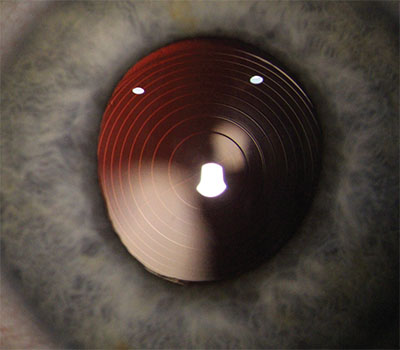
AMO’s Symfony Toric
The recently approved Symfony toric sets itself apart from similar lenses by being the only extended depth of focus lens approved in the United States. This hydrophobic, acrylic EDOF lens is able to achieve this extended-depth-of-focus through some unique design elements. The Symfony has a defractive grating on its face, similar to multifocal lenses, but has some significant differences. The ring structures have z-shaped echelette formations that elongate the focus area, rather than splitting and dispersing the light.
Jim Loden, MD, an ophthalmologist based in Nashville, provides some
 |
| The Symfony has four toric models to correct up to approximately 3 D of stigmatism at the corneal plane. |
The Symfony has four toric models to correct up to approximately 3 D of astigmatism at the corneal plane. Models ZXT150, ZXT225, ZXT300 and ZXT375 correct 1.03 D, 1.54 D, 2.06 D and 2.57 D of astigmatism at the corneal plane, respectively. “For treating more than that, we have the option of doing bioptics,” says Dr. Loden. “I leave the patient with compound myopic astigmatism; I intentionally leave him with nearsightedness in the IOL calculation. Then I can just do LASIK surgery to correct the rest of the astigmatism. Say someone has six diopters of astigmatism preop. You’re going to get three diopters of it with the Symfony toric and correct 2.75 to three through the refractive surgery, depending on the calculation.”
In terms of postop rotation, Dr. Loden claims that it’s minimal. Because the Symfony lens is similar to the TECNIS Toric IOL, the FDA drew from the TECNIS Toric approval data, which reported that of the first eyes done with the toric lens, 97 percent had <10 degrees of rotation from baseline to six months. “I have presented that data, and I’m basically seeing zero rotation,” he says. “I have not come back and repositioned a Symfony toric yet. For those saying the lens is more prone to rotate, I’m not seeing that at all.” The same study reported more than 90 percent of eyes having ≤5 degrees of axis change between consecutive visits three months apart.
Sioux City, Iowa, surgeon Jason Jones, MD, offers these tips for reducing the risk of rotational issues. “The first is to have a very clean surgical experience without any zonular compromise and have the capsulorhexis overlap the optic for 360 degrees,” he says. “Then, ensure you have complete viscoelastic removal from the posterior surface of the IOL. In my experience, I find that if I evacuate the viscoelastic from beneath the optic, it will disappear [from my view]. However, if I then rotate the lens 180 degrees and go behind the optic again, I’ll sometimes find a very small amount of viscoelastic remaining.
“In addition, though you of course leave the eye nicely closed and secure in terms of the wound, you might want the IOP to be a little lower than with a non-toric lens,” Dr. Jones adds. “This is so you don’t hyperinflate the capsular bag and the anterior segment, and instead have it ‘collapse’ around the haptic peripherally, if you will.
“If you want to avoid a rotational issue, I’d look into a capsular tension ring,” he continues. “The first option along these lines would be a regular CTR that most surgeons are familiar with. This will help ensure the capsular bag is symmetrically expanded and that there’s no ovalization of the peripheral capsule. Ovalization can permit the lens to rotate, and this helps prevent that. The other strategy, though I don’t use it routinely, is to use a Henderson CTR. This device has undulations in the ring structure and it, theoretically, provides an interface for the haptics to interact with, peripherally, thus preventing a rotational problem. The last strategy—which most surgeons probably won’t want to employ—is to do some form of optic capture,” he continues. “In some circumstances you can consider a reverse optic capture in which the haptics are in the bag and the optic is prolapsed through the anterior capsulorhexis. I tend to avoid this in the Tecnis single-piece family because the optic has fairly thick peripheral structure and has a squared-off anterior and posterior edge, and I want to avoid any potential iris chafe. Other single-piece acrylic lenses from other manufacturers might be more agreeable to this strategy, however. For the Tecnis monofocal toric lenses, I’ve also employed optic capture through a posterior capsulorhexis, both secondarily in patients who experience rotation and in primary cases in which I want to avoid rotation. Though this ensures no postop rotation, it’s not for the faint of heart, since you must be willing and able to perform a posterior capsulorhexis.”
To aid in the implantation of the new toric Symfony, Abbott offers an online calculator. Visit it at https://www.amoeasy.com.
Alcon’s ReSTOR +3 Multifocal Toric
The ReSTOR +3 D Multifocal Toric has the distinction of being the first toric multifocal approved in the United States, winning approval in late December 2016.
The lens is a foldable, hydrophobic acrylic. The diffractive, multifocal optic is on the anterior surface of the lens, with the toric component incorporated on the posterior surface. Since the lens is biconvex and foldable, it can be implanted through a relatively small incision. It’s available in four models for correction of astigmatism from 0.75 to 2.82 D at the corneal plane.
Suresh Pandey, MD, of Kota, India, describes the design of the toric ReSTOR. “The new lens is built on Alcon’s AcrySof platform and is designed to provide cataract patients that have astigmatism with a surgical option that delivers quality vision at all distances,” he says.
