As many have noted, dry eye ain’t what it used to be. Just a few decades ago, with little existing knowledge about the causes and treatment of dry-eye disease, doctors were at a loss to do much for these patients. Today, the situation has changed drastically, with a proliferation of tests and treatments. Now, these changes have led to the appearance of specialty clinics designed to treat dry eye.
Paul Karpecki, OD, of iOR Partners, director of cornea services at Kentucky Eye Institute in Lexington and an associate professor at the University of Pikeville Kentucky College of Optometry, has served as a research investigator for numerous clinical studies relating to ocular surface disease, and has helped set up eight dry-eye clinics in different practices (all of which he says are doing well). “Dry-eye treatment has evolved a lot,” he points out. “At the outset, only about half of our dry-eye patients ended up satisfied; we didn’t have the knowledge or diagnostics or therapeutics to really help them. Fast-forward 20 years, and we now have numerous resources. Today, the majority of our patients end up highly satisfied.”
As more practices have decided to open dry-eye clinics, others are wondering if they should follow suit. Here, doctors deeply involved in treating dry eye—most with their own specialty clinics—answer 10 questions frequently asked about opening a dry-eye clinic.
1. Who should do this?
Vance Thompson, MD, founder of Vance Thompson Vision in Sioux Falls, South Dakota, and a professor of ophthalmology at the University of South Dakota School of Medicine, argues that there’s definitely a need for this kind of specialty dry-eye treatment. “Dry eye is one of the most underdiagnosed conditions in eye care today, and one of the most undertreated,” he says. “If you want to embrace dry-eye care, it can definitely be a full-time practice.”
“I don’t think there’s any criteria that makes a given practice a good or bad place to open a dry-eye clinic,” says Dr. Karpecki. “Every practice, large or small, has plenty of dry-eye patients. No type of practice is immune to dry eye—although a retina specialist might find this too far afield.”
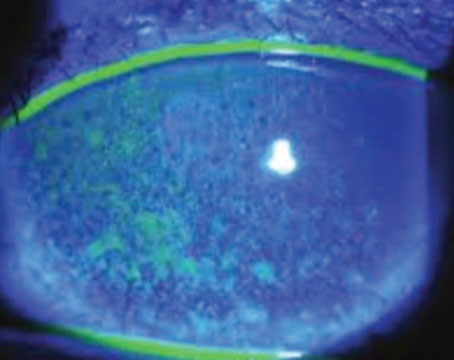
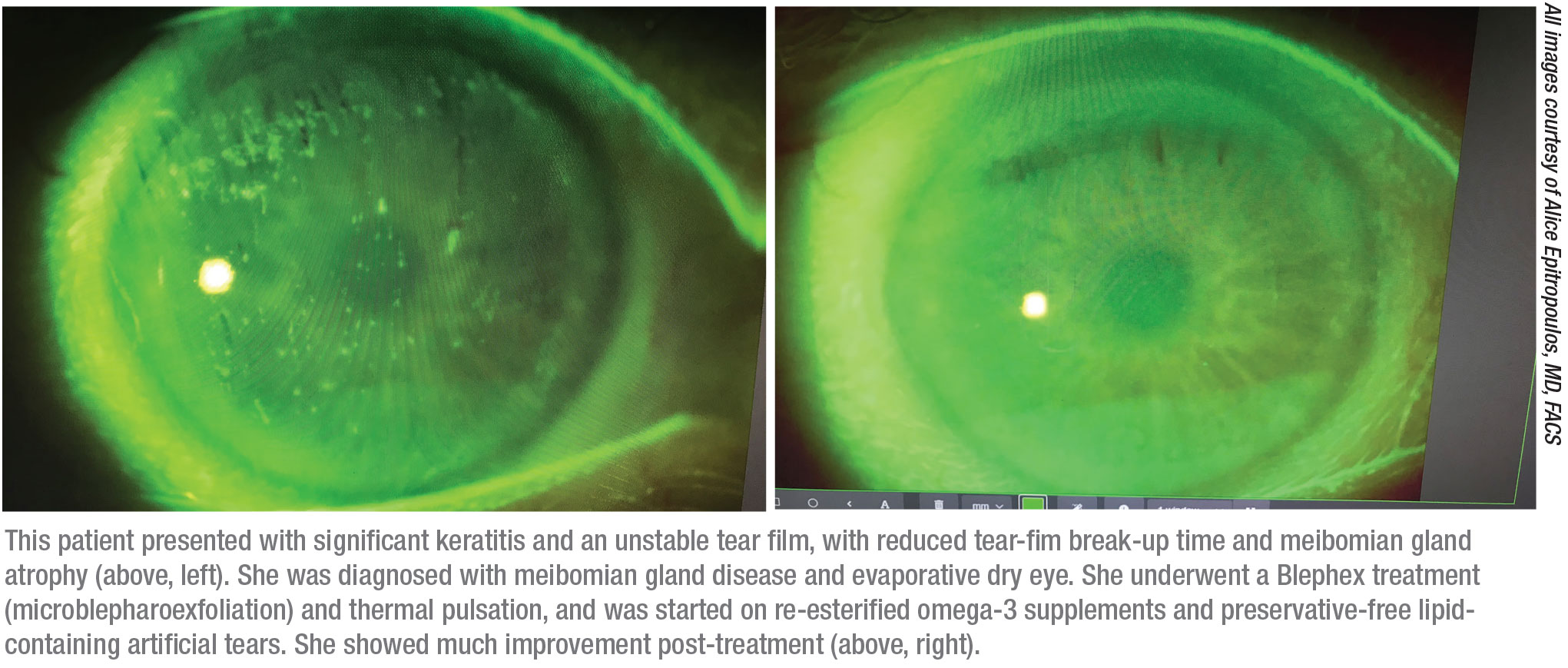
