Although toric intraocular lenses are considered a “premium” option—one that can have a profound impact on a patient’s vision—they involve far fewer potential visual tradeoffs than premium options such as multifocal IOLs. Nevertheless, they do require making some extra effort and managing the occasional pitfall. With that in mind, several surgeons with extensive experience implanting toric IOLs answer 11 key questions to help make sure you end up with happy toric IOL patients.
1. What should I use to determine toric power and orientation?
Y. Ralph Chu, MD, founder and medical director of Chu Vision Institute in Bloomington, Minnesota, and adjunct associate professor of ophthalmology at the University of Minnesota, says the most critical measurement when implanting a toric lens is topography. “That not only defines the magnitude of corneal astigmatism on the anterior corneal surface, it also helps define the type of astigmatism—regular or irregular,” he says. “When thinking about implanting a toric IOL, surgeons need to shift from looking at the astigmatism in the patient’s refraction to seeing what topography reveals.”
Dr. Chu notes that just doing keratometry isn’t sufficient. “Keratometry is the classic way of measuring astigmatism, and today most of us calculate lens power using advanced instruments like the IOLMaster or Lenstar that do take keratometry into account,” he says. “However, relying on something like keratometry alone is just not sufficient. Corneal topography is essential, especially in patients who’ve had previous corneal refractive surgery.”
George Waring IV, MD, FACS, founder and medical director of the Waring Vision Institute in Mount Pleasant, South Carolina, believes it’s essential to base your toric lens choice on at least two measurements. “To measure magnitude and orientation,” he says, “you should use optical biometry and either tomography or placido-based topography.”
David F. Chang, MD, a clinical professor at the University of California San Francisco and in private practice in Los Altos, California, says that in his experience, the single most important factor when calculating the toric correction is to use the Barrett toric calculator. “The Barrett toric calculator uses the keratometry readings obtained from the exam and then makes a theoretical adjustment for posterior corneal astigmatism,” he explains. “The Barrett toric calculator is available online through the websites of the American Society of Cataract and Refractive Surgery and the Asia Pacific Association of Cataract and Refractive Surgeons. It’s also integrated into the IOLMaster 700 and the Lenstar LS 900 biometers.”
Dr. Chu adds that taking more than two measurements preoperatively isn’t usually necessary; he only does so based on the individual patient. “In our practice, we have the ability to take multiple measurements on different devices to gather more data about a patient’s astigmatism,” he says. “This can be helpful for determining whether some patients are good candidates for a toric IOL, especially patients that have had previous laser vision correction. But at the very least, a good corneal topography is essential in the preoperative assessment of patients seeking a toric IOL.”
2. Does the astigmatism measured in the manifest refraction matter?
“Conventional wisdom says to disregard refractive astigmatism,” notes Dr. Waring. “However, we have a different philosophy in our practice, because we’re operating on younger and younger patients, treating cataracts and dysfunctional lens syndrome.
“One reason surgeons have disregarded the manifest refraction is that the lens, which may contribute to the total astigmatism, comes out,” he explains. “However, we’ve found that the manifest refraction is useful for predicting the astigmatic contribution of the posterior cornea. It can provide clues about how aggressive we need to be in terms of addressing against-the-rule or oblique astigmatism. For example, if someone has against-the-rule astigmatism, it’s not uncommon to pick up on the posterior cornea
contribution in the refractive astigmatism. This may tell us that we need to treat the total corneal astigmatism more aggressively.”
 |
3. What makes someone a poor candidate for a toric IOL?
“I’d avoid implanting a toric lens in an eye with markedly irregular astigmatism, where the manifest refraction fails to neutralize the astigmatism,” says Dr. Waring. “Irregular astigmatism can be grouped into two types: skewed radial axis and asymmetric bowtie. In eyes with either of these, a toric lens should be used with caution.
“If the astigmatism is an asymmetric bowtie, it’s true that a toric IOL might help to debulk it,” he continues. “However, in an extreme example such as keratoconus, a careful discussion should be had with the patient, because he or she might need to wear a specialty rigid or hybrid contact lens afterwards. By implanting a toric lens in that situation you’ve made the astigmatism much more optically complex.”
Dr. Chu agrees. “I’d be cautious about putting a toric lens in an eye with irregular astigmatism,” he says. “That includes eyes with keratoconus or pellucid marginal degeneration. If residual astigmatism still needs to be corrected and the patient needs a contact lens, the lens required might be a complex lens such as a bi-toric contact lens. Those can be more difficult to fit, and they’re more expensive. You have to think about what will happen after surgery if that patient wants further reduction of the astigmatism.”
