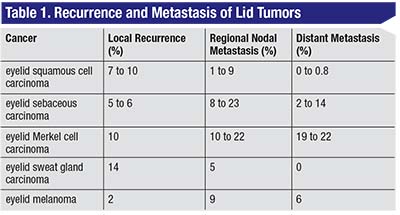
The investigators performed a systematic review of the literature using the terms “AJCC (American Joint Committee on Cancer),” “eyelid,” “carcinoma” and “melanoma.” The rates of local recurrence, regional nodal metastasis and distant metastasis appear in Table 1.
The researchers say
 |
Ophthal Plast Reconstr Surg 2017;33:5:317-324.
Ford J, Thakar S, Thuro B, et al.
Diabetes and DMEK
Researchers reviewed a consecutive, single-center case series of Descemet’s membrane endothelial keratoplasty to determine the effect of diabetes on both hosts and donors.
In 504 of 1,791 cases (28 percent) the donor had a history of diabetes, and the recipient had such a history in 14 percent of cases (250 corneas). For donors without diabetes vs. those with the disease, the preparation success rate was 99 percent versus 95 percent (p<0.0001), the air reinjection rate was 16 percent versus 18 percent (p=0.19), and the four-year graft replacement/failure rate was 7 percent versus 9 percent, respectively (p=0.15). The investigators say that endothelial cell loss wasn’t associated with donor diabetes (p=0.76). For recipients without and with diabetes, in addition to the replacement/failure rate mentioned above, the median endothelial cell loss increased from 27 percent versus 29 percent at one month to 42 percent versus 48 percent at four years, respectively (p=0.02). Recipient use of insulin therapy was associated with poorer graft attachment and a higher air reinjection rate (p=0.0023).
The researchers say that although donor diabetes was associated with a fivefold increased risk of tissue preparation failure, it wasn’t significantly associated with air reinjection, graft survival or endothelial cell loss in their study population. They add that this provides corneal surgeons with the reassurance that tissue prepared successfully from donors with diabetes is safe to use for DMEK.
Because recipient diabetes was associated with increased endothelial cell loss, the potential effect on longer-term graft survival merits further study, the investigators say.
Cornea 2017;36:10:1184–1188.
Price, MO, Lisek M, Feng M, Price FW
Reoperation Rate: RRD With Co-existing Macular Hole
Investigators examined surgical outcomes in individuals with coexistent macular hole and rhegmatogenous retinal detachment, as part of a retrospective case series. They looked at all individuals who underwent surgical repair of concomitant MH and retinal detachment in their facility between January 2014 and December 2016.
At least one retinal break was noted in all MHRD cases. Exclusion criteria included MHRD related to high myopia without peripheral retinal tears. Data collected included presence of proliferative vitreoretinopathy and classification at time of surgical repair. Outcomes evaluated included visual acuity comparisons, reoperation rate, final anatomic success and MH closure rate.
Over the study period, MHRD cases accounted for 17 (2.3 percent) of all 745 repaired RDs in the practice. Proliferative vitreoretinopathy was present in 53 percent of MHRD cases. Reoperation rates for MHRD were significantly higher than the practice average for all RD repairs (29 percent vs. 9.7 percent; p=0.01). Final anatomic success with RD was achieved in 100 percent of individuals. Internal limiting membrane peeling was performed in 15 of 17 individuals. The macular hole closure rate was 71 percent after initial surgery. Although 82 percent of individuals experienced equal or improved vision, only 24 percent of individuals achieved VA better than 20/80. Retinal detachment in the contralateral eye was noted in three of 16 individuals (19 percent) before initial presentation or during the follow-up period.
Investigators wrote that visual outcomes in MHRD cases were underwhelming because of high rates of PVR macula-off RRD and reoperation, and relatively low MH closure rates; therefore, they suggested aggressive surgical techniques to repair MHRD.
Ophthalmology Retina 2017; Sep 28. [Epub ahead of print].
Najafi M, Brown JS, Rosenberg KI, et al.
Autoregulation of ONH Blood Flow During Vitreous Surgery
Scientists examined whether hypertension and hyperlipidemia affected autoregulation of optic nerve head blood flow during vitrectomy, as part of a cohort study.
Seventeen eyes from 17 subjects with HTN and HL, and 19 eyes from 19 control subjects without systemic disorders underwent vitrectomy for treatment of epiretinal membranes or macular holes. Following standard 25-gauge microincision vitrectomy, the mean blur rate—an index of relative ONH blood flow—in the vascular area and MBR in the tissue area were measured using laser speckle flowgraphy. Measurements were conducted before, and five and 10 minutes after, an approximately 15-mmHg rise in intraocular pressure. The parameters represented relative values of optic nerve head blood flow (percent, compared to baseline). Scientists calculated the recovery rate of ONH blood flow using the equation: (MBR at 10 min. - MBR at 5 min.)/(MBR at baseline - MBR at 5 min.).
Ocular perfusion pressure in all subjects dropped five and 10 minutes after the increase in IOP. Vascular MBR in subjects with HTN and HL (75.5 ±14.8) was significantly lower than that in controls (86.7 ±12.1) 10 minutes after IOP elevation (p=0.019). The recovery rate of vascular blood flow was significantly lower in the HTN and HL groups than in the control group (p=0.002).
The researchers wrote that their results suggested that HTN and HL impaired autoregulation in the vascular component of ONH blood flow during vitrectomy.
Graefes Arch Clin Exp Ophthalmol 2017; Sep 23. [Epub ahead of print].
Hashimoto R, Sugiyama T, Ubuka M, et al.
Zonal Analysis for Peripapillary Choroidal Thickness in POAG
Researchers evaluated automatic peripapillary choroidal thickness measurements in a wide area around the optic disc and zones in individuals with primary open-angle glaucoma and healthy controls. They used a new swept-source optical coherence tomography device as part of a single-center, observational study.
Researchers enrolled 135 POAG individuals and 86 healthy subjects. They obtained 6-mm × 6-mm, three-dimensional scans of the optic disc using the SS-OCT Triton and generated a 26 × 26 cube-grid centered in the OD to automatically measure choroidal thickness. In addition, they established seven choroidal zones (superior-temporal, -central and -nasal; inferior-temporal, -central and -nasal; and optic nerve head).
PPCT was significantly thinner in the central-superior, nasal-superior and nasal-inferior zones of POAG subjects. Choroidal thickness was:
• in the central-superior zone, 124.61 ±54.95 µm in the POAG group vs. 156.17 ±80.89 µm in healthy controls (p=0.029);
• in the nasal-superior zone, 133.84 ±58.89 µm in the POAG group vs. 168.34 ±73.45 µm in healthy controls (p=0.012); and
• in the nasal-inferior zone, 113.45 ±49.93 µm in POAG vs. 137.47 ±65.96 µm in controls (p=0.049).
Compared with healthy subjects, glaucoma subjects presented with peripapillary choroidal thinning. The researchers say that the new SS-OCT could be a useful tool to evaluate choroidal thinning and aid in glaucoma diagnosis.
Jpn J Ophthalmol 2017; Oct. 11. (Epub ahead of print).
Pablo LE, Bambo MP, Cameo B, et al.



