Using a novel high-throughput screening process, scientists have for the first time identified molecules with the potential to block the accumulation of a toxic eye protein that can lead to early onset of glaucoma.
The researchers have implicated a mutant form of the protein myocilin as a possible root cause of increased eye pressure. Mutant myocilin is toxic to the cells in the part of the eye that regulates pressure. These genetically inherited mutants of myocilin clump together in the front of the eye, preventing fluid flow out of the eye, which then raises eye pressure. This cascade of events can lead to early-onset glaucoma, which affects several million people from childhood to age 35.
To find molecules that bind to mutant myocilin and block its aggregation, the researchers designed a simple, high-throughput assay and then screened a library of compounds. They identified two molecules with potential for future drug development to treat early-onset glaucoma.
“These are really the first potential drug targets for glaucoma,” said Raquel Lieberman, PhD, an associate professor in the School of Chemistry and Biochemistry at the Georgia Institute of Technology in Atlanta, whose lab led the research.
Dr. Lieberman presented her findings on January 20 at the
Society for Laboratory Automation and Screening conference in San Diego, Calif.
The study was published on Nov. 26, 2013, in the journal ACS Chemical Biology.
At the heart of the study was an assay that Dr. Lieberman’s lab created to take advantage of the fundamental principles of ligand binding. In their assay, mutant myocilin is mixed with a fluorescent compound that emits more light when the protein is unwound. When a molecule from the library screen binds to myocilin, the pair becomes highly stable—tightly wound—and the fluorescent light emitted decreases. By measuring fluorescence, researchers were able to identify molecules that bound tightly to mutant myocilin.
  |
|
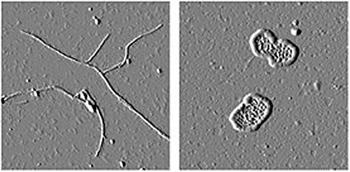
The glaucoma-associated olfactomedin domain of myocilin in straight fibrils common to many amyloids (left) and a disease-causing variant forming large circular fibrils (right). |
|
The researchers then added these molecules to cultured human cells that were making the toxic aggregating myocilin. Treating the cells with the newly identified molecules blocked the aggregation and caused the mutated version of myocilin to be released from the cells, reducing toxicity.
“We found two molecules from that initial screen that bound to our protein and also inhibited the aggregation,” Dr. Lieberman said. “When we saw that these compounds inhibited aggregation then we knew we were onto something good because aggregation underlies the pathogenesis of this form of glaucoma.”
In a separate study, the same lab characterized the toxic myocilin aggregates. The study found that my-ocilin aggregates are similar to the protein deposits called amyloid, which are responsible for Alzheimer’s disease and other neurodegenerative diseases.
“In Alzheimer’s disease, the deposits are extracellular and kill neurons. In glaucoma the aggregates are not directly killing neurons in the retina to cause vision loss, but they are cytotoxic in the pressure-regulating region of the eye,” Dr. Lieberman said. “It’s parallel to all these other amyloids that are out there in neurodegenerative disease.”
The researchers are now focusing on mapping the structure of myocilin to learn more about what myocilin does and why it is in the eye in the first place.
“The underlying problem with myocilin is that for 14 years it has been studied and still nobody really knows what its biological role is inside the eye,” Dr. Lieberman said.
Chemical Restores Light Perception To Blind Mice
Progressive degeneration of photoreceptors—the rods and cones of the eyes—causes blinding diseases such as retinitis pigmentosa and age-related macular degeneration. While there are currently no available treatments to reverse this degeneration, a newly developed compound allows other cells in the eye to act like photoreceptors. As described in a study appearing in the
February 19 issue of the journal Neuron, the compound may be a potential drug candidate for treating patients suffering from degenerative retinal disorders.
The retina has three layers of nerve cells, but only the outer layer contains the rod and cone cells that respond to light. When the rods and cones die during the course of degenerative blinding diseases, the rest of the retina remains intact but unable to respond to light. Even though the innermost layer’s nerve cells, called ganglion cells, remain connected to the brain, they no longer transmit information useful for vision.
Professor Richard Kramer, of the University of California, Berkeley, and his colleagues have invented “photoswitch” chemicals that confer light sensitivity on these normally light-insensitive ganglion cells, restoring light perception in blind mice. An earlier photoswitch required very bright ultraviolet light, making it unsuitable for medical use. However, a new chemical, named DENAQ, responds to ordinary daylight. Just one injection of DENAQ into the eye confers light sensitivity for several days.
Experiments on mice with functional, nonfunctional or degenerated rods and cones showed that DENAQ only impacts ganglion cells if the rods and cones have already died. It appears that degeneration in the outer retina leads to changes in the electrophysiology in the inner retina that enables DENAQ photosensitization, while the presence of intact photoreceptors prevents DENAQ action.
