Dry-eye disease can reduce visual quality and adversely affect refractive measurements before cataract and refractive surgery. Additionally, ocular surgery can exacerbate or induce dry eye, which can lead to worsened vision, increased symptoms and dissatisfied patients. Because of this, surgeons say there are steps you can take pre- and postop to minimize the effect of dry eye on your surgical outcomes. To learn how they approach the problem, read on.
An Insidious Problem
“In patients who are cataract surgery age—60 to 90 years old—two-thirds to three-quarters of them are asymptomatic and have ocular surface disease,” says Francis Mah, MD, who is in practice in La Jolla, California. “So, they don’t even know that they have it. A lot of these patients think that it is a normal part of the aging process, like getting gray hair and wrinkles. It has been shown that, especially in the cataract surgery age group, dry eye is very prevalent and is often asymptomatic. We need to be looking for it even if they are not complaining about it.”
He adds that dry eye can affect preoperative measurements. “Before cataract surgery, we are doing biometry and measuring keratometry. It is well-known that dry eye skews biometry and keratometry measurements,” Dr. Mah says. “The same goes for refraction before refractive surgery. Obviously, this can have a huge impact on our surgical outcomes. Sometimes, you get a refractive surprise because of preoperative dry eye.”
Besides less than optimal visual acuity, dry eye can cause postoperative fluctuation in vision and foreign body sensation. “Fluctuation in vision can be anything from blurred edges or blurry images to just overall reduction in vision,” notes Dr. Mah. “Patients may also complain of foreign body sensation or burning.”
According to John Sheppard, MD, of Norfolk, Virginia, there are two key issues with dry eye.1 “One is that you may not be able to assess the proper target for your surgical intervention if the patient has ocular surface disease that impacts the topography and the refractive error in the eye,” he says. “Two, after surgery, untreated ocular surface disease may worsen the recovery and significantly increase the risk of complications, including, rarely, infectious keratitis or conjunctivitis.”
ASCRS OSD Algorithm
 |
Dr. Mah is the chair of the American Society of Cataract and Refractive Surgery’s cornea clinical committee, which recently published a paper in the Journal of Cataract and Refractive Surgery that described an algorithm surgeons can use to prepare their patients for cataract and refractive surgery.2
Surgeons should be looking for dry eye in every surgical patient, says Dr. Mah. “The ASCRS corneal clinical committee has been trying to educate people on looking for dry-eye disease, and ocular surface disease in general, so that outcomes will be better and patients will be happier,” he explains.
Part 1 of the algorithm is a novel preoperative ocular surface disease questionnaire for all patients who are undergoing cataract or refractive surgery. Patients typically fill out the questionnaire before they see their surgeon. “It’s a very simple questionnaire,” Dr. Mah explains. “Because the SPEED questionnaire for dry eyes isn’t proprietary, the ASCRS corneal clinical committee altered it a little bit for our preoperative surgical patients and included some personality questions, which help identify appropriate patients for premium cataract and refractive surgery. Obviously, LASIK patients are premium patients just by their nature. We also ask patients if they are experiencing any dry-eye symptoms. If the SPEED questionnaire is positive or if the patient reports any dry-eye symptoms, then he or she has stage 1 dry eye and dry-eye testing—depending on which tests—can be reimbursed,” Dr. Mah explains.
