Operating under the belief that where you start determines where you finish, refractive surgeons at this year’s ARVO meeting are doing a lot of research on screening prospective patients properly ahead of time to head off possible problems with ectasia and dry eye. However, they offer up some data on treatments, as well, for both surface ablation and LASIK. Here’s a look at their research. (Unless noted in the text, studies had no commercial support.)
Preop Considerations
Researchers at the University of Buenos Aires say that you might get more useful keratoconus screening data from the Ocular Response Analyzer by combining its measurement parameters, rather than focusing on each individually.
The research includes 95 eyes from 95 healthy subjects and 70 fellow eyes from 70 unilateral manifest keratoconus patients. Both groups were evaluated with ORA, corneal topography, aberrometry and anterior segment optical coherence tomography. The researchers studied the groups’ corneal hysteresis, corneal resistance factor and 41 other biomechanical parameters. They used linear regression to correct for the effect of central corneal thickness on correlated parameters, and they assessed diagnostic performance by receiver-operating characteristic curve analysis.
The investigators say that 29 of the 41 additional biomechanical parameters, along with CH and the CRF, showed statistically meaningful differences between the groups (p<0.05). Six parameters, including CH and CRF, were significantly correlated with CCT in both groups. The researchers note that the CRF, Time-In, H2, H21 and Dive2 had the best performances (area under the curve), and that only the CRF was improved after correcting for CCT. What they found interesting is that combinations of these parameters had better diagnostic yields (an error rate of less than 20 percent) than when the parameters were considered individually, with the highest yield coming from a combination of the 10 best parameters (AUC=0.82). They say these results also applied to eyes with normal higher-order 5-mm anterior corneal surface aberrations (<0.344 µm, taken from mean +1 SD of group 1)—outperforming corneal topography.
Ultimately, the researchers say that biometric analysis with multiple parameters on the ORA can detect a higher proportion of eyes with subclinical keratoconus than corneal topography alone, and with a better diagnostic yield than CH or CRF individually.1117
The same group of Argentinean researchers also took a look at the pros and cons of using the Pentacam vs. the ORA for preoperative screening, and found that each one compensates for the other’s shortcomings.
Using corneal topography, the Pentacam and the ORA, the investigators evaluated 19 eyes from 19 healthy subjects (group 1) and 30 eyes from 30 unilateral manifest keratoconus patients (group 2). In group 2, the eye with the lowest average corneal power was recruited for the study. The investigators compared Pentacam-reported indices for posterior corneal elevation (Db), pachymetric progression (Dp) and overall keratoconus findings (D) with ORA-derived CRF (DifCRF, corrected for corneal thickness) and CH-CRF.
The groups weren’t different in mean age (mean: 30.9 ±10.6 vs. 31.3 ±12.2 years) or central corneal thickness (512.6 ±26 vs. 496.9 ±34.6 µm) but the average corneal power was higher in group 2 eyes (43.90 ±1.93 vs. 45.66 ±3.17 D, p<0.05). Pentacam’s Db, Dp and D indices (positive >2) had 94.7 percent, 89.5 percent and 89.5 percent specificity and 50 percent, 50 percent and 66.7 percent sensitivity, respectively. ORA’s DifCRF (positive <-0.695) and CH-CRF (positive >0.95) indices showed 78.9 percent and 57.9 percent specificity and 86.7 percent and 53.3 percent sensitivity, respectively. The physicians add that either D or DifCRF indices were positive in 93.7 percent of group 2 eyes, with 68.4 percent combined specificity.
Looking over all the data, the researchers say that the ORA-derived index DifCRF has a higher sensitivity for subclinical keratoconus eyes but falsely flags healthy corneas more often than Pentacam’s indices do, with the latter indices showing a high specificity. They think that an approach combining both methods could markedly increase sensitivity while sacrificing some specificity, which the researchers deem is a tradeoff that’s probably acceptable when screening refractive surgery candidates.6798
Investigators at Utah’s Moran Eye Center say there are some differences in measurement methods to be aware of if you attempt to calculate patients’ white-to-white corneal diameter preoperatively before implanting an intraocular lens.