Treating dry eye can be especially helpful for refractive surgeons, making a dry-eye clinic worth considering. “Focusing on dry-eye treatment improves biometry and IOL calculations,1 surgical outcomes, and most important, it improves patient quality of life,” notes Alice Epitropoulos, MD, FACS, a partner at Ophthalmic Surgeons and Consultants of Ohio and a clinical assistant professor at The Ohio State University. She runs the Dry Eye Center of Excellence for the group practice, while also performing cataract and refractive surgery.
John D. Sheppard, MD, MMSc, president of Virginia Eye Consultants and a professor of ophthalmology at Eastern Virginia Medical School, who set up a dry-eye specialty clinic in his practice about six years ago, agrees. “Premium IOL surgeons understand the value of this,” he notes. “The one thing everybody hates is an angry multifocal lens patient who paid $3,000 for a new IOL and then can’t see optimally.” (Dr. Thompson adds that measuring and treating dry eye prior to surgery not only can make your outcomes more accurate, it can also help prevent patients from blaming postop problems on your surgery.)
Some reasons for deciding not to pursue this may relate to the surgeon’s personal interests. Preeya K. Gupta, MD, who specializes in cornea and refractive surgery and is an associate professor of ophthalmology at Duke University Eye Center in Durham, North Carolina, says that although her academic practice offers many of the high-tech diagnostic and treatment options for dry eye, they’ve opted not to separate out their dry-eye treatment into its own clinical entity.
“I had mixed feelings about focusing exclusively on treating dry eye,” she explains. “It’s an emotional challenge to manage many of these patients, some of whom are very frustrated. But even without a dedicated dry-eye clinic, our volume of dry-eye patients has grown over the years. Patients are eager to get care for their dry-eye condition.”
 |
2. How risky a proposition is this?
“I think opening a dedicated dry-eye center is a low-risk proposition,” says Dr. Gupta. “You’re offering your patients a service that’s in high demand. Plenty of patients out there have dry eye but haven’t been treated—including many of your existing patients. If you screen for this, you’ll find a high incidence of dry eye, and many of those patients are looking for specialized care.”
