Just as surgeons’ methods for removing cataracts continue to evolve, so do their options for treating presbyopia and astigmatism with intraocular lenses. In an effort to give surgeons as many options for their patients as possible, lens companies are working on IOLs that incorporate multifocality and toric correction, lenses that provide pseudo-accommodation and even a lens that can potentially change shape within the eye. Here’s a look at several potential future premium IOL options.
AcrySof IQ ReSTOR Multifocal Toric
The ReSTOR Multifocal Toric lens is aimed at giving surgeons a single solution for presbyopic patients who also present with some astigmatism. In addition to its diffractive multifocality and its toric correction, the lens is aspheric, uses a single-piece design and has UV and blue-light filters built in.
Thomas Kohnen, MD, professor and chair of ophthalmology at Goethe University in Frankfurt, Germany, has used the lens both in his practice and in clinical study. “If I have a patient who comes in with astigmatism below 0.75 D, then I use the normal ReSTOR,” he says. “If he has more than that, I use the toric ReSTOR. We’re not sure how high we can go in terms of astigmatism and whether that level of correction will go well with the multifocality. I believe we have used it for astigmatism up to 3 D, which covers 89 percent of patients. You don’t see a lot of patients with 4 D of astigmatism.”
|
The other key outcome surgeons watch for when evaluating a toric lens, multifocal or otherwise, is its stability postop. Along these lines, Dr. Kohnen says he hasn’t been disappointed. “There’s been no notable rotation with the lens,” he avers. “I rarely have to reposition a toric lens. Also, the methods we have to determine preop astigmatism are getting better, and the better you are preoperatively, the greater the chance you won’t have to rotate the lens. The Alcon material is pretty sticky, so, in my opinion, it doesn’t rotate much.”
According to U.S. ReSTOR Multifocal Toric clinical investigator Stephen Lane, MD, of St. Paul, Minn., enrollment in the U.S. trial is complete. “But it will be toward the end of the year for all follow-up visits to be completed,” he says.
Tecnis One-piece Toric
The Tecnis Toric is a one-piece, hydrophobic acrylic lens with a 13-mm overall diameter. It was launched in Europe in 2011. The Tecnis toric has five models designed to treat different amounts of cylinder, from 0.69 D to 2.74 D, measured at the corneal plane.
|
“The haptics have pretty good memory,” Dr. Findl continues. “So in normal-sized capsular bags, it will hold its rotational position quite well. But in very large bags, such as those of highly myopic patients, you may have to wait a little while intraoperatively for the haptics to fully extend and for it to become rotationally stable.”
Though there are some patients in whom the lens doesn’t correct all the astigmatism, Dr. Findl says it often gets close enough for them. “If we put in the toric lens and there’s residual astigmatism, it’s usually not very much,” he says. Dr. Findl says he didn’t have to reposition any of the lenses postop.
In Dr. Findl’s study of the Tecnis One-piece Toric, uncorrected visual acuities postop were between 20/25 and 20/20 in cases without other ocular diseases. However, he says that surgeons may be able to get more consistent results in a greater number of toric Tecnis patients by measuring both anterior and posterior corneal astigmatism. “In 5 to 7 percent of patients, we have the IOL on the correct meridian, we see that the corneal topography hasn’t changed much with surgery—which means the lens was suitable for the eye—yet there is more residual astigmatism than we expected, maybe 1 or 1.25 D,” he says. “When we analyzed these eyes, it turned out that the posterior corneal surface had a different astigmatism from the anterior surface. Now we’re thinking about whether we should be routinely looking at the posterior corneal surface with imaging techniques such as Scheimpflug corneal tomography, as well.”
Though the Tecnis one-piece toric lens isn’t approved in the United States, AMO is planning on bringing it here. “We’re working toward its approval in the United States,” says AMO’s Steve Chesterman.
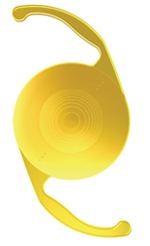
Lenstec Tetraflex
The hydrophilic acrylic Tetraflex’s mechanism of action was initially planned to be along the same lines as the Crystalens’s: Use some forward movement of the lens to attempt to give an improvement in near vision. However, it appears that lens movement doesn’t account for the pseudo-accommodation provided by the lens, so some think another mechanism is at work.
