in which the resistance to aqueous outflow is downstream from the trabecular meshwork,” he says.
SLT’s Safety
Surgeons say that, like first-line medications, SLT is very safe and has a low incidence of complications.
 |
Dr. Hutnik notes that there have been anecdotal reports of some SLT patients having corneal edema or bleeding in the eye. “It doesn’t seem to be a widespread problem but instead looks like it involves something other than the laser, such as a preop or post-op drop,” says Dr. Hutnik.”
Repeatability
Influencing the efficacy of SLT is the fact that the procedure appears to be repeatable. It’s only recently that data on repeatability has emerged.
In 2009, a group of researchers from Yale University performed 360-degree SLT on 44 eyes of 35 open-angle glaucoma patients (primary open-angle, pseudoexfoliation or pigmentary glaucoma) who were uncontrolled on maximum tolerable medical therapy. The treatment was successful for at least six months in all cases, then needed to be repeated. They defined success as a peak IOP reduction of at least 20 percent, and found no significant difference in success rates between the first and second SLT treatments, suggesting that the repeat SLT can be just as safe and effective as the first one.6
Dr. Francis presented a report on SLT’s repeatability at the recent meeting of the American Glaucoma Society. In it, his group performed 360-degree SLT on 132 eyes. The eyes then had to have a positive effect for at least six months, after which a second SLT procedure could be performed. “In our overall analysis, we found that there was a significant difference between the baseline pressures before SLT1 and SLT2,” says Dr. Francis. “We think that’s because, clinically speaking, as we saw the pressure going up we would treat before it reached the previous baseline. So, with the unequal baselines, the end result was the same, about 16 mmHg in each group. However, since there was a lower baseline with the SLT2 group, it follows that it didn’t lower the pressure as much as SLT1. We were able to do a subgroup analysis in which we took a group of around 50 patients that were matched for baseline IOP. We found that, in that analysis, there was an equal pressure reduction between groups.”
Surgeons think that more of their colleagues will embrace SLT as they get frustrated with poor patient compliance with medication.
“Glaucoma specialists use a certain algorithm for treating their patients that usually starts with medical therapy,” says Dr. Gedde. “I think that approach is probably the most common one. However, I think SLT is a very appropriate initial therapy and it’s my impression that it may be underutilized.”
Dr. Francis presented a report on SLT’s repeatability at the recent meeting of the American Glaucoma Society. In it, his group performed 360-degree SLT on 132 eyes. The eyes then had to have a positive effect for at least six months, after which a second SLT procedure could be performed. “In our overall analysis, we found that there was a significant difference between the baseline pressures before SLT1 and SLT2,” says Dr. Francis. “We think that’s because, clinically speaking, as we saw the pressure going up we would treat before it reached the previous baseline. So, with the unequal baselines, the end result was the same, about 16 mmHg in each group. However, since there was a lower baseline with the SLT2 group, it follows that it didn’t lower the pressure as much as SLT1. We were able to do a subgroup analysis in which we took a group of around 50 patients that were matched for baseline IOP. We found that, in that analysis, there was an equal pressure reduction between groups.”
Surgeons think that more of their colleagues will embrace SLT as they get frustrated with poor patient compliance with medication.
“Glaucoma specialists use a certain algorithm for treating their patients that usually starts with medical therapy,” says Dr. Gedde. “I think that approach is probably the most common one. However, I think SLT is a very appropriate initial therapy and it’s my impression that it may be underutilized.”
1. Ramulu PY, Corcoran KJ, Corcoran SL, Robin AL. Utilization of various glaucoma surgeries and procedures in Medicare beneficiaries from 1995 to 2004. Ophthalmology 2007;114:12:2265-70.
2. Rachmiel R, Trope GE, Chipman ML, Gouws P, Buys YM. Laser trabeculoplasty trends with the introduction of new medical treatments and selective laser trabeculoplasty. J Glaucoma. 2006;15:4:306-9.
3. Katz LJ, Steinmann WC, Kabir A, Molineaux J, Wizov SS, Marcellino G. Selective Laser Trabeculoplasty Versus Medical Therapy as Initial Treatment of Glaucoma: A Prospective, Randomized Trial. J Glaucoma 2011 May 3. [Epub ahead of print]
4. Mao AJ, Pan XJ, McIlraith I, Strasfeld M, Colev G, Hutnik C. Development of a prediction rule to estimate the probability of acceptable intraocular pressure reduction after selective laser trabeculoplasty in open-angle glaucoma and ocular hypertension. J Glaucoma 2008;17:6:449-54.
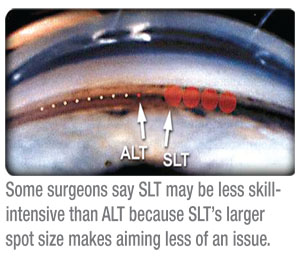
5. Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology 2001;108:4:773-79.
6. Hong BK, Winer JC, Martone JF, Wand M, Altman B, Shields B. Repeat selective laser trabeculoplasty. J Glaucoma 2009; 18:3:180-83.