“Many ophthalmologists avoid treating dry-eye disease because they feel that doing so would slow them down,” says Dr. Epitropoulos. “Some also believe that treating dry-eye disease has low profit margins. Some worry that it would distract them from their surgical practices. But those are myths; they’re not true. Having a dry-eye center is a practice-builder. Remember that most commercial payers and Medicare will reimburse for tear osmolarity and InflammaDry.” Dr. Sheppard notes that even the latest therapeutic devices, which require a considerable investment, have the potential to bring in significant patient-pay revenue.
“Creating a dry-eye center involves a multidimensional approach,” adds Dr. Epitropoulos, “but it’s something that any practice can accomplish if it’s committed to doing it.”
3. Will having a dry-eye clinic bring in extra patients?
Dr. Thompson says a dry-eye clinic will definitely bring in more patients. “In addition,” he says, “when patients come in for dry-eye treatment, they’re likely to have other problems as well, such as cataract, glaucoma, corneal issues and other concerns.”
Dr. Sheppard says his dry-eye clinic draws in extra patients. “I think it’s most useful for attracting the attention of internet surfers, and referral by word of mouth,” he says. “I think it impresses people who have a dry-eye problem; it tells them they’re coming to the right place. Patients who come to our clinic have often seen other doctors and been unhappy with the outcome. When they realize that you respect their complaints and you’re not making fun of them, they like that. They’ll refer other patients to you as well.”
Dr. Thompson adds that a dry-eye clinic can be a great source of referrals. “We like to work with the doctors in our region,” he says. “We make sure they know that we have a dry eye center of excellence, and that we’re here for them if they have dry-eye cases that they’re not making headway on, or if they want help with more serious things such as making serum tears or working with amniotic membrane tissue.” Dr. Epitropoulos concurs, noting that a large percentage of her patients come from referrals, from both doctors and patients.
Dr. Karpecki points out that although a dry-eye clinic should bring in new patients, that might not happen at the outset. “It takes a while,” he says. “In the beginning, your dry-eye patients will mostly come from your existing patient pool, so internal marketing will be key. But you’ll be increasing the number of exams, because you’re getting patients into your specialty clinic, and many of these patients will need procedures. The new patients will come later.”
4. Will we need specialized personnel?
 |
Dr. Karpecki says that running a dry-eye clinic does involve a skill set, so you shouldn’t jump in without training your staff—and possibly bringing in a specialist.
“Figuring this out by trial and error would be a waste of your time and effort,” he says. “To get a good dry-eye clinic up and running, get help from those who’ve already done it. Often this requires bringing in a different doctor—an MD or an OD—who can focus on building it up and taking it to the next level. Find a doctor who has the passion and drive to be dedicated to it, even if he or she doesn’t yet have all the knowledge and experience that comes with running this type of clinic. That can be obtained.”
“If you set up your own clinic you’ll need to have ancillary personnel to help you out,” Dr. Sheppard agrees. “A number of the point-of-service dry-eye tests are useful diagnostics—but only if they’re done correctly. You want to have staff who are specifically trained so they can perform the procedures and testing properly. Usually, the companies that make the tests will send in personnel to train your staff; then, those staff members can help train the rest of your staff.”
Dr. Epitropoulos notes that you may also want to enlist a clinical research coordinator. “Having a dry eye center of excellence and a clinical research coordinator who’s organized and experienced gives us the opportunity to participate in clinical trials. Being able to do that gives our patients access to new cutting-edge treatments and technologies that may not be available in private practice,” she says.
5. Can a dry-eye clinic produce useful data?
Doctors with dry-eye clinics agree that it allows them to collect data that’s often helpful—sometimes in surprising ways.
“The data clinical staff can gather has been very useful clinically, and the data our publicity team gathers has been very constructive for our business,” says Dr. Sheppard. “Of course, you have to actually look for the data, but you can do many useful internal studies if you’re predisposed to do so.”
Dr. Karpecki believes that monitoring the data from such a clinic is essential. “The future of dry-eye treatment—and successful clinics—is going to center around using big data and artificial intelligence,” he says. “We’ve already started doing that in our clinics. We’ve create a simple algorithm for the doctors; they put in the patient’s information and get back a recommendation for treatment. Then, to refine this, we have the patient fill out a form detailing the response to each treatment.