4. How much does astigmatism of the cornea’s posterior surface matter, and how should I account for it?
“Toric IOLs have been around long enough that most of us know there’s a component of posterior corneal astigmatism we have to take into consideration,” says Dr. Chu. “Many practices are transitioning to instruments that can look at both the anterior and posterior surfaces of the cornea and calculate total corneal power. That’s important when we’re trying to fine-tune the results, but at the very least, in the initial assessment you have to look at an anterior surface topography to determine candidacy for a toric IOL and its placement.”
Dr. Waring believes that taking the refractive contribution of the posterior cornea into account is essential. “It’s important to understand how posterior astigmatism works,” he notes. “It tends to behave in predictable ways, so in most cases you can account for it without having an exact measurement.
“The vast majority of people naturally have with-the-rule posterior corneal astigmatism,” he explains. “Refractively, that creates against-the-rule astigmatism because the posterior cornea acts like a minus lens. As a result, we have to be more aggressive when we treat topographic anterior-surface against-the-rule astigmatism, and less aggressive when we treat with-the-rule astigmatism.
“It should be noted, however, that patients that have with-the-rule astigmatism tend to be more predictable in terms of determining the posterior cornea’s contribution,” he continues. “That contribution is less predictable when the astigmatism is oblique, and even more unpredictable when it’s against-the-rule. Fortunately, current advances in technology and diagnostics are allowing us to directly measure the contribution of the posterior cornea, in terms of magnitude and orientation.”
Dr. Chang reiterates that the Barrett toric calculator uses the keratometry readings obtained from the exam and makes a theoretical adjustment for posterior corneal astigmatism. “The posterior corneal astigmatism not only affects the amount of optimal toric power, but also the axis for oblique astigmatism,” he points out. “In addition, the IOL Master 700 now has ‘TK’ software that measures the total keratometry by combining the anterior and posterior corneal curvatures. The latter is inferred by combining the corneal thickness, as determined by OCT, with the telecentric keratometry readings.”
Dr. Chang adds that a study by Tiago Ferreira, MD, and colleagues showed that directly measuring the posterior corneal curvature didn’t produce better outcomes than using the theoretical adjustments of the Barrett toric calculator.1 “In any case,” Dr. Chang says, “I would definitely not ignore posterior corneal astigmatism. Using the Barrett toric calculator is very important and, in my experience, very reliable.”
Dr. Chu says that, as a clinician, he believes overlooking the contribution of the posterior cornea may not make a huge difference in the outcome for many patients. “Nevertheless, in our practice we look at it in every patient,” he says. “That’s a step you have to take if you want to improve your outcomes. It helps minimize surprises and it improves the percentage of patients seeing well without glasses after toric IOL implantation.”
Dr. Waring adds that it’s good to aim to leave about 0.25 D of with-the-rule astigmatism. “That’s because the astigmatism of the anterior cornea will shift a small amount as the eye ages, from with-the-rule to against-the-rule,” he explains. “Leaving a very small amount of with-the-rule astigmatism will help to offset this change over time.”
