Workup, Diagnosis and Treatment
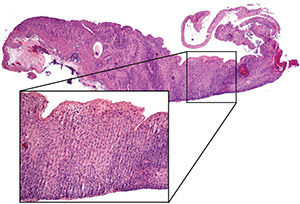 |
| Figure 2. Histopathology of excised limbus. Lower power mag- nification demonstrates the papillary configuration of squamous cells. Higher-power photomicrograph (inset) shows full-thickness epithelial replacement with dysplastic squamous cells with scant cytoplasm. The basement membrane is intact with no subepithe- lial spread, consistent with squamous cell carcinoma in situ. Photo by Ralph C. Eagle, MD |
Given the typical appearance of the lesion, ocular surface squamous neoplasia (OSSN) was the leading diagnosis. Treatment involved careful excision and intraoperative subconjunctival IFN according to the method described by Drs. Jerry and Carol Shields of the Wills Eye Ocular Oncology Service.1 The limbal conjunctiva was excised from 9 to 3 o’clock with 4-mm margins and alcohol-assisted removal of the corneal epithelium beginning 2 mm anterior to the extent of tumor, scraping toward the main lesion without direct manipulation of the tumor. A sample of Tenon’s fascia from 10 to 2 o’clock and an orbital biopsy at 10 o’clock were sent for staging. Cryotherapy was performed at all surgical margins. Subconjunctival injection of 10 million units of IFN was performed 360 degrees around the surgical margin.
Histopathology of the surgical specimens demonstrated papillary squamous cell carcinoma in situ at the limbus, with both Tenon’s fascia and the orbital biopsy negative for tumor (Figure 2). Postoperatively, treatment continued with monthly subconjunctival injections of IFN and topical IFN four times daily for four months.
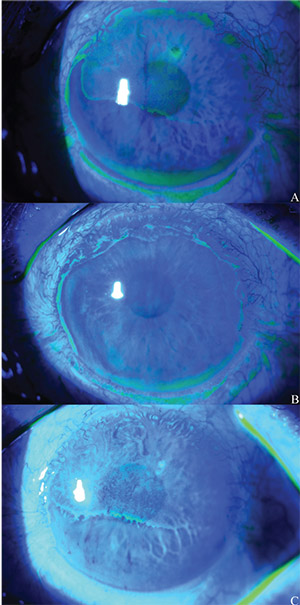 |
| Figure 3. External photo of the left eye nine months after limbus excision with corneal scraping, subconjunctival interferon injection and cryotherapy to the surgical margins (A). Fluorescein staining highlights irregular corneal epithelium covering about 60 percent of the surface. Photo of the left eye one week after selective epithelial debridement (B). At postop year one (C), fluorescein staining demonstrated recur- rence of the corneal epithelial irregularity. Photo by Cornea Service, Wills Eye Hospital |
At postoperative month six, the patient began to complain of blurred vision with intermittent monocular diplopia in his left eye. His vision at this time was 20/70 (PH 20/60) OS, and anterior segment evaluation revealed irregular corneal epithelium superiorly. Over several months, his vision deteriorated to 20/400 (PH 20/80), and the irregular corneal epithelium covered the superior 60 percent of his corneal surface (Figure 3A). When conservative treatment for presumed limbal stem cell deficiency (LSCD) with artificial tears and eyelid hygiene didn’t improve his symptoms or corneal appearance, selective epithelial debridement was performed.
Histopathology of the epithelial scraping revealed sheets of epithelial cells with focal collections of goblet cells; the increased cellularity of squamous cells with scant cytoplasm was suspicious for intraepithelial neoplasia. Given the history of multiple recurrences with concerning findings on histopathology, daily topical IFN was restarted. The ocular surface reepithelialized with healthy-appearing epithelium, and vision improved to 20/100 (PH 20/70) (Figure 3B). One year later, however, the corneal epithelial irregularity recurred (Figure 3C). At this time, daily topical interferon was restarted for a six-month course.