In the study, researchers measured the WTW diameter and the anterior chamber depth of 38 eyes (19 patients) using four instruments: the Zeiss Meditec Atlas; Zeiss IOLMaster; Orbscan II; and the Pentacam. The mean horizontal corneal diameter measurements were 12.41 ±0.35 mm with the Atlas, 12.13 ±0.31 mm with the IOLMaster, 11.79 ±0.30 mm with the Orbscan II and 12.06 ±0.78 mm with the Pentacam. The physicians found significant differences in the mean WTW diameter between the Atlas and IOLMaster (p<0.01), Atlas and Orbscan (p<0.01), Atlas and Pentacam (p<0.02) and IOLMaster and Orbscan II (p<0.01). The best 95-percent limits of agreement were for the IOLMaster and Pentacam (-1.30, 1.43; r=0.76, p<0.01).
Mean ACD measurements were 3.55 ±0.31 mm for the IOLMaster, 3.51 ±0.28 mm for the Orbscan II and 3.02 ±0.30 mm for the Pentacam. Significant differences in ACD were found between the IOLMaster and Pentacam (p<0.01), and the Orbscan II and Pentacam (p<0.01).4036
In a prospective study from Mexico, researchers took anterior chamber depth measurements using various systems to get a feel for their accuracy.
The investigators analyzed 84 eyes of 42 patients with the Orbscan II (scanning-slit technology); the Pentacam, Galilei and Sirius systems (Scheimpflug imaging systems); and the Visante OCT and IOLMaster (laser interferometry). To assess the intraobserver, interobserver and interdevice reproducibility of the five systems, the two independent observers examined all the eyes twice, and the reliability coefficient was calculated using Cronbach alpha-test.
The mean ACD were as follows: 2.94 ±0.31 μm (Orbscan); 3.08 ±0.32 μm (Pentacam); 3.16 ±0.29 μm (Galilei); 3.10 ±0.31 μm (Sirius); 3.13 ±0.30 μm (Atlas/Visante) and 3.48 ±0.65 μm (IOLMaster). The researchers say intraobserver and interobserver Cronbach alpha-tests showed a very good reliability coefficient (greater than 0.90) in all the measurements in all the systems. They say, however, that when using the Pentacam as reference, the interdevice reliability coefficient was very good for the rest of the devices (greater than 0.90) but low for the IOLMaster (less than 0.70).4037
Researchers at the University of South Carolina say that preop punctal occlusion in contact lens wearing dry-eye sufferers leads to fewer dry-eye complaints after laser-assisted sub-epithelial keratectomy.
The team conducted a retrospective review of 72 eyes of 36 patients who underwent LASEK over a three-year period. All 36 patients were contact lens wearers. The researchers separated the patients into two cohorts: contact wearers who tested positive for dry-eye syndrome with Schirmer’s I testing and received preoperative punctal occlusion, and those who didn’t receive punctal occlusion. A control group was composed of lens wearers who tested negative for dry-eye syndrome on Schirmer’s I testing and didn’t receive preoperative punctal occlusion. After undergoing, LASEK, the patients completed a dry-eye questionnaire to identify complaints of continued dry-eye syndrome.
Postop, a review of the data showed that of the eight patients in the contact lens group who tested positive for dry-eye syndrome and received punctal occlusion, two (25 percent) had postoperative dry-eye complaints at an average follow-up of 4.6 months. Of the five patients in the contact lens group who tested positive for dry eye and didn’t receive punctal occlusion, two (40 percent) had postoperative dry-eye complaints at an average of 5.6 months. Of the 23 patients in the contact lens group who tested negative for dry eye and didn’t receive punctal occlusion, eight (35 percent) had postoperative dry-eye complaints at an average of 5.2 months.
The researchers say that their findings seem to indicate that in contact lens wearers who undergo laser vision corrective surgery and test positive for dry-eye preoperatively, the rate of postoperative complaints will be less if they have preoperative punctal occlusion. They add that it might help postop patient satisfaction if this information on punctal occlusion were included in preoperative counseling.4043
In an effort to enhance the accuracy of refractive surgery and toric intraocular lens outcomes, surgeons from Chicago developed a novel way to approximate the effect of patient intraoperative head tilt on cyclotorsion measurements.