5. Are ink marks sufficient to achieve accurate intraoperative alignment?
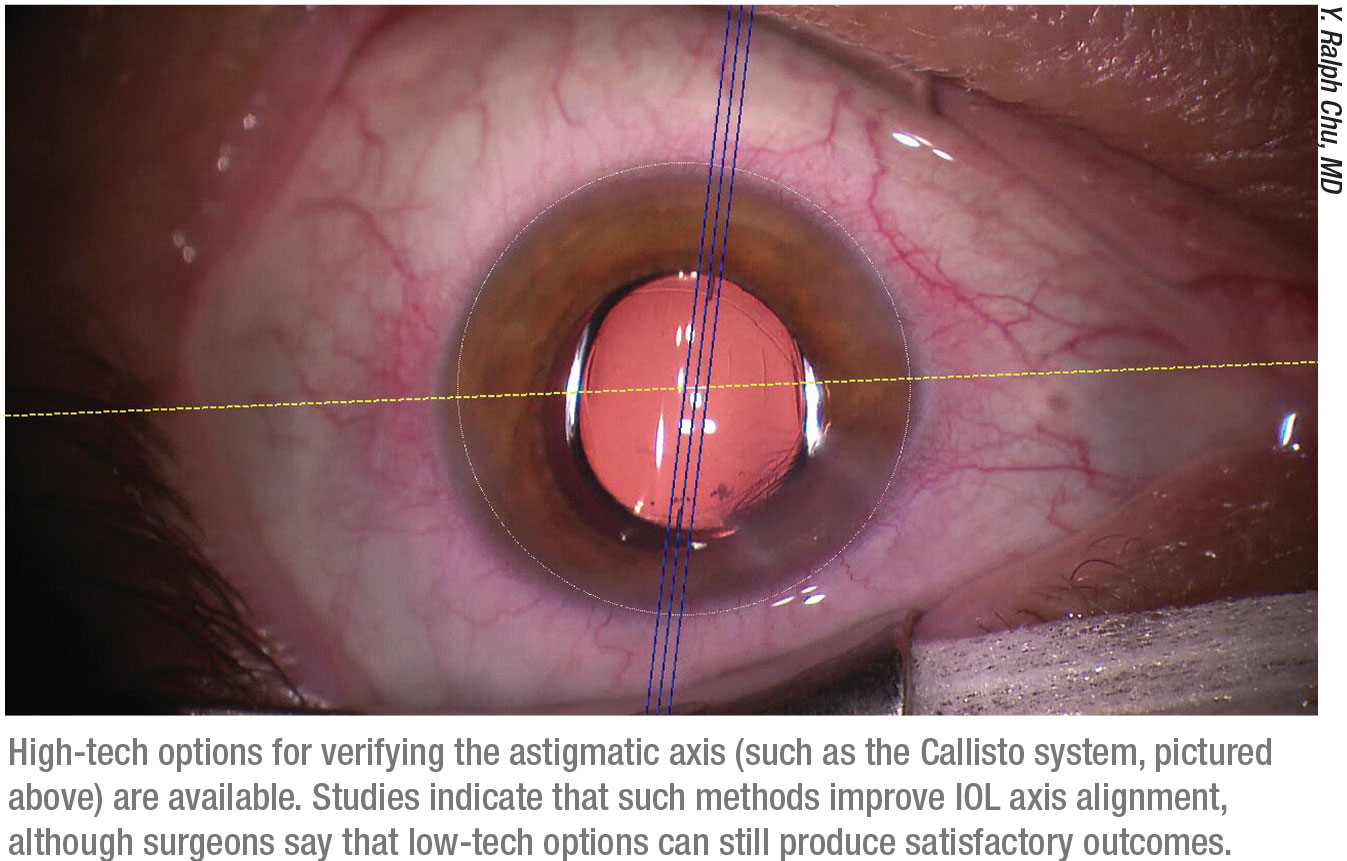
Dr. Chu points out that getting the right axis orientation is critical. “A small percentage of eyes rotate a little when the patient goes from seated to a supine position,” he notes. “So, having a technique that keeps the axis of orientation aligned is key. I think manual marking techniques still work in the hands of an experienced surgeon, but there have been several technological advancements that can increase the accuracy of alignment. In our practice, for example, we use the Callisto guidance system. (See image, p. 29.)
“There are many advanced systems out there,” he continues. “I like the markerless technologies that use digital alignment based on a preoperative corneal image that can be applied in real time during the surgery. Studies have shown that these technologies are indeed more accurate than manual marking methods. However, that doesn’t mean using manual marking is a bad thing. I’ve seen some manual marking devices that work well, and some surgeons have good results even just using anatomic guidelines.”
Dr. Chang agrees that relying on pen ink marking may be less than ideal. “A study by Yasushi Inoue, MD, and colleagues2 showed that 28 percent of the net mean misalignment of toric IOLs at one year is due to surgical misalignment, rather than postoperative rotation,” he says. “The surgeons in this study used ink marking performed at a slit lamp preoperatively. In my experience, digital axis registration is a major improvement over freehand pen marking of the
horizontal axis. We use Zeiss’ Callisto system, which registers the live image from Zeiss’ Lumera 700 microscope with an image obtained from the
IOLMaster 700 evaluation.”
To ensure accurate alignment, Dr. Waring says he uses an intrastromal toric registration mark made with a femtosecond laser. “Systems are being developed for toric alignment that will register preoperative tomography to an intraoperative mark made with a laser, whether it’s in the corneal plane or on the lens plane on the capsule,” he says. “In addition to allowing precise alignment, these archival, intrastromal femtosecond registration marks allow us to check on postop day one to confirm that the lens is indeed in the intended position. Furthermore, if the patient ever has a change in vision in the future, we can look to see if the lens is still properly aligned. We also use an aximeter and toric marker to double-check the alignment.