“The information we gain from doing this is sometimes counterintuitive,” he continues. “For example, I used to teach students that if your patient has an evaporative dry eye related to meibomian gland issues or lipid deficiency you should recommend an oil-based tear. When we analyzed our data it turned out that I was only partly right. In the mild-to-moderate cases that was good advice. However, the really severe patients—those with rosacea, a minimal number of glands, high osmolarity or more advanced forms of the disease—actually preferred osmolarity-lowering tears. This experience taught me that big data—the data we capture—is going to be critical. It may reveal that our assumptions and anecdotal experience aren’t always right.”
6. How much diagnostic equipment do you need?
“Concerns about having to invest in equipment undoubtedly discourage many doctors from opening a dry-eye clinic,” notes Dr. Karpecki. “The tests and treatment options out there are excellent, and the companies obviously want us to buy them, but that doesn’t mean you have to have them to run a successful clinic.”
Dr. Sheppard points out that ophthalmologists already have the most important dry-eye diagnostic equipment. “The most important device is your slit lamp,” he says. “Then, you need fluorescein to stain the cornea. A topographer is important, but almost everybody has one.”
“In addition to doing a great exam and taking a thorough history and having the right dyes to stain the ocular surface, other equipment can be helpful,” notes Dr. Thompson. “Tools like the HD Analyzer can give you an objective tear-film breakup time. Many topographers can tell you a lot about the condition of the tear film, since the air-tear interface is what reflects the placido disc that helps provide you with the corneal curvature information. Often, an irregular topography indicates a dry eye.”
Dr. Karpecki says he’d recommend one piece of equipment beyond the recently available testing and treating technologies. “Having a slit lamp imaging system—essentially a slit lamp with a camera built into it—can be really helpful,” he says. “First, this gives you an easy and efficient way to show patients that they have a problem. Second, when I write down a staining score, I don’t know exactly what I saw when the patient returns. But if I have a picture of the staining, or a picture showing what the patient’s meibomian gland expression looked like, I’ll be able to tell how much they’ve improved.”
Dr. Epitropoulos agrees that a lot of equipment isn’t required for evaluating dry eye. “However, if you want to become a dry eye center of excellence, I think it’s important to incorporate the latest state-of-the-art technology,” she says.
“In terms of the higher-tech devices,” Dr. Sheppard notes, “you can invest in them one at a time if you’re inclined, such as an inflammation test, an osmolarity test or a meibography device like the LipiScan. Even if you decide you want to have all three, bringing them in all at once can become a headache because you have to learn to use them, as well as getting the billing straight. So if you’re going to purchase or adopt them, procure one technology at a time.”
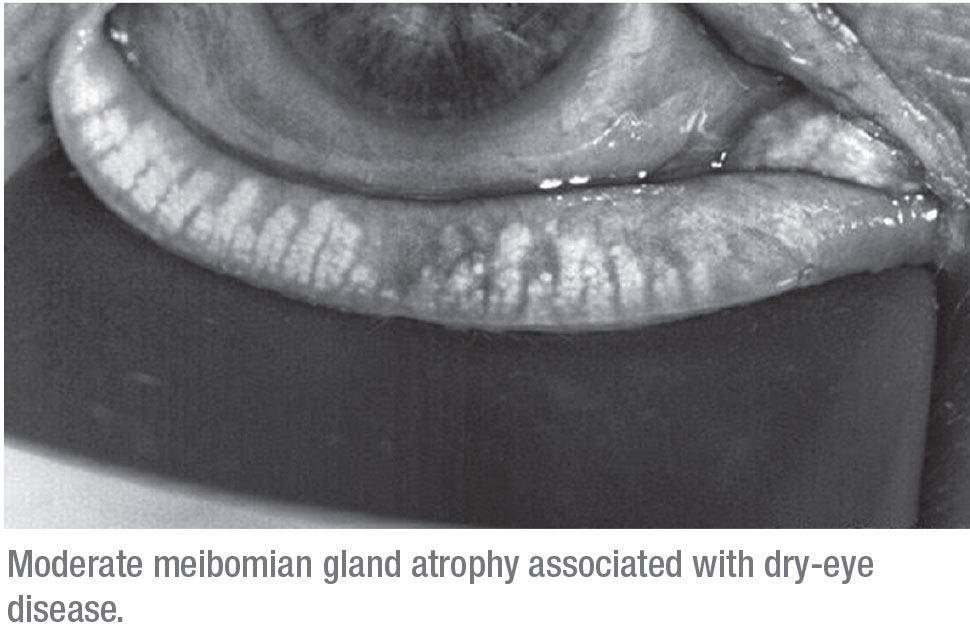
“Key pieces of equipment to have in your practice, in my opinion, include some kind of point-of-care testing, such as osmolarity or MMP-9 measurement, and meibography,” says Dr. Gupta. “I find meibography to be essential because meibomian gland disease is a significant contributor to dry eye. The images are crucial.”
