In surgery, as in life, the mind truly controls the body, and I teach my fellows all the time: “Your hands cannot do what your mind has not decided. Performing surgery should be a breeze—it’s the preoperative planning that should exhaust you.” If a patient is referred to you with a post-refractive surgery complication and you view his case as a difficult problem for which there is only one solution, such as corneal transplant, then you’ll never see the potential for better vision by way of a custom-designed procedure. If, however, you can change your mindset and see a complication as an opportunity to improve vision, then myriad options will open themselves up to you. Here, I’ll explain how to approach complications with a different point of view.
Formulating a Plan
The basis of my approach to managing complications is the attitude that every complication can be corrected to 20/20 vision, what I call Best Visual Potential. It’s not good enough to just make an attempt to correct a complication and leave the patient with somewhat better vision. You have to aim to correct the patient to the point where he’s truly seeing 20/20 or better. In that way, not only are you taking him from a bad situation to a satisfactory one, you’re taking him to an elevated level of vision. Along these lines, you have to constantly battle the urge to just do a default procedure such as penetrating keratoplasty—the procedure of least resistance—and be done with it. Though PK may be easy for you, it’s suboptimal for the patient, leaving him with less than 20/20 vision and a full-thickness wound that could potentially open up at any point during his lifetime. PK is the last resort.
Also, let the patient know your plan. By bringing a patient in on your surgical plan, he becomes your partner. He’ll also be impressed that even though you have access to textbook techniques such as PKP or lens exchange, you’d rather fight for his best vision using a plan that’s custom designed for his situation.
To help systematically approach complications, I created an algorithm, I refer to as the Five-S system:
• Sight. Is the patient correctable to 20/20 with glasses and/or hard contact lenses?• Scar. Is there a scar involved?• Strength. This point asks whether there is a thickness problem. Do you need to add tissue as in a lamellar keratoplasty (for ectasia), or remove it as in epikeratophakia?• Shape. Is the corneal shape affected? This is central to everything we do in refractive surgery.• Site. Is the problem central or peripheral?
There is no case that can’t fit into this 5S system, and the evaluation of these 5S attributes will unfold the blueprint for a unique approach to each case, either single or staged, which will move towards the patient’s BVP.
Putting the Plan into Action
Once you see a complication as a situation that needs to be dealt with rather than as an error or a headache, and approach it in a logical fashion, you’ll find things will become more manageable. Here are some examples of approaching common complications with this mindset.
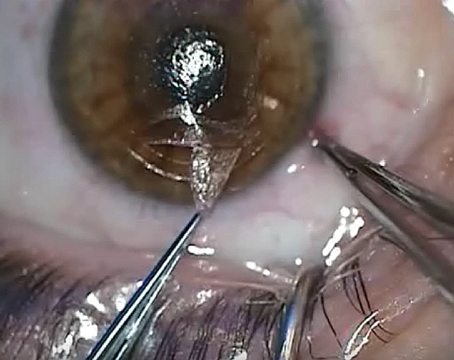
• Postop corneal scar. When a patient presents with a scar, it’s important to look at it from her perspective. She doesn’t come in and say, “Hey, doc, I’ve got a corneal scar to deal with.” Instead she simply says, “I can’t see.” The patient is asking for vision. This is why I emphasize the use of PRK, not PTK, for scars. PTK is the wrong concept because with it, you dig at the scar but damage the cornea’s shape. Since vision is determined by corneal shape, it’s better to shape the cornea with a PRK. The intended, fortunate side effect of this shaping is that the “shavings” that result from it are the scar tissue. I have numerous patients in whom you may still see the residual corneal scar but who see 20/20.
|
A 68-year-old patient came to me with a post-RK cornea scar. Every doctor he had been to told him he needed a penetrating transplant. However, using my 5S system to approach the scar and shape, I made a staged plan. Following my plan, I was able to easily peel the scar under the laser. Following that, I performed a myopic ablation and the patient immediately began crying beneath the laser, since he could finally see out of that eye. Since he was 68, after a period of stabilization, I performed cataract surgery and implanted a toric lens, and the patient now sees 20/20. Both surgeries were topical and brief and the eye looks as if no one has ever touched it.
• Post-LASIK ectasia. Though corneal ectasia isn’t trivial, it shouldn’t be viewed as a railroad that runs straight to a PK. In many cases, ectasia can be viewed as a case of a thin cornea with astigmatism in the 5S system. In ectasia cases in which the astigmatism is the main component but corneal thickness isn’t too bad, you can place Intacs in a directional pattern using an asymmetric combination, with a thick and a thin segment, including superficial and deep channels associated with a steep-axis technique. After about three months, you can perform PRK to bring the patient to his BVP.
However, if the patient has a very thin cornea, such as less than 200 µm, and maybe also has a scar, you can instead perform lamellar keratoplasty (in 5S terms, you’d add “Strength” and remove “Scar”). With this approach, you remove the LASIK flap and discard it and place the lamellae of a donor cornea that’s thicker than that being replaced. A thicker donor is preferable because it will deturgesce with time and also provide tissue for future laser PRK ablation. Six months later, return to the eye and do a PRK to get the patient to his BVP of 20/20.
• Multifocal intraocular lens nightmare. You can also take a stepwise approach to managing postop issues with premium IOLs. You may perform what I call “Optical Manipulation” with all types of IOLs, ICL, etc., and then use the cornea as a final vision rehabilitative platform. Alternately, you can clear the cornea to lead to more accurate biometry and then perform lens-based surgery.
For example, in one case I dealt with, a surgeon implanted a multifocal ReSTOR lens, but the patient ended up with a hyperopic surprise. The surgeon attempted to correct the refraction with LASIK but a corneal scar resulted, which the surgeon then tried to remedy with more laser, making the refraction worse. The surgeon also performed a YAG capsulotomy. When the patient presented to me, she was very depressed, could see only 20/200 best-corrected out of the eye, and wanted to sue the original surgeon.
Approaching the case, I saw that the scar was on-cornea, with false irregular, hyperopic astigmatism. I performed a laser ablation first to take care of the scar to achieve a clear and “measurable” cornea, and then waited three months to observe refractive stability at +6 D with 20/25 best-corrected vision. It’s at this point that you have to not settle for satisfactory, but push yourself to give the patient the vision that she was used to or better. Given this high hyperopia, I wanted a lens-based surgery, but since a YAG had been done the ReSTOR lens removal wouldn’t make sense. Therefore, I decided to leave the lens in place and add a piggyback lens on top of it, which brought the patient back to 20/20 vision, and lifted her spirits in the process.
In the end, treating complications is all about inflicting the least trauma (surgically and psychologically) and getting the BVP.
REVIEW
Dr. Gulani is in private practice.