“Of course intraoperative aberrometry has a role in this setting as well,” he adds. “We don’t currently use it for astigmatism management in our practice, mostly due to inefficiencies and the number of intraoperative variables. We still use it for eyes that have undergone previous refractive surgery, but we’re using it less often even in that situation, mostly because today’s advanced IOL power calculation formulas are so good. The formulas are producing excellent results without the help of the aberrometer. However, we have respected colleagues who rely heavily on intraoperative aberrometry, so it’s another tool in the tool box.”
 |
6. What can I do intraoperatively to minimize postoperative rotation?
These strategies can help:
• Be especially careful about creating and closing the wound. “Meticulous wound construction and wound closure are essential to keeping the lens in position,” says Dr. Waring.
• Avoid using a dispersive OVD. “A dispersive OVD will make the IOL surface more slippery,” notes Dr. Chang.
• Perform an automated capsulotomy. “A uniform capsulorhexis, in terms of size and shape, whether it’s done with a femtosecond laser or using a thermal device like the Zepto, ensures uniform overlap over the edge of the optic,” Dr. Waring points out. “That makes it less likely that you’ll have lens tilt or decentration.”
• Apply a slight posterior pressure to the lens optic after implantation. “This will help to ensure that the optic and haptics are seated in the posterior portion of the capsule,” Dr. Waring explains.
• Be careful to remove all OVD behind the IOL using the irrigation/aspiration instrument. Dr. Chu notes that getting all of the viscoelastic out from behind the lens is critical. “You have to wait until the haptics and the lens have opened up and they’re stable inside the bag,” he says. “Patience counts. Then, once the lens has properly unfolded, make sure all of the viscoelastic is out from behind the lens. Paying attention to those details helps keep the lens in position after surgery.”
• Leave the eye soft at the conclusion of surgery. “Inflating the capsular bag with BSS will make early postoperative rotation more likely,” Dr. Chang says.
7. What does the patient need to know?
Surgeons note that patients should be advised that, while unlikely, a postoperative correction could become necessary. In addition, Dr. Waring points out that you need to meticu-lously educate the patient about avoiding any postoperative internal or external pressure on the eye. “That includes applying zero pressure to the eye in the early postoperative period,” he says.
8. How much postoperative rotation should trigger a correction?
Dr. Chang says that it’s very safe and easy to rotate a misaligned toric IOL in the OR during the first several weeks after surgery. “Nevertheless, many surgeons don’t offer this option to their patients,” he notes. “That deprives those patients of a better refractive outcome.”
Dr. Chang notes that one of his studies, which he co-authored with his partner, Bryan Lee, MD, showed that even under ideal circumstances, a toric IOL can rotate off-axis postoperatively.3 The study also found that not all toric IOLs have the same rotational stability. “Our comparative study of toric monofocal IOLs showed that the AcrySof platform rotated significantly less than the Tecnis platform,” he says. “As a result of this study, Johnson & Johnson Vision carefully studied different design modifications to reduce the rotation of the Tecnis toric IOL. These modifications were recently approved and incorporated into all of their monofocal toric IOLs.” (The Tecnis Toric II, which has these new design features, was just approved in mid-December.)
So: How do you decide that a toric IOL is sufficiently misaligned that it needs to be rotated again postoperatively? Dr. Waring says he has a low threshold for going back in to correct lens alignment—if several conditions are met. “First, the problem has to be the result of lens rotation,” he says. “Second, it has to be causing a meaningful drop in the patient’s uncorrected vision that can be refractively neutralized. Third, the patient’s vision has to be close to a spherical equivalent of plano. Fourth, we have to believe the problem can be resolved by a simple lens repositioning. But it’s rare that we need to do this, using the surgical techniques that I’ve described.”
Dr. Chu says his toric lens patients are refractive surgery patients, and that affects his decision. “We’re not just treating a refraction,” he says. “We’re focusing on the entire patient and how patients are functioning in their lives, and asking if they’re happy with the outcome.”