 |
7. How much treatment technology do you need?
Dr. Karpecki says you don’t need to have every piece of high-tech equipment. “You probably need a debrider for the eyelid margins,” he says. “You should have 180-day dissolving punctal plugs, and the instruments designed to work with them. Then, you probably want to have a tool for expressing the oil glands. You can do that manually, or using a thermal pulsation or expression technology, low-level light therapy or IPL. You’ll need a device to clean the lid margins and remove the biofilm, such as Blephex, and access to amniotic membrane and autologous serum. I do think it’s useful to have at least one or two high-tech devices—at the very least to set yourself apart from other clinics.”
“I believe it’s good to have something that will help you treat the meibomian glands,” says Dr. Thompson. “I don’t believe in pushing on eyes after warming the eyelids, the way we used to teach people to do. I prefer to use devices that express the glands without pushing on the eye, like LipiFlow, which creates a ‘sandwich’ on either side of the eyelid to create the compression, or the TearCare system from Sight Sciences, where you warm the eyelid and then use forceps to express the meibomian glands.”
“Therapies such as LipiFlow, Bleph-ex, iLux and IPL really do help to optimize the health of the tear film, improve patient symptoms and improve surgical outcomes,” notes Dr. Epitropoulos. “Cynthia Matossian, MD, presented her data at the 2019 ASCRS meeting, which showed that thermal pulsation treatment prior to cataract surgery improves the accuracy of keratometry and subsequent surgical decision making.2 That’s been true in my practice as well.”
“You should approach this the same way you’d set up a LASIK practice,” says Dr. Sheppard. “With these new instruments you’re selling patients a cash procedure, and you can’t do that in a flippant way. You have to have a whole coordinated setup with a counselor, technicians, billing, a friendly, sales-minded scheduler and a patient credit program that lets patients pay for a procedure on credit, the same way they’d buy a car. Taking that step is a big decision.”
8. Should you advertise your clinic?
If you’re opening a dry-eye clinic, Dr. Thompson suggests a number of ways to spread the word. “Meet with your potential referring doctors and show them case presentations illustrating how you’ve helped patients with mild, moderate and severe dry eye,” he says. “Show how you’ve helped them not only deal with ocular surface issues, but also image-quality issues. We talk with local rheumatologists and internists and family doctors, because we know that patients with collagen vascular diseases like rheumatoid arthritis often have dry eye along with their systemic disease.
“In addition, you can include news about your dry-eye center in your patient newsletter,” he says. “Hold webinars. When new technologies or drugs are approved, send a press release to your local press media outlets. All of these strategies will help generate referrals and bring in new patients.”
Dr. Karpecki says it’s perfectly reasonable to do some marketing of your dry-eye clinic, especially using social media and similar avenues. “However,” he notes, “you have to be successful internally first, for two reasons: First, you already have that patient base, so there’s almost no expense involved. Second, being successful internally first gives you the chance to get really proficient with managing these patients before getting outside referrals. I’ve seen practices try to build referral ocular surface clinics without doing this; then the first few referrals didn’t turn out well, and they never got another referral.”