In the study, physicians measured the direction and degree of cyclotorsion in 110 eyes of 55 patients undergoing bilateral sequential laser refractive surgery. Preoperatively, they used the Visx WaveScan system to record an iris image of each eye with the patient seated. They then compared this image to one obtained immediately prior to laser ablation, when the patient was supine and situated beneath the laser. The investigators calculated presumed head tilt for each patient by calculating the average cyclotorsion of both eyes. They operated under the assumption that if both eyes of the same patient rotated the same amount in the same direction (clockwise or counter-clockwise) the amount of cyclotorsion measured was entirely due to head tilt. They calculated the adjusted cyclotorsion by subtracting the presumed head tilt for each eye of the same patient.
For the unadjusted data, 41.8 percent of patients had bilateral excyclotorsion, while only 10.9 percent had bilateral incyclotorsion. The number of patients with comitant rotations was 30.9 percent CCW and 16.4 percent CW. After adjusting for presumed head tilt on an individual basis, 70.9 percent of patients had bilateral excyclotorsion, while only a quarter had bilateral incyclotorsion. No relative movement was observed in 3.6 percent. Researchers say the average presumed head tilt was 0.83 degrees CCW (SD: 2.6 degrees) and ranged from 6.85 degrees CCW to 5.25 degrees CW.
The physicians say that the physiological basis for the fact that a majority of the patients had bilateral excyclotorsion between seated and supine positions after adjusting for presumed head tilt is unclear, though they theorize that it may be related to the decreased relative tone of the incyclotorting muscles relative to the excyclotorting muscles in the supine position, or to the placement of a lid speculum causing slight excyclotorsion. The researchers add that, given that primary eye positioning is difficult to guarantee, they recommend bilateral cyclotorsion measurements for unilateral refractive surgery, as well as for toric IOL implantation. They think additional analysis with more patients would foster a more definitive conclusion.5570
Treatment Efficacy
Patients and surgeons alike may take comfort in the fact that it appears that PRK for a range of myopia produces a good result for almost 20 years after surgery.
Researchers in Denmark recently completed follow-up (r: 16 to 19 years) on 172 eyes of 107 PRK patients. One hundred forty eyes had low myopia (less than 6 D) and 32 had myopia of 6 D or greater. The preoperative mean spherical equivalent refraction for all eyes was -4.4 ±2.1 D (r: -1 to -10.8 D). At follow-up, eyes with low myopia had a mean difference between attempted and achieved SE refraction of -0.7 ±1.1 D (r: +1.1 to -6.9 D), and eyes with high myopia were -1.2 ±2.3 D (r: +1.0 to -10.8 D) of target. For all eyes, 51 percent were within 0.5 D of the target SE refraction, 74 percent were within 1 D, and 91 percent were within 2 D. Mean uncorrected distance visual acuity was 0.14 ±0.33 logMAR (a little worse than 20/25 Snellen) (r: ~20/500 to 20/12) and mean best-corrected distance vision was -0.09 ± 0.09 logMAR (about 20/16) (r: ~20/63 to ~20/12).
Eight percent of eyes with low myopia and 16 percent of eyes with high myopia had visible haze of grades 0.5 to 2. Three percent of all eyes had undergone PRK enhancements due to myopic regression. A total of two eyes had lost two or more lines of best-corrected vision at follow-up, and eight eyes had gained two lines. Mean central corneal thickness was 524 ±34 µm (r: 402 to 610 µm). The surgeons say there have been no signs of ectasia.5571
Surgeons from Denmark say the relatively new SMall Incision Lenticule Extraction procedure can be effective once a surgeon surmounts its learning curve. One of the researchers received financial support from Carl Zeiss Meditec.
In the prospective study, 379 eyes of 198 patients underwent the SMILE procedure and were followed for three months. The average preop SE was -7.28 D (r: -13.13 to -1.63 D). Three hundred thirty-two eyes completed the three-month follow-up.
