AS CATACRACT SURGERY IS BECOMING more like refractive surgery, more and more patients are asking for and expecting to see better without their glasses. One option cataract surgeons can select is a toric intraocular lens to provide patients with better uncorrected near and distant vision.
The Staar Toric Intraocular Lens, a silicone plate lens, is the only toric lens currently approved in the United States. It is available in two powers. The lower power can correct upwards of 2 D and the higher power can correct 3 D. The Alcon AcrySof toric IOL is currently under investigation, and we hope to have it available soon.
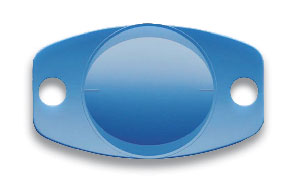
The Staar Toric Intraocular Lens, a silicone plate lens, is the only toric lens currently approved in the United States. An Alcon AcrySof toric IOL is in clinical trials.
Treatment Options
For the lower amounts of astigmatism (1 D to 1.25 D or less), I treat with astigmatic keratotomy. I primarily use limbal relaxing incisions in the axis of the steep meridian to minimize or reduce the astigmatism. I am careful not to overcorrect because patients usually tolerate some residual astigmatism better than they do if their axis is changed.
For astigmatism greater than 1.25 D, I use a toric IOL. With toric IOL implantation, I evaluate the patient's corneal astigmatism prior to surgery.
In most cases, the corneal astigmatism and the refraction are the same. In some instances, they are different, and we often associate that with lenticular astigmatism. However, this is not a guarantee. Occasionally, the patient could also have staphyloma or retinal pathology. (Most of the time, lenticular astigmatism and corneal astigmatism usually add up to the total astigmatism in a prescription.)
With cataract surgery, I focus on the corneal astigmatism and assume that what is in the lens will be corrected when the cataractous lens is removed.
The Procedure
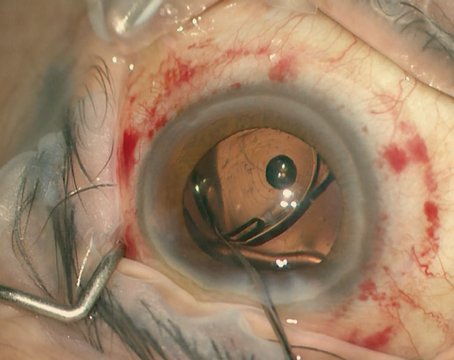
As always, the surgery should be pristine. In addition, the capsulorhexis should be the proper size (5 to 5.5 mm) to ensure that there is an adequate seal of the anterior rhexis overlying the optic edge.
I do two things differently with patients who receive toric IOLs. First, I mark the patients preoperatively at the 3 o'clock and 9 o'clock axes by having them sit up before they lie down. Then I tape the topography adjacent to the operating microscope and make sure when I place the lens in the eye that I orient it in the direction of the astigmatism along the steep axis consistent with the corneal topography.
For the first few cases of toric lenses that I implanted, I would streak the patient on the table to confirm that the lens was in the proper axis. I used to streak patients with the viscoelastic in, then I would remove the viscoelastic, and then streak them one more time to check for rotation.
I do not perform this step anymore, because I have found that my orientation and my streak retinoscopy were almost always one and the same. Surgeons who are new to the toric IOL procedure can streak their patients when the viscoelastic is out.
Afterwards, I have patients lie flat in the holding area for 30 minutes, which is not a step I normally recommend with other lens implantation. This helps ensure that the anterior-posterior capsules form a small seal to keep the lens in position.
When they leave the hospital, I also advise patients to lie down at home and try to stay flat as much as possible for the first day. Then, I confirm the orientation of the lens on postop day one to make sure it has not rotated.
On occasion, the lens does rotate. It is a plate lens, so one size does not fit all. Some surgeons have found that if the lens is inserted upside down it is less likely to rotate. However, this technique does decrease the effect of the astigmatism correction by 0.25 D to 0.50 D. In my experience, by having patients lay flat, the incidence of rotation is less than 5 percent.
Postop Considerations
In the case of rotation, a different set of circumstances occurs. While some surgeons rotate the lens at the slit lamp. I do not. Instead, I return the patient to the surgery suite. There, I enter through the original paracentesis and inject a very small amount of viscoelastic. I open the bag up, rotate the lens to the proper position, evacuate the viscoelastic, and have the patient lie flat for 30 minutes. I have not had a toric IOL rotate a second time.
|
|
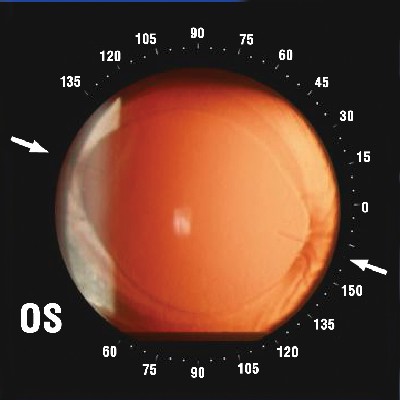
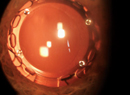
| • Retroillumination photograph of a toric IOL two weeks after implantation. • Axis determined with a protractor. |
In cases in which the lens needs to be rotated, it is best to do it early, because once the capsule is fused through the holes in the plate haptic it can be harder to reopen. If I am planning to rotate one of these toric IOLs, I usually like to do it in the first two to four weeks of surgery.
In addition, I am very cautious about time for Nd:YAG capsulotomy. I wait a minimum of six months because of previous reports in the literature that demonstrated the potential for plate lenses to dislocate to the vitreous. However, this is less likely with the newer plate lens designs.
If cortical cleanup is done properly, Nd:YAG capsulotomy should not need to be done much earlier. Regardless, I try to be conservative with the timing of the YAG capsulotomy.
Any residual astigmatism at that point can be corrected with limbal relaxing incisions or LASIK. In the past, I have had a few patients who have had more astigmatism than can be corrected with a toric lens alone. In those instances I perform bioptics. It is helpful to treat partially with LASIK and partially with a toric IOL, rather than entirely with LASIK, because the optical zone would be bigger with bioptics and less surgery is needed.
For this technique, I cut a LASIK flap only, replace the flap, and then bring the patient in a month later to measure the corneas. Then I base IOL calculations on the keratometry measurements, and implant the lens. One month postop, the flap is lifted and I can treat residual myopic astigmatism or astigmatism.
For cases in which I know I will do bioptics, I leave the patients with a small amount of myopia. The procedure tends to work better to treat myopic astigmatism than hyperopic astigmatism.
Toric IOL implantation effectively provides patients with better uncorrected near and distant vision. The procedure can be a valuable part of a surgeon's armamentarium.
Dr. Solomon is a professor of ophthalmology and director of cornea and anterior segment at the Magill Laser Center for Vision Correction at the Medical University of South Carolina. Contact him at (843) 216-2020 or Solomonk@musc.edu. He has no financial interest related to this article.