An 82-year-old Caucasian male presented with a three-day history of decreased vision, redness and pain in his left eye. He denied any concurrent headache, diplopia, photophobia, purulent discharge, history of trauma or recent illness. Systemic review was not significant; the patient denied the presence of any rashes, joint pain, abnormal bowel movements or urinary symptoms. The patient initially presented to an outside emergency room two days prior to his presentation at Wills. He was diagnosed with bacterial conjunctivitis and placed on topical ciprofloxacin four times daily without improvement.
Medical History
Past medical history was significant for coronary artery disease, treated with the placement of two stents and a quadruple bypass surgery. Additionally, the patient suffered from myelodysplastic syndrome with isolated thrombocytopenia, hypertension, gastroesophageal reflux disease and hyperlipidemia. His family history was noncontributory. The patient was a former smoker; he drank alcohol socially and denied illicit drug use. He did not have any known drug allergies.
His medication list included: niacin 250 mg by mouth daily; lisinopril 5 mg by mouth daily; metoprolol 20 mg by mouth daily; isosorbide 30 mg by mouth daily; and aspirin 81 mg by mouth daily.
Examination
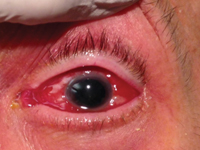
The patient’s vital signs were stable and within normal limits. Ocular examination demonstrated a best corrected visual acuity of 20/25 OD and 20/125 OS. External examination showed periorbital edema of the entire left upper and lower lid, erythema and ptosis (See Figure 1). Hertel exophthalmometry revealed 3.5 mm of left-sided proptosis.
|
Anterior slit-lamp examination of the right eye was normal, and revealed chemosis and injection of the conjunctiva of the left eye. The anterior chamber of the left eye was noted to be shallow. Gonioscopy revealed blood in Schlemm’s canal of the left eye. Intraocular pressure by Goldmann tonometry was 9 mmHg OD and 12 mmHg OS. Funduscopic examination of the right eye was normal. Funduscopic examination of the left eye exhibited peripheral elevations; a B-scan ultrasound was performed that confirmed the presence of choroidal effusions. Orbital ultrasonography demonstrated thickening of the retinochoroidal region with increased vascular flow, and choroidal elevations anterior, temporal and nasal to the optic disc consistent with choroidal effusions.
Please click this link for diagnosis, workup, treatment and discussion.