For eyes with emmetropia as their target refraction, 83 percent had an uncorrected distance acuity of 20/25 or better one day after surgery, which increased to 91 percent at three months. Nine eyes (2.7 percent) lost two or more lines of vision, and 42 (12.6 percent) eyes lost one line. The surgeons say that loss of best-corrected vision was mainly caused by interface scatter, and mostly occurred during treatment of the initial 100 eyes. Comparing attempted vs. achieved correction, the proportion of eyes within 0.5 D was 77.1 percent, and 94.3 percent were within 1 D. The difference in attempted vs. achieved SE correction was -0.13 ±0.49 D (r: 1.50 to -1.88 D). The researchers say 95 percent of the patients said they would recommend refractive surgery to others.5575
|
French researchers have found that PRK can be safe and effective in patients with suspected keratoconus, as long as the patients are chosen carefully.
In the study, surgeons identified 42 patients (62 eyes) who had been classified as keratoconus suspects or as having keratoconus by the corneal navigator function of the Nidek OPD-Scan II, and who had also undergone PRK with the Nidek EC5000 between 2004 and 2007. The mean preop SE was -3.96 ±0.92 D. The average central pachymetry was 529.4 ±32.8 µm (the mean thinnest point was 522.1 ±33.6 µm) and the mean simulated keratometry was 45.75 ±1.75 D. The average follow-up in the study is 4.8 ±1.4 years. Over the follow-up period, the average SE was -0.53 ±1.35 D, with an average postop K of 42.9 ±2.4 D. Only two patients had to wear glasses because of myopic regression, and there were no cases of corneal ectasia over the follow-up period.1475
In a controlled, prospective trial sponsored by the U.S. Department of Defense, researchers from the Army’s Refractive Surgery Research Center, Walter Reed National Military Medical Center and the Wilmer Eye Institute found that wavefront-optimized PRK results in corneas with better optical quality than WFO LASIK.
In the study, 143 patients with myopia or myopic astigmatism underwent WFO PRK (n=73; 146 eyes) or WFO LASIK (n=70; 139 eyes). The surgeons performed epithelial debridement with the Amoils brush in PRK, and for LASIK the superior-hinged flaps were made with the Intralase. All ablations were performed with the Alcon Allegretto Wave Eye-Q 400-MHz laser. To assess optical quality, the surgeons used the surface regularity index, surface asymmetry index and irregular astigmatism index. Repeated measures analysis of variance was used to compare WFO PRK to WFO LASIK. PRK eyes treated with mitomycin-C were excluded from the analysis and a P value <0.05 was considered significant.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
To help give refractive surgeons a handle on what’s going on during their treatments, surgeons from the University of Utah did a study to determine the ratio of keratometric change to refractive change in myopic ablations.
The researchers reviewed the charts of 2,738 eyes of patients who underwent LASIK or PRK between March 2007 and March 2010. The analysis involved comparing 1,020 eyes with a refractive change of 0 to 2.99 D (low refractive change) to 1,253 eyes with a refractive change of 3 to 5.99 D (moderate refractive change) and with 456 eyes with a refractive change greater than 6 D (high refractive change). Significant differences were found in the ratio of keratometric change/refractive change between eyes with low refractive change vs. moderate refractive change (0.98 ±0.60 vs. 0.80 ±0.17, p=1.02 x 10-25); moderate refractive change vs. high refractive change (0.80 ±0.17 vs. 0.77 ±0.11, p=1.01 x 10-14); and low refractive change vs. high refractive change groups (0.98 ±0.60 vs. 0.77 ±0.11, p=4.55 x10-4). The surgeons say the equation that best predicts the postoperative K prior to surgery was found to be K=x-(y*z), where x=preoperative K; y = -0.264*ln(attempted refractive change) + 1.1788; and z=attempted refractive change.
