|
"We've done cross-linking in more than 1,000 patients over the past six years, and find that most of our patients get very nice changes in corneal shape and an improvement in uncorrected and best-corrected visual acuity."
–William Trattler, MD |
• SMILE. Small-incision lenticular extraction is a surgical procedure performed with the Carl Zeiss Meditec Visumax femtosecond laser that creates a small lenticule of tissue within the stroma. The surgeon then extracts the lenticule through a corneal incision. The goal is to consolidate the refractive procedure into one surgery with one device and avoid the issues involved with creating a flap. SMILE is currently being studied in a U.S. Food and Drug Administration trial.
“We’re just about done with the spherical myopia trial— we’re not treating any astigmatism,” says John Doane, MD, of St. Louis, a principal investigator for the study. “We can treat from -1 to -10 D and the results look good so far. For my personal data, I’ve treated 90 patients. One eye of each patient got LASIK and the other SMILE. With the longest postop at over a year, I’ve yet to enhance either procedure. The effectiveness of the SMILE procedure seems to be as good as anything we’ve seen with LASIK. The stability is rock-solid, and the results we get at one month stay hat way. The safety is as good as anything we’ve done.”
One interesting aspect of SMILE that surgeons have commented on is how its predictability remains good even in higher levels of correction. “Looking at the international data, I was pretty sure that, for patients over -6 D, SMILE would be as good as anything we’ve seen,” Dr. Doane says. “And my personal data has borne that out. It also seems to be just as good as LASIK for low myopes. As to why this is, consider what happens when we do excimer laser, either PRK or LASIK. In those procedures, we’re opening the corneal stroma to the environment.
As such, we’re worried about temperature, humidity and barometric pressure—essentially the hydration effects on the stroma or Bowman’s layer. But when you do a SMILE procedure, it’s being done in a closed system, and all the energy is delivered within the cornea. This is one of the reasons that’s being discussed as a possible explanation why SMILE is better predictability-wise with higher myopes; with a high myopic LASIK that lasts 40 seconds or so, the amount of cornea dehydration that occurs may result in more tissue removal per pulse near the end of the procedure than when the procedure first started.”
The challenges to SMILE are hyperopic treatments—it currently doesn’t do them—and enhancements. “The vast bulk—85 percent—of my patients are myopic or compound myopic/astigmatism,” says Dr. Doane. “There may also be some mixed astigmatism. I personally don’t treat a lot of hyperopia in my practice, however. So, my thinking is if SMILE works for myopia or compound myopic astigmatism, that’s the bulk of the patients.
|
• Combined refractive surgery/corneal cross-linking. Several years ago, surgeons began attempting to fortify the cornea in certain refractive surgery patients with a riboflavin/UV light cross-linking procedure, and have reported stable results. Current bones of contention center on leaving the epithelium on vs. taking it off and whether or not to use a higher fluence and less energy duration.
“We combine collagen cross-linking as a prophylactic measure in routine LASIK cases for high myopes and in hyperopes and have published extensively on this modality, which is now commercially known as LASIK-Xtra,” says Athens, Greece, surgeon John Kanellopoulos. “In our practice, where it’s been applied for the last eight years, it’s a routine procedure. More than half our LASIK cases are now performed in conjunction with very high-fluence collagen cross-linking, specifically 30 mW applied for 80 seconds after pre-soaking the exposed cornea stroma for just 60 seconds. LASIK-Xtra has shown in our clinical practice—and we have reported—a significant advantage in hyperopic LASIK and a significant advantage in very high myopic LASIK, especially in younger patients; we see an increased stability in these patients and a reduced number of retreatments needed. We’ve not seen significant risks with the combination.”
|
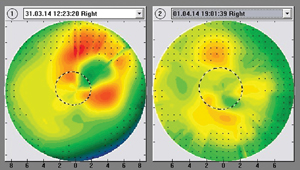
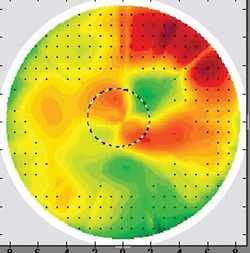
In cases of progressive keratoconus, Dr. Kanellopoulos says a
combination of topography-guided PRK—purely to normalize the corneal
shape rather than to try to perfect vision—and collagen cross-linking
has been helpful in more than 2,000 patients in his practice. He adds
that Avedro (Waltham, Mass.) is currently conducting trials for LASIK-
Xtra in the United States.
In terms of the future, Dr. Kanellopoulos says Avedro is currently developing a cross-linking treatment designed purely to create a refractive change, like LASIK without an excimer. “At our Athens center, we have been able to achieve the correction of small refractive errors—mild myopias, hyperopias and/or astigmatism—with only collagen crosslinking using a very sophisticated device, the KXL II, which has had a CE mark in Europe since 2013,” says Dr. Kanellopoulos. “This is very high-fluence collagen crosslinking, achieved through a specific pattern of UV light being produced and applied with a tracker on a cornea that has been pre-soaked with riboflavin, epi-off and epi- on. I think that this will be an area where the next page of refractive surgery may possibly concentrate on thousands, possibly millions, of people with very mild myopic errors.”
The CXL-USA surgeons are currently looking for funding for a new study, CXLO, which will look at the effects of conductive keratoplasty combined with corneal cross- linking performed a day later. “We’ll be looking at a combination of reshaping the cornea with CK and then locking that in with corneal cross-linking to achieve a better effect,” explains Dr. Trattler.
• Topography-guided laser vision correction. The ability to add topography guidance to a refractive surgery gives surgeons more flexibility in how they can approach refractive cases, especially for patients with corneal irregularities. Two topography-guided systems have been approved in the United States, one by Alcon and the other by Nidek, though they’re not yet in clinical use.
Dr. Kanellopoulos has worked with topography-guided systems for several years and thinks U.S. surgeons will appreciate their usefulness. “It is well-known that customized ablations have in the past employed wavefront-guidance,” Dr. Kanellopoulos says.
“But it is also well-known that wave- front imaging isn’t possible in a very high percentage of those cases as the very high irregularity of the cornea creates difficulties in reproducible wavefront measurements. So, topography-guided ablations have found great clinical application over the last decade internationally, outside the United States, in treating difficult cornea problems such as corneal scars, decentered laser ablations, high astigmatism and asymmetric astigmatism, and even to address mild keratoconus to an extent. We have published in numerous publications and book chapters on topography-guided incorporation within the Athens Protocol as a means to not only stabilize keratoconus but to dramatically improve visual function.” Dr. Kanellopoulos says the advantages of topography-guided ablations in comparison to wavefront- guided are that the cornea is easier to image and the images are more specific and sensitive. The topography-guided treatments can also flatten steep areas not only by treating the peaks of corneal curvature but by also treating around the troughs, allowing them to use about a third of the tissue that a wavefront-guided approach does. However, they have shortcomings, as well. “Topography-guided ablations only look at and diagnose cornea irregularities,” Dr. Kanellopoulos says, “and do not have the ability to incorporate in their planning other biometric data that would also make them very predictable in spherical refractive correction in these corneas, whereas wavefront-guided ablations would treat that as well from the get-go.”
REVIEW
|
"Topography-guided ablations have found great clinical application over the last decade internationally, outside the United States, in treating difficult cornea problems such as corneal scars, decentered laser ablations, high astigmatism and asymmetric astigmatism."
–John Kanellopoulos, MD |