The selective action of DENAQ on diseased tissue may reduce side effects on healthy retina, exactly what is desired from a vision-restoring drug. “Further testing on larger mammals is needed to assess the short- and long-term safety of DENAQ and related chemicals,” says Dr. Kramer. “It will take several more years, but if safety can be established, these compounds might ultimately be useful for restoring light sensitivity to blind humans. How close they can come to re-establishing normal vision remains to be seen.”
REVIEW
Exercise May Slow Retinal Degeneration
|
|
Moderate aerobic exercise helps to preserve the structure and function of nerve cells in the retina after damage, researchers at the Emory Eye Center and the Atlanta VA Medical Center have found.
The findings, from a study of an animal model of age-related macular degeneration, are the first to suggest that aerobic exercise can have a direct effect on retinal health and vision. The results were scheduled for
publication Feb. 12 in the Journal of Neuroscience.
“This research may lead to tailored exercise regimens or combination therapies in treatments of retinal degenerative diseases,” said Machelle Pardue, PhD, one of the senior authors. “Possibly in the near future, ophthalmologists could be prescribing exercise as a low-cost intervention to delay vision loss.”
Although several studies in animals and humans point to the protective effects of exercise in neurodegenerative diseases or injury, less was known about how exercise affects vision.
The researchers ran mice on a treadmill for two weeks before and after exposing the animals to bright light that causes retinal degeneration. They found that treadmill training preserved photoreceptors and retinal cell function in the mice.
They trained mice to run on a treadmill for one hour per day, five days per week, for two weeks. After the animals were exposed to toxic bright light—a commonly used model of retinal degeneration—they exercised for two more weeks. The exercised animals had nearly twice the number of photoreceptor cells of animals that spent the equivalent amount of time on a stationary treadmill, and their retinal cells were more responsive to light.
“One point to emphasize is that the exercise the animals engaged in is really comparable to a brisk walk,” Dr. Pardue said. “One previous study that examined the effects of exercise on vision in humans had examined a select group of long distance runners. Our results suggest it’s possible to attain these effects with more moderate exercise.”
The researchers were able to show that the effects of exercise come partly from a growth factor called BDNF, which was thought to be involved in the beneficial effects of exercise in other studies. Exercised mice had higher levels of BDNF in the blood, brain and retina, while chemically blocking BDNF receptors effectively eliminated the protective effects of aerobic exercise, they demonstrated.
The group is testing whether other exercise regimens are even more protective and whether exercise is beneficial in models of other retinal diseases such as glaucoma and diabetic retinopathy.
|
|
|
MIT Researchers Devise Hand-Held OCT
|
|
Researchers at the Massachusetts Institute of Technology have devised a new ophthalmic-screening instrument that could enable widespread use of a hand-held optical coherence tomographer to screen for retinal disease. The paper describing their device was
published in the open-access journal Biomedical Optics Express.
The developers say the new design is the first to combine cutting-edge technologies such as ultrahigh-speed 3-D imaging, a tiny micro-electro-mechanical systems mirror for scanning and a technique to correct for unintentional movement by the patient. These innovations, they say, should allow clinicians to collect comprehensive data with just one measurement.
“Hand-held instruments can enable screening a wider population outside the traditional points of care,” such as a primary-care physician’s office, a pediatrician’s office or even in the developing world, said author and researcher James Fujimoto, PhD, of MIT.
Tabletop OCT imagers have become a standard of care in ophthalmology. The researchers were able to shrink what has been typically a large instrument into a portable size by using a MEMS mirror to scan the OCT imaging beam. They tested two designs, one of which is similar to a handheld video camera with a flat-screen display. In their tests, the researchers found that their device can acquire images comparable in quality to conventional table-top OCT instruments.
To deal with the motion instability of a hand-held device, the instrument takes multiple 3-D images at high speeds, scanning a particular volume of the eye many times but with different scanning directions. By using multiple 3-D images of the same part of the retina, it is possible to correct for distortions due to motion of the operator’s hand or the subject’s own eye. The next step, Dr. Fujimoto said, is to evaluate the technology in a clinical setting. But the device is still relatively expensive, he added, and before this technology finds its way into doctors’ offices or in the field, manufacturers will have to find a way to support or lower its cost.
In the future, Dr. Fujimoto envisions that hand-held OCT technology can be used in many other medical specialties beyond ophthalmology, for example, in applications ranging from surgical guidance to military medicine.
“The hand-held platform allows the diagnosis or screening to be performed in a much wider range of settings,” he said. “Developing screening methods that are accessible to the larger population could significantly reduce unnecessary vision loss.” |
|
|