R
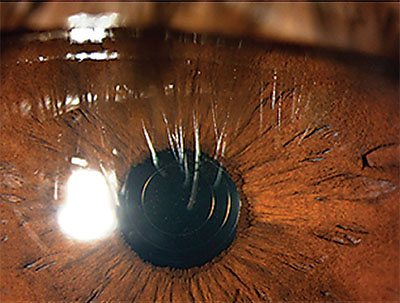 |
| This postop image shows a clear cornea and the ReSTOR multifocal toric IOL successfully implanted in a 45-year-old patient who underwent refractive lens exchange. |
Dr. Pandey also provides some insight into managing intraoperative complications. “If the posterior capsule is torn, the surgeon should try to convert the tear to a circular posterior capsulorhexis,” he says. “Toric and multifocal toric IOL implantation shouldn’t be attempted in the capsular bag in the presence of a posterior capsulorhexis. If a posterior capsulrrhexis can’t be achieved, then sulcus implantation of a three-piece, monofocal IOL with optic capture in the bag behind the anterior capsulorhexis can be attempted. Don’t forget to adjust the IOL power in this event.”
In terms of postop complications, Dr. Pandey says rotation is not too much of an issue, though he does recommend follow-up appointments at least three months apart to monitor rotational stability. Because of its multifocal design, the lens is more prone to halos and glare, however. The data from the clinical study1 demonstrates that the highest rate of “severe” reports of visual distortions at one year was for halos, at 7.5 percent. In terms of glistenings, 95.7 percent and 96 percent of subjects had no observation of glistenings in the first and second eye, respectively. None of the observed glistenings were reported as clinically significant by the implanting surgeons.1 “The problems of glare and halos during night-time are typically minimal with the modern toric multifocal IOL design,” Dr. Pandey says. “Refractive surprise after implanting a toric multifocal can also be managed with LASIK or piggyback IOL implantation.” The data from the FDA trial demonstrates that 94.2 percent (first eye) and 93.9 percent (second eye) of the subjects had rotation of five degrees or less between two consecutive visits.
In the trial, 97.2 percent of first and second eyes had less than 10 degrees of rotation from surgery to 12 months. The mean absolute difference between the achieved lens axis orientation at surgery and at 12 months was 2.7 ±5.8 degrees in the first operative eyes and 2.2 ±2.7 degrees in the second operative eyes. Furthermore, the mean actual difference between the achieved lens axis orientation and the achieved axis placement at surgery (either positive or negative) was ≤1.0 ±6.3 degrees in the first and second operative eyes at all postoperative visits.
Alcon also offers a toric lens calculator. View it at http://www.acrysoftoriccalculator.com.
Bausch + Lomb’s enVista
Not approved in the United States—but in clinical trials—Bausch + Lomb’s enVista toric IOL is in the pipeline, with the company hoping it’ll be approved within the year. The enVista toric IOL is made of a hydrophobic acrylic material, and is designed to be kept in isotonic saline in its packaging so that it emerges with the same tonicity as the aqueous. The company says that this prevents the mechanism that results in glistenings.
Mark Packer, MD, a surgeon from Boulder, Colo., describes the toric models that the enVista offers. “There are three steps similar in magnitude to the the AcrySof toric,” he says. “It’s 0.9 D, 1.4 D and 1.93 D in terms of the astigmatism it corrects at the corneal plane.”
 |
| Bausch + Lomb’s enVista toric IOL. |
When discussing the postop results in terms of visual acuity and corrected astigmatism, Dr. Packer says, “It does quite well,” referencing a 2015 study2 that measured the postop results of the enVista. According to the study, 90.5 percent of eyes implanted with the enVista toric IOL showed less than five degrees of rotation. More than 10 degrees of rotation was observed in 9.5 percent of patients with the enVista toric.2 In terms of uncorrected distance visual acuity, 80 percent of the enVista cases saw 20/25 or better postop, and just under 40 percent saw 20/20 or better. Same thing for correction of astigmatism. It decreased the average astigmatism from 1.89 D preop to 0.41 D postop.2
Dr. Packer also offers a pearl to ensure good surgical outcomes. “One of the things with the enVista material is that it unfolds a little more slowly than the other torics,” he says. “You have to wait 30 seconds when you implant the lens to let it unfold. We learned pretty early on that if you’re in a hurry and you get up from the operating table before the lens is in the capsule, it will rotate when the patient sits up. It hasn’t contacted the capsule—it’s still a taco shape. So, given that you will wait the 30 seconds because you believe in good outcomes, then the mean rotation is in the realm of two degrees. Dr. Packer also highlights the importance of follow-up appointments. “Rotation generally occurs between the end of surgery and the next visit,” he says. “That’s the most important time point, which is why you must let the lens unfold all the way.”
Upon the enVista’s approval in Europe, Bausch + Lomb reported that the trials showed that 91 percent of patients had ≤5 degrees of rotation from postop to six months. The mean rotation at six months was 3 degrees. Bausch + Lomb also noted that no glistenings were detected with the enVista lens at any time during a two-year prospective study of 172 eyes.
Regarding the timeline for the enVista’s approval in the United States, Dr. Packer believes that the approval is imminent. “The FDA study is complete, and the submission is in process,” he says. “Bausch + Lomb would probably be expecting approval sometime this year. The company’s monofocal enVista has been approved for several years, which is the same lens without the toric element, so I would assume the approval will be happening soon.” REVIEW
Dr. Loden is a consultant for AMO and was paid as a part of the Symfony FDA trials. Dr. Jones has consulted for Abbott and was an investigator in the Symfony FDA trial. Dr. Pandey reports no financial interest in any products or procedures discussed in this article. Dr. Packer is a consultant for Bausch + Lomb.
1. http://ecatalog.alcon.com/iol_dfu/40-500-135_us_en.pdf accessed 9 Feb 2017.
2. Garzón N, Poyales F, Ruiz-García J, et al. Evaluation of rotation and visual outcomes after implantation of monofocal and multifocal toric intraocular lenses. J Refract Surg. 2015;3:1-9.



