Differential diagnosis of the mass included a neoplastic process such as amelanotic choroidal melanoma or metastases with overlying thinning of the sclera. Additional considerations included an inflammatory process, such as posterior scleritis or granulomatous disease, or a structural process, such as choroidal effusion or exudative retinal detachment.
Further workup was directed at imaging the mass and macula. Optical coherence tomography of the macula of the right eye showed internal limiting membrane irregularity with retinal folds (Figure 4), consistent with retinal striae seen on examination. B-scan ultrasonography documented echodense thickening of the eye wall with high internal reflectivity and a thickness of 4.9 mm, consistent with scleritis (Figure 5). Transillumination of the mass revealed complete transmission of light, more suggestive of scleritis rather than solid melanoma. Review of previous MRI images revealed no extension of the mass into the optic nerve or orbit.
Given the patient’s examination, a diagnosis of anterior and posterior scleritis was made. The diagnosis was based on several factors: First, she had symptoms of pain and anterior segment signs consistent with anterior scleritis. In addition, there was an elevated mass with normal-appearing overlying choroidal and retinal vessels and orange color, lacking pigmentation, that was similar to the surrounding fundus. Furthermore, B-scan ultrasonography showed dense thickening of the eye wall and transillumination revealed complete passage of light, consistent with posterior scleritis. At this time, the patient was started on oral prednisone 80 mg daily with a slow taper. She was also referred to the rheumatology department for further workup of a possible systemic autoimmune etiology, but all of her lab results were unrevealing.
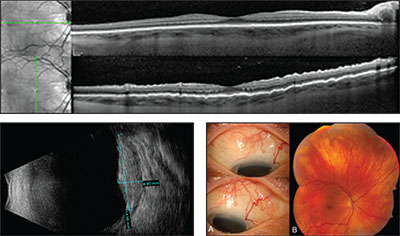 |
| Figure 4 (top). Optical coherence tomography of the right eye showing internal limiting membrane irregularity with retinal folds on vertical orientation. Figure 5 (bottom left). B-scan ultrasonography of the right eye showing echodense diffuse posterior thickening with high internal reflectivity, consistent with posterior scleritis. Figure 6 (bottom right). Three months following initiation of oral prednisone, the episclera (A) showed improvement and the fundus (B) demonstrated reduction in scleral thickening, with nearly complete resolution of symptoms. |
At one-month and three-month follow-up, she had improvement in her pain and the fundus abnormalities (Figure 6). However, there was mild recurrence of her symptoms during the prednisone taper, so she was started on mycophenolate mofetil 1,500 mg twice daily by the rheumatologist.
Discussion
Posterior scleritis is a rare disease and confirming the diagnosis can be challenging. It can mimic many other disease processes;1 among these is choroidal melanoma or metastasis, as seen in our patient. Although all age groups can be affected, one study of 99 patients with posterior scleritis found the mean age at onset to be 49.2 This condition also has a predilection for women and is twice as common in females compared to males. Posterior scleritis is associated with systemic disease in 30 percent of cases, including rheumatoid arthritis, systemic vasculitis and granulomatosis with polyangitis.2
The most common presenting symptoms are unrelenting periocular pain, headache, decreased vision and epibulbar redness.2,5 There is clinical evidence of anterior scleritis in one-third of cases at the time posterior scleritis is diagnosed, and anterior involvement is present in 60 percent of cases at some point on follow-up.2 On examination, patients most commonly manifest deep scleral thickening with overlying serous retinal detachment, and occasionally optic disc edema. Other findings can include retinal striae, choroidal folds and choroidal detachment.5 Vision loss occurs in approximately 33 percent of cases, most commonly secondary to exudative retinal detachment, macular distortion from a scleral mass, and cystoid macular edema.2,5,6 Although rare, 1 to 3 percent of patients can develop permanent vision loss.2 Rarely, patients may have deep ocular pain without objective findings. In fact, in a study of 99 patients with posterior scleritis, 17 percent had no clinical abnormalities,2 and therefore required an even higher index of suspicion to make the diagnosis.