Discussion
Ocular surface squamous neoplasia is a spectrum of disease encompassing squamous dysplasia, intraepithelial neoplasia, carcinoma in situ and squamous cell carcinoma of the conjunctiva and cornea. It is typically unilateral and rarely metastatic, with risk factors including age (typically age 70 and above), male gender, Caucasian race, lightly pigmented iris, infection with HIV and HPV, and exposure to UV-B radiation.2 Although diagnosis is primarily made by clinical presentation and examination findings, histopathology is useful for confirmation and staging. Historically, OSSN has been treated surgically with excision and adjuvant cryotherapy and/or local chemotherapy. Recurrence may occur if neoplastic cells remain after excision.3
The patient in the present case had three recurrences prior to his presentation at Wills Eye Hospital. Two strategies for preventing recurrences were employed at this time: “no touch” surgery and adjuvant IFN therapy. With 4-mm wide conjunctival margins and alcohol-assisted removal of the corneal involvement 2 mm anterior to the extent of tumor, scraping toward the main lesion, the excision was broad without direct manipulation of tumor cells.1 Furthermore, IFN, both in its subconjunctival injection and topical drop forms, has demonstrated efficacy as an adjunct to surgery and as sole treatment for OSSN. In one study, five patients with histologically diagnosed OSSN responded with complete tumor control to topical IFN alone.4 Similar results were observed in a case series of 81 eyes with OSSN in which IFN with or without surgical excision and cryotherapy led to complete tumor control in 95 percent of cases, with a recurrence rate of 5 percent.5 Of note, in the 5 percent of recurrent cases, complete regression was achieved with further IFN and cryotherapy. Furthermore, there were minimal side effects in this cohort, with less than 5 percent of patients developing ocular surface irritation, a mild follicular reaction or hyperemia when IFN was administered topically. Finally, no patients developed LSCD, in contrast to topical chemotherapeutics such as MMC and 5-FU, which have been known to cause epitheliopathy and loss of limbal stem cells.2
Despite the low risk of ocular surface toxicity from IFN, this patient had numerous risk factors for developing LSCD, including multiple surgical excisions at the limbus, cryotherapy and prior chemotherapeutic application, in addition to the ocular surface neoplasia itself. In milder cases of LSCD – which some suggest may represent limbal stem cell dysfunction rather than true deficiency – conservative management with artificial tears, eyelid hygiene and medical therapy such as topical cyclosporine, topical corticosteroids or oral doxycycline can lead to restoration of a healthy corneal epithelium.6
In cases refractory to supportive care and medical management, surgery is often necessary. When less than half of the limbus is damaged, selective epithelial debridement can allow dividing epithelium from healthy limbal cells to regenerate over the debrided area faster than the process of conjunctivalization, leading to improvement in the ocular surface in the visual axis.7 In our patient, this intervention led to initial improvement in visual symptoms, visual acuity and the ocular surface examination. The histopathology of the epithelial scraping was concerning for possible recurrence of intraepithelial neoplasia; however, it’s unclear whether this represented true recurrence, since epithelial scrapings don’t have histologic features specific enough to diagnose OSSN. Furthermore, the area of epithelial irregularity involved only the cornea, while prior recurrences in this patient had occurred at the limbus and conjunctiva. Nevertheless, given this individual’s concerning history and the favorable risk-benefit profile of IFN, the decision was made to restart IFN.
A history of OSSN can complicate decisions regarding management of LSCD. In patients not responsive to medical therapy for LSCD, limbal stem cell transplantation (LSCT), including simple limbal epithelial transplantation (SLET), may be employed. Many surgeons, however, will delay LSCT for LSCD unresponsive to medical therapy in the setting of OSSN until a patient has been recurrence-free for months or years. There have been several reports of early intervention for LSCD, including one case describing simultaneous OSSN excision at the limbus and SLET to prevent postoperative LSCD after nine clock hours of limbus were removed.8 At two years of follow-up, the reported patient had no evidence of LSCD or recurrence of OSSN, but it should be noted that adjuvant MMC and radioactive plaque therapy were used after the initial surgery. Although early intervention may prevent complications of LSCD, introducing transplanted cell lines may add to diagnostic confusion of ocular surface changes and may further limit the ability to detect early recurrence of OSSN. The patient in the case presented here will require further monitoring and perhaps a repeat biopsy for more in-depth histopathologic analysis for neoplasia, given the recurrence of ocular surface irregularity. His complex clinical course serves as a reminder of the potential virulence of ocular surface squamous neoplasia and its complications.
1. Shields JA, Shields CL, De Potter P. Surgical management of conjunctival tumors. Arch Ophthalmol 1997;115:6:808.
2. Kiire CA, Srinivasan S, Karp CL. Ocular surface squamous neoplasia. Int Ophthalmol Clin 2010;50:3:35-46.
3. Holcomb DJ, Lee G. Topical interferon alfa-2b for the treatment of recalcitrant ocular surface squamous neoplasia. Am J Ophthalmol 2006;142:4:568-571.
4. Karp CL, Moore JK, Rosa RH. Treatment of conjunctival and corneal intraepithelial neoplasia with topical interferon á-2b1. Ophthalmology 2001;108:6:1093-1098.
5. Shields CL, Kaliki S, Kim HJ et al. Interferon for ocular surface squamous neoplasia in 81 cases: Outcomes based on the AJCC classification. Cornea 2013;32:3:248–256.
6. Kim BY, Riaz KM, Bakhtiari P, et al. Medically reversible limbal stem cell disease: Clinical features and management strategies. Ophthalmology 2014;121:10:2053-2058.
7. Jeng BH, Halfpenny CP, Meisler DM et al. Management of focal limbal stem cell deficiency associated with soft contact lens wear. Cornea 2011;30:1:18-23.
8. Mittal V, Narang P, Menon V, et al. Primary simple limbal epithelial transplantation along with excisional biopsy in the management of extensive ocular surface squamous neoplasia. Cornea 2016;35:12:1650-1652.