In the final analysis, the researchers say the change in simulated K required to achieve a diopter of myopic refractive correction decreases as the amount of refractive change increases, is more variable with lower amounts of correction, more constant with higher amounts of correction, and follows a non-linear relationship.1492
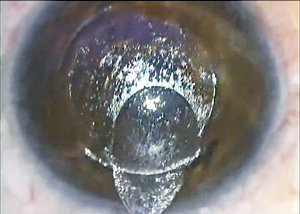
In a small retrospective study, surgeons from New York have found that the LenSx femtosecond laser can produce good results with astigmatic keratotomy after penetrating keratoplasty.
Fourteen patients were included in the study. In each patient, the surgeons created a pair of relaxing arcuate incisions on the steep corneal meridian as defined by a topographic map. For less than 4 D of astigmatism they used two 40-degree incisions; for 4 to 6 D two 50-degree cuts; and for more than 6 D the surgeons made two 60-degree incisions. Using the femtosecond laser and with the aid of topical anesthesia, the physicians made the pair of arcuate incisions within the corneal graft at a diameter of 6.5 mm and depth of 85 percent of the graft thickness as measured by the laser’s own intraoperative optical coherence tomography imaging system.
The mean preop subjective astigmatism was 9.59 ±2.8D. On the first day after the treatment the mean subjective astigmatism was 5.3 ±1.7 D, (p=0.0005) with an average reduction of 44 percent. At week one post treatment the mean subjective astigmatism was 4 ±1.25 D (p=0.0001), with an average reduction of 52.5 percent. Best-corrected visual acuity preoperatively was 0.67 ±0.23 logMAR (~20/100). It was 0.51 ±0.33 (~20/63) (p=0.025) on day 1 and 0.49 ±0.33 (~20/60) (p=0.016) at week one. Age, gender and etiology of PK had no effect on final outcome. Surgeons say the only adverse finding was mild worsening of the dry-eye symptoms observed in six patients in the immediate postoperative period. No infections or other postoperative complications were noted. The surgeons hope to create a precise nomogram and a predictable algorithm for LenSx AK incisions in the future.1503
|
The researchers reviewed 61,561 consecutive LASIK procedures and identified 335 eyes that required a flap re-lift to address striae (incidence: 0.54 percent). Of these, 42 percent were in the right eye, 39 percent in the left and 19 percent were bilateral. In 6.3 percent of the cases, surgeons needed to perform an additional relift and irrigation. The average time to re-lift was 2.7 ±9.9 days after LASIK, with 95 percent occurring within a week postop. Most of the eyes, 246, had a follow-up of at least three months.
In terms of risk factors, 80 percent of the eyes had flap diameters of 9.5 mm, with the rest having 8.5-mm flaps. Sixty-five percent of the flaps were created with a Hansatome microkeratome with the Z16 head, and the rest were made with the Z18 head. About half, 52 percent, had both a 9.5-mm flap and the use of the Z16 head, meaning larger and thinner flaps were at increased risk. The researchers found that surgeons with less experience, defined as having performed fewer than 1,000 LASIK procedures, had a higher incidence of re-lift (1.75 percent) than surgeons with intermediate experience (1,000 to 5,000 surgeries, re-lift incidence of 0.91 percent) or high experience (more than 5,000 surgeries, re-lift incidence of 0.47 percent).
The average spherical equivalent refraction before the re-lift was 0.21 ±0.52 D, which improved to -0.05 ±0.4 D (p<0.001) after the re-lift. Ninety-eight percent were within 1 D, and 87 percent were within 0.5 D, of the intended correction after re-lifting, compared to 96 and 81 percent before the re-lift. Ninety-eight percent of the eyes saw 20/40 or better, and 65 percent saw 20/20 or better, after the re-lift, vs. 82 percent who saw 20/40 and 25 percent who saw 20/20 before the intervention. The uncorrected distance vision was 0.2 ±0.3 logMAR (20/32) before re-lifting, and 0.1 ±0.1 logMAR (20/25) after the re-lift. Before the re-lift, 8.5 percent of eyes had lost three or more lines of best-corrected vision, 10.4 percent lost two and 31.6 percent lost one line. After re-lifting, no eyes lost more than two lines, 0.4 percent lost two lines and 5 percent lost one line.5572
Presbyopia Approaches
Researchers from London, one of whom is a consultant for Carl Zeiss Meditec, studied the effect of blended vision on presbyopes, and the effect the induced higher-order aberrations have on distance vision and contrast sensitivity.