The lens uses closed-loop haptics with a 5-degree angulation that was intended to enhance near vision by working in conjunction with the hydrophilic acrylic material, which is very flexible. “It’s a near-enhancing IOL,” says Los Angeles surgeon Paul Dougherty, who was involved with the 12-center trial of the lens, and who also owns stock in Lenstec.
“We did a substudy within the FDA study and found a 34-percent increase in higher-order aberrations—including coma, spherical aberration and trefoil—with this lens compared to a control lens. We think this increase may be part of the primary mechanism of action.” In the FDA study of the lens, in 242 subjects at one year, the average amount of accommodation was 1.8 D. “So the forward movement of the lens, which we can see isn’t much, can’t account for the almost 2 D of accommodation.”
|
In the study, the investigators primarily used Minnesota Reading Speed as their way of determining the lens’s effect on near vision. “Using MRS, we found that 76 percent of patients were either spectacle-independent or minimally dependent on glasses after surgery,” says Dr. Dougherty. “The reading results aren’t like those of a multifocal lens, where you get J1 and J2 acuities at near routinely. This is typically functional reading, which is J4 and above. Seventy-five percent of patients got distance-corrected near vision of J4 to J6, which translates into reading speed of those optotypes of 80 words per minute. Again, the reading isn’t as good as it is with a multifocal, but you don’t get the side effects such as glare and halo, decreased contrast sensitivity or loss of vision quality.” There was a 1-percent incidence of lenses being inserted so that the haptics folded rather than unfolded, but Dr. Dougherty says this was treated by manipulation of the lens intraocularly.
The trial data for the Tetraflex has been at the FDA for years now, so the next move is the agency’s. In the meantime, 18,000 Tetraflex lenses have been implanted outside the United States and, in 2011, the company rolled out a new version: an aspheric, spherical aberration-neutral lens called the Tetraflex HD. “When and if the Tetraflex gets approved in the United States, the company is likely to not bring it out, and instead apply for approval of the Tetraflex HD,” Dr. Dougherty says. “So, commercially, all U.S. surgeons will see is the HD version.”
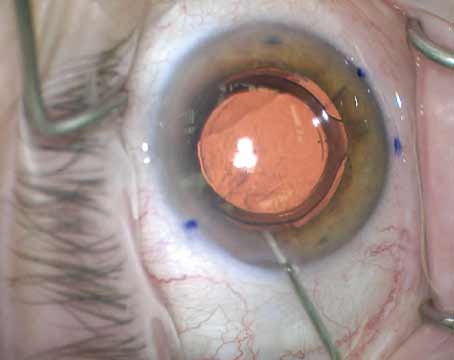
Light-adjustable Lens
The LAL, from Calhoun Vision, is unique among premium lenses because while other lenses make ophthalmologists perform painstaking preoperative biometry to ensure they’re implanting the correct lens, the LAL potentially will allow the surgeon to transform it into the correct lens after it’s already in the eye.
“The LAL is made of photosensitive silicone,” explains Los Angeles surgeon Robert Maloney, the medical monitor of the U.S. LAL trial. “By shining a light on it, the photosensitive silicone reacts, allowing you to increase or decrease the power of the lens. You can also correct astigmatism with the lens by changing the power in one axis.” The lens has a 6-mm optic and polypropylene haptics that aren’t photosensitive, so as to avoid adjusting them with the special light.
Besides the lens itself, Dr. Maloney says the light-delivery system is a key part of the technology. “It’s a very sophisticated system that uses a microchip similar to that used in advanced slide projectors,” he explains. “The chip lets us put a digital pattern on the lens for optimally adjusting the lens power.” The wavelength of the light is around 380 nm.
The process of implanting and adjusting the LAL starts off like a normal lens implantation. “Then, two weeks after the surgery, the doctor, instead of prescribing spectacles, adjusts the lens power,” says Dr. Maloney. The patient’s eyes need to be shielded from sources of UV light for that initial period, and they usually wear some kind of sunglasses or protective lenses. “After two weeks, if the patient is myopic, you do a light adjustment for myopia, the pattern for which looks like an annulus, with very little energy in the middle and a lot near the edge of the lens. The pattern for hyperopia is the opposite. For correcting astigmatism, the light pattern is saddle-shaped, with a lot of energy in one axis and less in the other axis.”