9. How do I get started?
Dr. Epitropoulos says many doctors ask her how to start a dry eye center of excellence. “If you’re thinking about building a dry-eye center, reach out and talk to other doctors who’ve done it,” she advises. “That way you don’t have to reinvent the wheel. Visit other dry-eye clinics to get a first-hand view of how a dry eye center of excellence is run. Consider taking courses, such as Dry Eye University in Jacksonville, Florida, set up by Frank Bowden III, MD. You can also take online courses and those offered at the major meetings.
“Another key to building a successful dry eye center of excellence is staffing,” she continues. “Doing this requires a team of trained, dedicated technicians. They also need to be caring and empathetic, because these patients are frustrated and often depressed about their disease; they often need someone to listen to them and understand what they’re going through.
“You also want to find a lead technician and coordinator to be your quarterback,” she notes. “This should be someone who can work with you and oversee your patient flow, workups, patient education and overall problem-solving. And if you’re going to participate in clinical trials for dry-eye treatments, you’ll also need to have an organized, efficient and experienced clinical research coordinator.
“Once you’re up and running, you’ll need to keep up with the latest technology for diagnosing and treating dry eye,” she adds. “And, it’s crucial to continuously educate both your patients and your staff. Having your staff visit other dry-eye clinics and attend courses will ensure that they’re well-educated about dry eye so they can communicate with patients effectively.”
10. Should I wait for the pandemic to end?
 |
“There are three good reasons to create your dry-eye clinic now, during the pandemic,” says Dr. Karpecki. “First, it takes a little time to get your system in place and understand patient flow. Since most of us are seeing fewer patients right now, that gives us more time to set this up and learn to make it work efficiently.
“Second,” he says, “the dry-eye patients coming in right now will be the more serious cases. They’ll require treatments like amniotic membrane, punctal occlusion and so forth, so they’ll generate more revenue for your practice than other patients might. That’s been the case in our clinic; our patient volume is down 15 to 30 percent, but because we’re seeing more significant cases, our revenue hasn’t dropped at all.
“Third,” he says, “no one can rely on insurance reimbursement alone, and dry-eye patients often need out-of-pocket procedures. In addition, we found that even during the COVID shutdown, our dry-eye patients continued to order products they needed from us, generating some additional revenue. Those are three good reasons to start a dry-eye clinic right now, rather than waiting for things to return to some semblance of normalcy after the pandemic is over.”
Dr. Gupta adds another point. “During the pandemic, the one population that’s been willing to come back into our clinic is our dry-eye patients,” she says. “So I wouldn’t wait for the pandemic to end to set up a dry-eye clinic, if you’re thinking about doing it.”
Making a Difference
“Millions of Americans suffer from dry-eye disease,” notes Dr. Epitropoulos. “These are some of the most frustrated patients I come across. A lot of them have suffered for years, and we’re their last hope. Really helping them is one of the most gratifying parts of practicing medicine for me—sometimes even more than performing cataract or refractive surgery.” REVIEW
Dr. Sheppard reports financial ties to Quidel, TearLab, TearScience and Johnson & Johnson Vision. Dr. Thompson is a consultant for Visiometrics, Johnson & Johnson Vision and TearCare. Dr. Karpecki consults for more than 40 dry eye-related companies. Dr. Gupta is a consultant for Johnson & Johnson Vision, TearLab and Quidel. Dr. Epitropoulos is a consultant for Allergan, Sun, Novartis, Johnson & Johnson Vision, PRN, BioTissue and Blephex.
1. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg 2015;41:1672–7.
2. Matossian C. Effect of Thermal Pulsation System Treatment on Keratometry Measurements Prior to Cataract Surgery. Presented at the annual meeting of the American Society of Cataract and Refractive Surgery, May 2019.
3. Trattler WB, Majmudar PA, Donnenfeld ED, et al. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: The effect of dry eye. Clin Ophthalmol 2017;11:1423-30.