The retrospective study included 96 myopic eyes (mean spherical equivalent: 4.19 ±2.29 D) and 341 hyperopic eyes (mean SE: +2.46 ±1.26 D) that underwent the laser blended vision treatment using the MEL80 excimer laser for the refractive ablation and the VisuMax femtosecond laser for the flap (both from Carl Zeiss Meditec). The laser blended vision technique involves correcting the dominant eye for sharpness at both intermediate and distant ranges of vision and the non-dominant eye for sharpness at near to intermediate ranges. It induces negative spherical aberration to try to increase depth of field. The researchers performed correlations between postop spherical aberration and postop distance-corrected near vision, between postop higher-order root mean square values of aberrations and postop DCNV, and between postop HORMS and the change in contrast sensitivity.
After the surgery, the average DCNV improved by 0.71 ±1.45 lines in the myopic group (p<0.001) and by 0.85 ±1.4 lines in the hyperopic group (p<0.001). In the myopes, DCNV was better for higher SA (R-squared: 0.047, p=0.035) and higher HORMS (R-squared: 0.046, p=0.031).
In the hyperopic group, DCNV wasn’t directly correlated to SA (R-squared: 0.008, p=0.100); however DCNV was better for higher HORMS (R-squared: 0.045, p<0.001). The researchers say that there was no statistically significant change in CS at 3, 6, 12 or 18 cycles per degree in either group. In the myopic group, the CS wasn’t altered by increasing HORMS, while in the hyperopic group there was a small reduction of 1 CS patch per 0.88 μm of HORMS at 12 cpd and 1 CS patch per 0.71 μm of HORMS at 18 cpd.
The researchers note that an increase in HORMS improved DCNV in both groups, and SA was correlated with DCNV in myopia. In hyperopia, they say that the finding that the correlation between DCNV and SA wasn’t statistically significant might be explained by larger angle kappas and the fact that wavefront measurements are conventionally calculated at the center of the entrance pupil, while in this study the ablation was centered on the corneal vertex, meaning that spherical aberration would produce “wavefront coma.” They plan to perform further studies of the treatment based on corneal topographic wavefront changes.5573
|
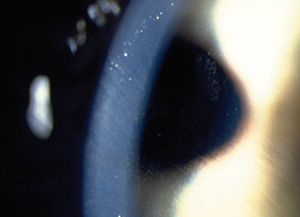
The researchers describe the mechanism of the inlay as alleviating the symptoms of presbyopia by extending the eye’s depth of focus through small-aperture optics. Following monocular implantation over a patient’s coaxially sighted corneal reflex, the opaque inlay, which has an overall diameter of 3.8 mm and a central aperture of 1.6 mm, only allows focused light rays to reach the retina, thereby increasing the eyes’ depth of focus, the investigators explain.
In the study, nine subjects received the implant in their non-dominant eyes. The researchers then studied the patients’ acuities as well as their visual fields, specifically using the indices of pattern standard deviation, fixation losses, false positives and false negatives.
Mean uncorrected distance acuity at baseline was 47.7 ±6.1 letters; postop it was 47 ±6.9 letters (p=0.30). The average best-corrected vision at baseline was 52.7 ±3.2 letters, and the study doctors say it wasn’t significantly different from the postop best-corrected vision of 51 ±4.5 letters (p=0.09). Uncorrected near acuity improved from an average of 26.7 ±3.6 letters to 44.1 ±7.2 letters postop (p<0.001).
In terms of the visual field indices, PSD at baseline in the implant eye was 1.37 ±0.25 and in the non-implant eye it was 1.53 ±0.61db (p=0.36). After surgery it was 1.58 ±0.36 in the implant eye and 1.52 ±0.38db (p=0.54) in the non-implant fellow. Automated perimetry reliability indices weren’t significantly different between eyes at baseline and after inlay implantation, the researchers say.1391 REVIEW
Dr. Probst is national medical director for TLC The Laser Center.