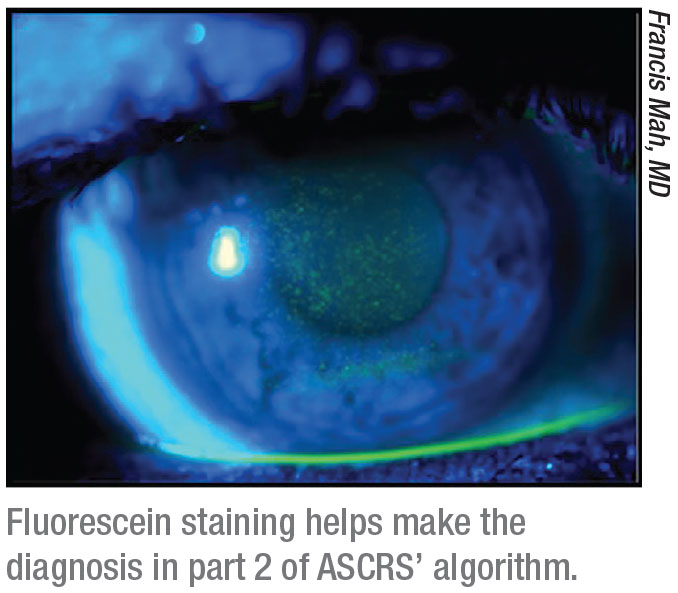
Part 2 of the algorithm is the clinical examination, which includes the look, lift, pull and push examination.1 The algorithm recommends looking at the blink quality and quantity and examining the eyelids. The surgeon should also be looking for signs of anterior and posterior blepharitis and looking at the interpalpebral ocular surface for signs of conjunctival injection, follicles and papillae, discharge and mucus, concretions, conjunctivochalasis, pingueculae, pterygia, conjunctival scarring and symblepharon.1 Also, examine the interpalpebral cornea for any surface abnormality. Then, lift and pull out the upper eyelid, which is an often overlooked part of the ocular surface examination. Finally, push on the lower lid margin, which expresses the meibomian glands, and assess the quality, quantity and flow of the meibum. Vital-dye staining is also important to assess tear-film stability, experts say.
There are many ways to test for dry eye, and some of them are reimbursed. Dr. Mah says that osmolarity testing by TearLab and MMP-9 testing are both reimbursed if a patient has a positive questionnaire or is reporting symptoms. “Other things like meibography and tear assessment by interferometry may not be reimbursed,” he cautions. “Essentially, the next step, regardless of whether the patient says yes or no to any of the questions on the questionnaire, is to do some sort of dry-eye testing. This may just be clinical testing, but that testing can be enhanced with some of the point-of-service tests that are now available. Specifically, in addition to looking at the tear film for staining with vital dyes, I look at the tear meniscus, the superior conjunctiva, and the nasal, temporal and inferior conjunctiva for lissamine green staining, injection and signs of inflammation. I then do a tear-film breakup time with fluorescein. Anything less than 10 seconds on the tear-film breakup time test is abnormal. Then, I push on the lids to assess the meibomian glands and do the osmolarity, MMP-9 and meibography. If any of those tests are positive, we initiate treatment,” Dr. Mah adds.
Part 3 of the algorithm is treatment, which is based on the subtypes and severity of ocular surface disease.
According to Dr. Mah, treatment can include topical steroids, such as loteprednol or fluorometholone, or an FDA-approved dry-eye medication like cyclosporine or lifitegrast. “The algorithm recommends being very aggressive for cataract and refractive surgery patients because they don’t want to wait weeks or months for surgery,” he avers. “Surgeons also don’t want to wait. They want to optimize the surface, optimize their biometry, optimize their topography, optimize their preoperative measurements, and then get going with surgery.
“This is a little bit different than how we normally treat dry eye,” Dr. Mah continues. “Typically, we start off with education, lifestyle changes like taking breaks from computers, and using over-the-counter artificial tears. Then, you kind of ramp up to other therapeutic modalities like using lifitegrast or cyclosporine, or managing the evaporative component by doing lid scrubs or warm compresses or some of these other in-office or even at-home treatments, like BlephEx, NuLids (NuSight), TearCare (Sight Sciences) or LipiFlow (Johnson & Johnson). Before cataract or refractive surgery, you want to be a little bit more aggressive, try to quiet the eyes, and get the eyes normal faster so that you can get repeat measurements and do your surgery, hopefully within two to four weeks.”
According to Rajesh Rajpal, MD, who is in practice in McLean, Virginia, and is the recently appointed chief medical officer for Johnson & Johnson Vision, treating surgical patients often requires a combination of dry-eye treatments. “We would consider artificial tears, meibomian gland treatment—whether it’s warm compresses or a thermal device—and anti-inflammatory medications, as well as evaluating for potential environmental modifications,” he says. “We also consider any contributing medical conditions, as well as any medications that the patient may be taking that can cause a drying effect. It is also critical after initiating appropriate treatment that when we’re measuring for the IOL, we pay attention to the readings. If the ocular surface isn’t ready, then we would either not do the readings or we’d repeat the readings to confirm the surface’s stability before proceeding with surgery,” he says.