“Of course, the patient’s opinion is important,” agrees Dr. Waring. “However, we believe that if we optimize the refractive outcome, even when the patient isn’t unhappy—particularly if the patient is ‘lukewarm’ about the outcome—we can go from good to great and move the needle on penetration in the market. We can increase the word of mouth and buzz if we take the extra steps and give the patient the best possible vision. We don’t want patients who are lukewarm about their experience. We want patients who are ecstatic about their outcomes, shouting from the rooftops about how amazingly well they see.”
Dr. Chu says that whether he’d go back into an eye to adjust a lens that’s rotated out of alignment is situation-dependent. “I don’t have a specific degree of rotation that makes me decide to go back in,” he says. “There are many ways of enhancing residual astigmatism after toric IOL implantation besides IOL repositioning, such as laser vision correction and glasses.”
| “Do any re-rotation fairly early—but don’t rush into it.” —Y. Ralph Chu, MD |
9. How long should I wait before going back in to realign the lens?
Dr. Waring says how quickly you go back in to correct a rotation—in the rare case in which it’s necessary—depends on several factors. “Everyone heals differently, but in general, the sooner you make the correction, the better,” he says. “However, in some cases you might want to wait a few days to give the cornea a chance to refractively stabilize. I’d base the timing on the specific circumstances of the case. If the problem is an obvious lens rotation, causing a serious decline in vision, then I wouldn’t wait to address the problem. In that situation, waiting will work against you. But if the problem is subtle, and you don’t feel that the cornea has refractively stabilized, then it’s reasonable to wait a week or two to determine what the issue is.”
“If you do have to re-rotate the lens postoperatively, sometimes it helps to wait a week or so,” says Dr. Chu. “This allows the capsule to contract slightly, which helps keep the lens in a more stable position after re-rotation. So, you don’t have to make a correction the next day. In fact, sometimes if you do, the lens will re-rotate. The bottom line is to do any re-rotation fairly early—but don’t rush into it.”
10. How can I realign a lens as precisely as possible?
“One tool that many ophthalmologists find to be invaluable is the website astigmatismfix.com, created by David Hardten, MD, and John
Berdahl, MD,” notes Dr. Waring. “It’s a free-source website. You enter the refractive data and it will tell you whether or not a rotation is indicated, and if so, in which direction and by how much.”
Dr. Chang agrees. “If a toric IOL is misaligned, we use the astigmatismfix.com online tool to see how much improvement will result if we rotate the lens,” he adds. “If we calculate that there will be a significant refractive improvement, we aggressively suggest this option to patients.”
