If cold comfort is better than no comfort, then the report on high volume LASIK surgeons contained in this year’s survey of the U.S. members of the International Society of Refractive Surgery may be comforting. Though the percentage of surgeons doing high-volume LASIK hasn’t increased, it hasn’t decreased either, which some may take as a sign that better times are on the horizon. Results from other areas of refractive surgery, from phakic lenses to the use of monovision, stayed similarly consistent with recent surveys, as well.
In this article, Mobile, Ala., surgeon Richard Duffey, a co-administrator of the survey, discusses trends he sees in the data, the possible reasons for surgeons’ choices, and a couple of surprising results.
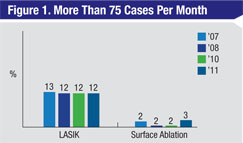 |
Dr. Duffey has been conducting the survey with Palm Springs, Calif., ophthalmologist David Leaming for 15 years, and Dr. Duffey says he always looks to the percentage of high-volume surgeons (surgeons who say they perform 75 or more LASIKs per month) as a barometer for the health of the LASIK market. “Lately, I would look at it and ask, ‘How much is it dropping?’ ” he says. “The percentage of high-volume surgeons on the survey has declined since 2001, when it peaked at 27 percent. However, what’s interesting is that, in the last three years, it’s kind of bottomed out, staying at 12 percent. I think we may be at the bottom of the statistical ‘U’ now, so maybe we’ll actually see these volumes start to go up again in the near future.”
In terms of what surgeons prefer as a treatment for myopia over -10 D, 48 percent say they would perform laser vision correction; 39 percent would implant a phakic intraocular lens. As for the rest of the responses, 6 percent would wait, 3 percent say they never operate on such patients and 2 percent would perform a refractive lens exchange procedure.
Interestingly, breaking down the LVC procedures, the percentage of surgeons saying they prefer surface ablation for these patients increased from 15 percent last year to 20 percent on this year’s survey, while LASIK went down by the same number of percentage points. “It’s interesting that only 39 percent of the surgeons say they’d implant a phakic IOL in these patients,” says Dr. Duffey. “We talk a lot about using phakic IOLs for high myopes, but it looks like, with all things being equal, the membership still prefers LVC.
“Personally, I still favor LVC,” adds Dr. Duffey. “I like extraocular procedures. I also think there’s an increasing trend toward surface ablation in high myopes to lessen the risk of thinner residual stromal beds and ectasia.”
The surgeons on the survey go in the other direction when it comes to high myopia. “The preferred procedure for the 5-D hyperope is refractive lens exchange, as it has been for years,” says Dr. Duffey. “It illustrates the point that, somewhere between 3 and 4 D, there’s a cutoff at which surgeons will probably prefer a lens-based procedure for hyperopia as opposed to a laser-based one. When you get into the higher degrees of hyperopia, patients don’t do as well. In these cases, centration, long-term stability, dry-eye complaints and quality of vision are bigger issues.”
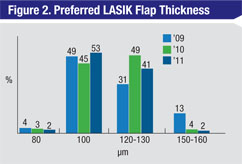 |
For the first time in the history of the survey, more than half of the respondents say they prefer a 100-µm flap or thinner. Two percent preferred an even thinner, 80-µm flap. (All of the preferred flap thicknesses appear in Figure 2.) “This is a first, because in previous years most surgeons chose 120 to 130 µm,” says Dr. Duffey. “And if you go back to 2004, it was a flap between 150 µm and 160 µm that was preferred.” Though the flap thickness has gotten progressively thinner, it may be reaching the physiological limit. “If we start hearing of physicians doing 60-µm flaps, we’ll include that on the survey. But the issue is the epithelium can be from 40 to 60 µm thick, so no one is going to want a flap that’s less than that, unless it’s an epithelial flap like in LASEK. So, in my opinion, 80 µm is as low as you can go and still routinely have a little bit of stroma on that flap.”
Along the same lines as the flap results, this year’s survey was also the first in which respondents preferred 300 µm of residual stromal tissue. The seven-year trend of more surgeons using the femtosecond laser to make flaps continued this year, with 57 percent of the surgeons saying it’s their preferred method.
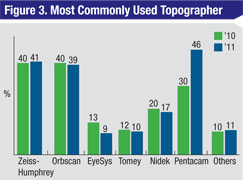 |
After hovering around 30 percent or lower over the past four years, 46 percent of the surgeons say the Pentacam is the topographer they use most commonly, with the next highest choices being the Zeiss-Humphrey device (41 percent), the Orbscan (39 percent) and the Nidek (17 percent). Though Dr. Duffey can only speak for his own practice, he says he also found himself switching to the Pentacam because his previous unit, though useful, didn’t meet the Digital Imaging and Communication Standards in Medicine, which are set by a committee who are members of the National Electrical Manufacturers Association. The DICOM standards seek to set a file format and communications protocol that can be standardized so all medical imaging devices can share data. “My previous topographer wasn’t DICOM-approved for electronic medical records,” he says. “I needed to get a device that could scan images and send them back and forth electronically in my records system. Beyond that, I think some surgeons feel there are some advantages to the Pentacam, such as indices like the Belin-Ambrosio maps for detecting corneal irregularities. It also has the flexibility to let you perform imaging of the anterior cornea, the angle and the lens.”
Dr. Duffey has already begun thinking about what questions to ask on next year’s survey, always keeping in mind that when he adds a question to the list, he has to take a question off in order to keep the entire questionnaire easy for the physicians to respond to. “Corneal cross-linking was identified at a meeting as something we may need to start looking at,” he says. “And we may change the way we approach the use of corneal inlays and presbyopic LASIK on the survey, both of which are getting closer to Food and Drug Administration approval.”