Dr. Rajpal adds that it’s often necessary to use a mild steroid in these patients because it frequently allows the surface to improve more quickly, as most patients want to have surgery relatively soon. He emphasizes the importance of detecting and treating dry eye that’s present preoperatively so that the patient doesn’t think it was caused by the procedure. “Postoperative treatment regimens are generally similar to preoperative treatments. We also want to make sure that the perioperative medications, such as antibiotic or nonsteroidal anti-inflammatory medications aren’t causing some irritating or toxic effect,” he cautions.
According to Dr. Mah, following this algorithm will produce better results in dry-eye patients. “That’s been shown; you’re definitely going to get better results by, number one, thinking about ocular surface disease; number two, diagnosing ocular surface disease; and then number three, treating ocular surface disease prior to doing any surgery,” he says. “I think it has to be a mindset that you go into examining these people and trying to identify these patients prior to any of your measurements, and definitely before the surgery. You’ll get better results.”
Postoperative Outcomes
To achieve the best postoperative outcome, the key is to manage ocular surface disease preoperatively and carry management through the perioperative period, says Dr. Sheppard. “Prior to measurements, we give them preservative-free tears, a topical anti-inflammatory like cyclosporine or lifitegrast, or a steroid, specifically loteprednol,” he says. “We put them on some type of lid hygiene, we give them oral essential fatty acids, we place a punctal plug, and we often go to the second tier of therapy with thermal pulsation or other means of rapidly improving their lid component. Once the surface is clear, the measurements are taken and the surgery is performed, we maintain the patient on that same preoperative regimen because a corneal or lens-based refractive procedure places a great deal of stress on the ocular surface. It anatomically damages—hopefully temporarily—the corneal nociceptor nerve complex, and the addition of perhaps stronger and preserved medicines can also temporarily stress the ocular surface.
“This concept is particularly true for the cataract patient, especially if one is performing a limbal relaxing incision, because the primary and secondary incisions sever corneal nerves, and limbal relaxing incisions sever even more corneal nerves,” Dr. Sheppard continues. “That’s one motivation for me to recommend a toric intraocular lens instead of a limbal relaxing incision. We now have a 0.75-D toric lens from Bausch and Lomb, so we can treat the patient’s astigmatism in almost all circumstances with an intraocular lens that does not in any additional way disturb the ocular surface. The stress of cataract surgery, of course, also involves a bright light in the eye, a speculum holding the eye open, excessive drying and extra medicines—such as steroids, nonsteroidal anti-inflammatory drops, and antibiotics—that can damage the ocular surface, as well.”
Dr. Sheppard explains that the management strategies for dry eye move along a continuum. “Pre-, intra- and postoperative measures are very important,” he says. “In some severe cases, we immediately resort to higher-order therapies. Some practices use intense pulsed light, Maskin probes [Rhein Medical], TearCare or BlephEx. We use thermal pulsation. We often use an amniotic membrane to ‘quick tune’ the ocular surface. Severe cases may need more drops, more plugs, additional surface procedures and more visits. The ultimate goal is to normalize topography and obtain an outstandingly consistent manifest refraction.” REVIEW
Dr. Mah has a financial interest in Allergan, Novartis, Sun, TearLab, Kala Pharmaceuticals, J&J Vision, NuSight and SightSciences. Dr. Sheppard has a financial interest in Alcon/Novartis, Kala, Lacriscience, Novaliq, Noveome, Ocular Therapeutix, Shire and TearLab.
1. Roberts CW, Elie ER. Dry eye symptoms following cataract surgery. Insight 2007;32:1:14-23.
2. Starr CE, Gupta PK, Farid M, et al, the ASCRS Corneal Clinical Committee. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg 2019;45:5:669-684.