The final step involves locking the pattern in with the same near-UV light. “We do the adjustment and see what the response is,” says Dr. Maloney. “If they’re on target, then we do the lock-in with the light delivery system. If they’re not on target, you can do another adjustment to the lens.”
Calhoun Vision and its investigators are also using the LAL to help enhance patients’ near vision by either creating a central near add or by increasing the lens’s asphericity to increase depth of focus.
Dr. Maloney says the company is moving to a Phase III trial for the astigmatism adjustments, having already completed a Phase II trial for myopia. “In the trial for myopic adjustments, in 74 patients we had more than 85 percent of patients corrected to within 0.5 D of emmetropia,” he says. “We’ve been doing astigmatism correction overseas for a number of years with good results, so the goal of this trial is to prove safety and efficacy.” In the international trial, 95 percent of patients had 0.5 D of cylinder or less postop.
In terms of adverse events, there was one explantation in the Phase II study because the surgeon used an unapproved lens folder and cracked the lens. Also, Dr. Maloney says patients typically experience a pink tint to their vision for a day or two post lock-in.
Looking toward possible U.S. approval, the company needs to complete enrollment of the Phase III study first. “We’ll then follow the patients for a year,” says Dr. Maloney. “We’ll collect the data and then submit it to the FDA. So, it will probably be a two-year process.”
Synchrony
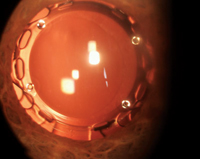
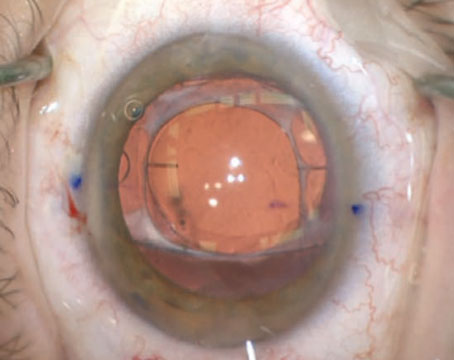
In the vein of unique designs, the Synchrony (Visiogen/AMO) uses two optics in an attempt to give patients a wider range of postop vision.
The Synchrony is composed of silicone and has a +32-D anterior optic that’s 5.5 mm wide, along with a 6-mm posterior optic that varies in power based on the patient’s needs. The two optics are connected by spring haptics and the whole device is 9.5 mm x 9.8 mm in size and designed to fill the capsular bag.
|
Matteo Piovella, MD, of Monza, Italy, who has worked with the Synchrony in his practice, says there are some trade-offs involved with using it.
“The dual-optic IOL is dramatically less sensitive to halos and glare,” he says. “These phenomena are 75 percent less when compared with some multifocal lenses. It gives very good results for distance vision and good intermediate vision, but normally I have to provide my patients with +1-D glasses for small print. So the perfect Synchrony patients for me are the patients who come in and want new IOL technology for some near vision but don’t want any halos or glare; and the patients who are computer users. I think the ability to get computer-distance vision and use a +1 add for certain situations is acceptable for these patients, and they’re really happy. Also, if there is a patient who I suspect will develop maculopathy in the future, I think Synchrony is a good lens. This is because with diffractive multifocal technology, if maculopathy develops in five to 10 years, the patient will be severely penalized. One of the benefits of the Synchrony is it doesn’t penalize contrast sensitivity, which can be decreased by as much as 30 percent in some multifocal lenses.
“It’s important to note that Synchrony patients will experience temporary myopia of -2 to -2.5 D for 45 to 60 days postop,” adds Dr. Piovella. “This is different from the normal IOL that gives a ‘wow’ effect for distance immediately postop. The Synchrony needs time for adaptation to the capsular bag.”
According to Mr. Chesterman from AMO, the company is nearing the launch of the Synchrony in Europe. “It should be approved there by mid-year,” he says. “In the United States, the FDA has requested additional clinical data. We are currently working on generating that data this year.”