B-scan ultrasonography is helpful in diagnosing posterior scleritis. Characteristic findings include diffuse, echodense thickening of the posterior sclera as well as the classic “T sign.”5,7 This is due to squaring off of a normally rounded optic nerve along with edema in Tenon’s capsule extending along the posterior aspect of the eye forming a “T” shape. On MRI, the sclera in posterior scleritis has a low signal with a small degree of retinal/choroidal enhancement, the surrounding orbital tissues may show greater enhancement.8
Of particular interest in this case, posterior scleritis can masquerade as other disease processes, including choroidal melanoma.9-12 Of the 12,000 cases of posterior uveal melanoma referred to a tertiary care center, 1,739 (14 percent) were pseudomelanomas and 5 cases (<1 percent) were due to posterior scleritis.13 B-scan ultrasonography greatly aids in distinguishing posterior scleritis from melanoma, as it will show an echo-dense mass with scleritis, whereas melanoma is echo-lucent. Posterior scleritis also reveals complete transmission of light on transillumination, whereas melanoma would likely block transmission. Additionally, presence of pain is more common in cases of scleritis, although it can be present in cases of tumor necrosis. If the findings are equivocal, fine-needle aspiration biopsy can be performed for a definitive diagnosis.8
Patients with posterior scleritis may respond well to nonsteroidal anti-inflammatory drugs.2 However, systemic prednisone is often necessary for resolution of symptoms and findings. In more severe cases with vision loss from optic nerve or macular involvement, intravenous corticosteroids can be initiated, followed by oral prednisone taper for complete resolution.2 Long-term dependency on corticosteroids may require adjustment to a steroid-sparing agent, such as mycophenolate mofetil, cyclophosphamide or cyclosporine A.2
Posterior scleritis is a rare inflammatory disease associated with pain, headache, redness and vision loss that can masquerade as other entities. In presenting this case we hope to highlight this rare entity along with the accompanying testing that can be instrumental in establishing the correct diagnosis.
1. Benson WE, Shields JA, Tasman W, Crandall AS. Posterior scleritis: A cause of diagnostic confusion. Arch Ophthalmol 1979;97:8:1482-6.
2. McCluskey PJ, Watson PG, Lightman S, et al. Posterior scleritis: Clinical features, systemic associations, and outcomes in a large series of patients. Ophthalmology 1999;106:12:2380-6.
3. Watson PG, Hayreh SS. Scleritis and episcleritis. Br J Ophthalmol 1976;60:3:163-191.
4. Lyne AJ, Pitkeathley DA. Episcleritis and scleritis. Arch Ophthalmol 1968;80:2:171-176.
5. Benson WE. Posterior scleritis. Surv Ophthalmol 1988;32:5:297-316.
6. Cleary PE, Watson PG, McGill JI, et al. Visual loss due to posterior segment disease in scleritis. Trans Ophthalmol Soc UK 1975;95:2:297-300.
7. Coleman DJ, Jack RL, Jones IS, Franzen LA. Ultrasonography VI. Pseudotumors of the orbit. Arch Ophthalmol 1972;88:5:472-80.
8. Li CQ, Cho AA, Edward NJ, et al. Magnetic resonance imaging of uveitis. Neuroradiology 2015;57:8:825-32.
9. Arevalo JF, Shields CL, Shields JA. Giant nodular posterior scleritis simulating choroidal melanoma and birdshot retinochoroidopathy. Ophthalmic Surg Lasers Imaging 2003;34:5:403-5.
10. Demirci H, Shields CL, Honavar SG, Shields JA, Bardenstein DS. Long-term follow-up of giant nodular posterior scleritis simulating choroidal melanoma. Arch Ophthalmol 2000;118:9:1290-2.
11. Liu AT, Luk FO, Chan CK. A case of giant nodular posterior scleritis mimicking choroidal malignancy. Indian J Ophthalmol 2015;63:12:919-21.
12. Sin PY, Liu DT, Young AL. Nodular posterior scleritis mimicking choroidal tumor in a patient with systemic lupus erythematous: A case report and literature review. Asia Pac J Ophthalmol (Phila) 2015. Epub ahead of print.
13. Shields JA, Mashayekhi A, Ra S, Shields CL. Pseudomelanomas of the posterior uveal tract: The 2006 Taylor R. Smith Lecture. Retina 2005;25:6:767-71.