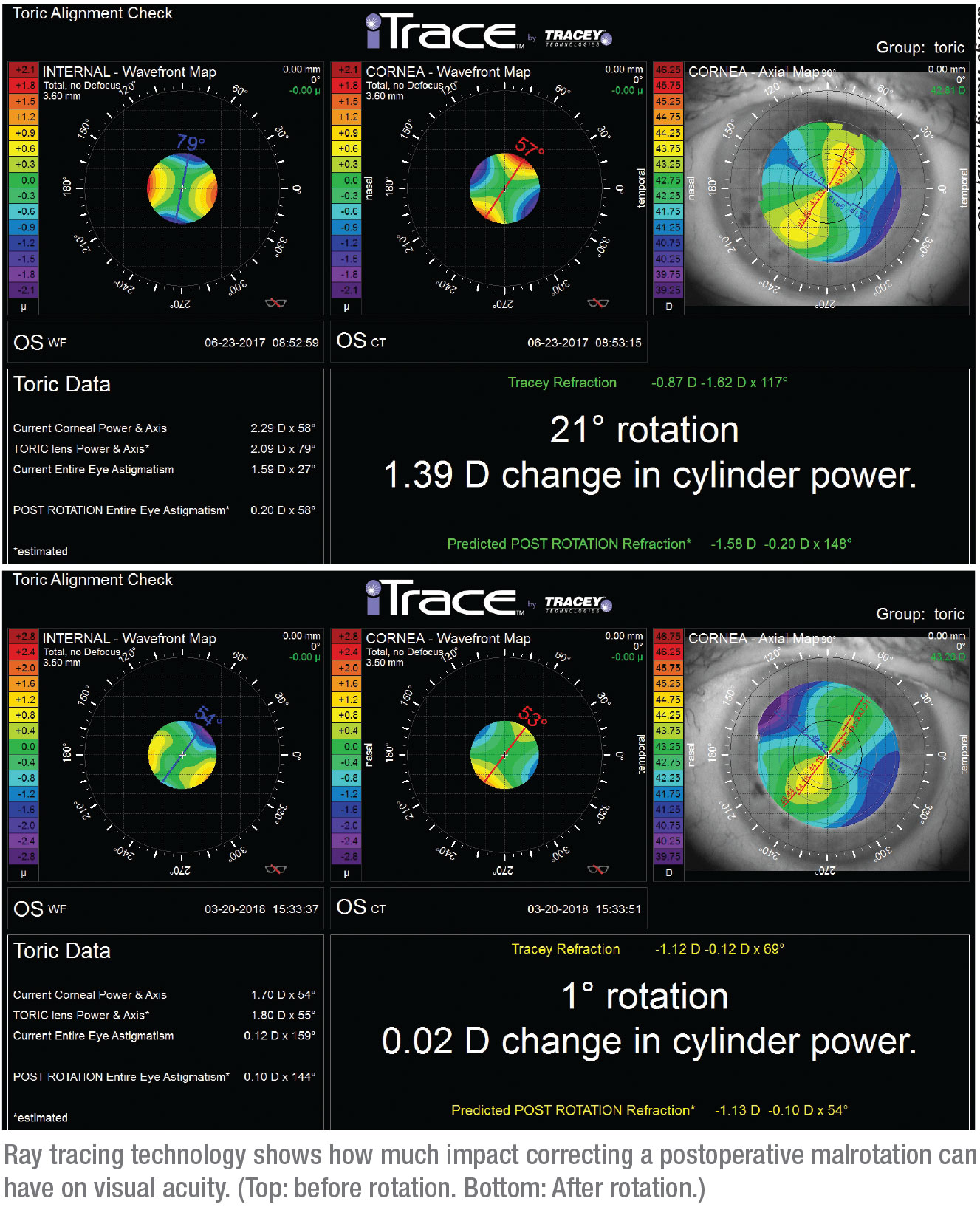
Dr. Waring notes that another helpful instrument—both in terms of de-ciding whether rotating the lens is nec-
essary, and if so, how much rotation should be done—is the iTrace system from Tracey Technologies. “It’s a ray-tracing aberrometer,” he explains. “It can measure the corneal astigmatism and position of the lens and then tell you in real time whether or not a rotation is indicated, and by how much.”
11. Do I need to own the most advanced technology before offering toric IOLs?
“For surgeons just starting to think about toric IOLs the process may seem intimidating, given all the different technologies and tools that are available,” says Dr. Chu. “I don’t think they should be intimidated. The surgical technique for implanting a toric lens is familiar to surgeons. The key steps are obtaining a good topography preoperatively, then marking and confirming alignment intraoperatively.
“The two areas that might be a little challenging for someone offering torics for the first time are deciding when a patient isn’t a good candidate, and attempting to correct a small amount of astigmatism,” he says. “But if you start with someone who has substantial, regular astigmatism—
2 D, for example—you’ll get really good results as long as you align the lens properly.”
What about needing advanced technology to directly measure the refractive impact of the posterior surface of the cornea? “I wouldn’t say it’s essential, but it’s definitely recommended,” says Dr. Waring. “Today’s advanced technology, whether it’s high-res OCT that can directly measure the posterior cornea, or an advanced tomography unit, is giving us much more information, and that can help us get the best possible outcomes.”
Getting It Right
Dr. Chu notes that the most important aspect of all of this is that astigmatism is no longer being overlooked. “We have toric ICLs as well as toric intraocular lenses,” he points out. “More surgeons are performing limbal relaxing incisions. The reality is that thinking about astigmatism and doing what we can to mitigate it has become a critical part of modern cataract surgery.” REVIEW
Dr. Waring is a consultant to Johnson & Johnson Vision. Dr. Chang is a consultant for Carl Zeiss and Johnson & Johnson Vision. Dr. Chu is a consultant to Bausch+Lomb and Carl Zeiss.
1. Ferreira TB, Ribeiro P, Ribeiro FJ, O’Neill JG. Comparison of astigmatic prediction errors associated with new calculation methods for toric intraocular lenses. J Cataract Refract Surg 2017;43:3:340-347.
2. Inoue Y, Takehara H, Oshika T. Axis misalignment of toric intraocular lens: Placement error and postoperative rotation. Ophthalmology 2017;124:9:1424-1425.
3. Lee BS, Chang DF. Comparison of the rotational stability of two toric intraocular lenses in 1,273 consecutive eyes. Ophthalmology 2018;125:1325–1331.