Rayner M-flex T
According to Gerd Auffarth, MD, chair of the ophthalmology department at the University of Heidelberg, one of the central design features of the Rayner multifocal toric lens called the M-flex T is its haptics. “The haptic has a patented, so-called anti-vaulting design,” he says. “That means that even if the capsular bag becomes smaller due to fibrosis, the lens haptics will adapt to it and the lens will always center extremely well. Decentration was below 0.1 mm in our clinic and rotational stability was around 1 to 2 degrees.” The lens is composed of hydrophilic acrylic and is available in optic sizes of 5.85 and 6.25 mm. It uses a multi-zone refractive aspheric design that has either four or five annular zones, depending on the lens’s base power, that provide +3 or +4 D of extra power at the IOL plane. “The standard cylinder correction would be 2 D,” says Dr. Auffarth. “Special power ranges are 1 to 1.5 D for low astigmatism, as well as 2.5 D up to 6 D for higher levels of astigmatism, in 0.5-D steps.”
In his practice, Dr. Auffarth has followed nine M-flex T patients for 11 months postoperatively. “The average post-surgical refraction was plano for sphere and -0.5 for cylinder,” he says. “The average spherical equivalent refraction was plano. The uncorrected distance visual acuity was 0.15 in logMAR [slightly worse than 20/25 Snellen], and best-corrected visual acuity was 0.10 logMAR [20/25]. Uncorrected near visual acuity was 0.3 [20/40] and distance-corrected near visual acuity was also 0.3.
“We had to explant a lens because of postoperative glare in one patient,” continues Dr. Auffarth. “Another patient experienced a myopic shift. In the patient with the myopic shift, since the lens had been in the eye too long already, we decided against explantation and so implanted a so-called add-on IOL in the eye. The patient is doing OK now.”
There is a trial of the M-flex T lens, being conducted by Brazilian surgeon Patrick Tzelikis, MD, PhD, currently registered with the FDA.
In the Wings
There are several other lenses that, though not being studied in FDA trials, are expected by many experts to make their way to ophthalmologists in the United States in some form in the future.
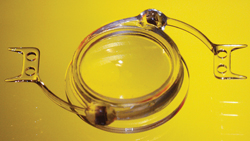
The DynaCurve (NuLens Ltd., Herzliya Pituah, Israel) is an out-of-the-bag IOL, based instead in the sulcus.
The lens’s design involves a PMMA anterior lens that the company calls a “reference plane” that provides distance correction, a small chamber that contains a solid silicone gel, and a posteriorly situated piston with an aperture in the center. The haptics are secured by internal scleral fixation to the sulcus without sutures. The chamber containing the flexible gel is in a fixed position. The piston, moved by ciliary muscle force, presses the gel through a small aperture to form a bulge that functions as a lens.
|
The Carl Zeiss AcriLisa diffractive multifocal toric IOL takes a different approach to focusing incoming light. “The AcriLisa is distance-dominant, so the distant focus gets 65 percent of the incoming light, and near focus gets only 35 percent,” says Vienna’s Dr. Findl. “So, it’s a distance-dominant lens that has pretty good intermediate vision and maybe slightly worse contrast sensitivity at near. However, I don’t find this to be a problem with most patients, because many of them need mostly intermediate vision and not necessarily as much near vision.” Another IOL aimed at giving patients a wider range of vision while also correcting astigmatism is Bausch + Lomb’s Crystalens toric, currently in development.
Information about Hoya’s Adoptics shape-changing lens is also currently under wraps. According to Hoya, the Adoptics lens uses a fluid-based refraction system within the IOL to create significant changes in refractive power, without requiring lens movement. The company says the refractive surface of the lens changes shape in response to movement of the ciliary muscles.
Surveying the landscape of presbyopic and toric premium lenses, Dr. Piovella says that, no matter what kind of intraocular lens technology a surgeon decides to adopt, it will end up dramatically changing his practice. “If you switch to multifocal or accommodative lens technology, you have to improve your patient selection, improve the technology you use to detect the right or the wrong patient preoperatively, and follow patients more strictly than usual. You have to learn, really learn, how the lens works,” he says. “You have to put in the maximum effort in getting the best biometry to get the perfect identification of the right IOL power. If you follow these rules, your practice will be effective and your experience with these lenses will be very positive. If not, there will be drama.” REVIEW