A Drug-Eluting Contact Lens
For many years researchers have attempted to create a contact lens that, in addition to meeting the refractive needs of a patient, would allow a drug to gradually seep out onto (and into) the eye for an extended period of time. This turned out to be difficult.
One team that has made major headway along these lines is a group in Boston, led by Daniel S. Kohane, MD, PhD, professor of anaesthesia and director of the Laboratory for Biomaterials and Drug Delivery at Harvard Medical School, and Joseph B. Ciolino, MD, at Harvard Medical School and the Massachusetts Eye and Ear Infirmary. Their team has developed a contact lens that elutes a drug at a consistent level for—in some cases—months, in in vivo studies using rabbits.
Dr. Kohane explains. “People have been trying to create something like this for decades,” he says. “In most cases, the results have allowed release of a drug for several hours or a day. In contrast, our lens has been shown, in vitro, to be capable of releasing substantial amounts of a drug over a period of months with relatively constant kinetics, so the same amount is released every day.”
Dr. Kohane says that the lens they’ve developed is a bit like a sandwich. “There are two layers of hydrogel material similar to a standard contact lens,” he says. “In between those layers is a flat doughnut that’s made of a polymer containing a drug. The hole in the doughnut overlies the pupil so you can see through it.”
Dr. Kohane notes that several things enable the lens to be effective for multiple months. “First of all,” he says, “this is local therapy and the drugs we’re testing tend to be very potent. Second, the polymer doughnut is a macroscopic object, which means we can pack a lot of drug into it—more than any other device that I’m aware of. That, and the specific polymeric composition of the material that allows the slow and even release of the drug account for our success.”
Controlled Release
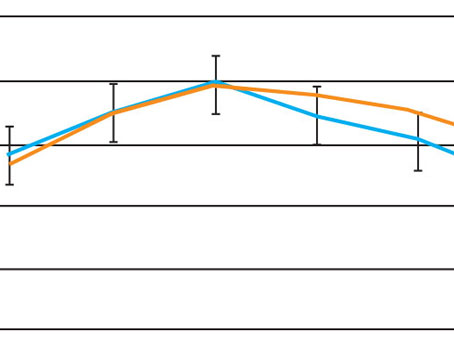
Dr. Kohane explains that the drug is eluted through a combination of drug diffusion and biocompatible polymer degradation. “When we tested the system with an antibiotic, we found that the drug was still being released evenly at three months, as documented in a paper we published at the time.1 We also tried the lens with econazole, an antifungal, and it was still working at three weeks. Our most recent study used latanoprost, a glaucoma medication, and we got good steady-state release and penetration into the anterior chamber for a month, which we measured by doing serial fluid withdrawals from the anterior chamber.2 We’ve tried this with both hydrophilic and hydrophobic drugs, and both worked.”
Dr. Kohane says the speed at which the drug is released can easily be altered. “There are lots of parameters you can play with to get the release characteristics you want, including the ratio of polymer to drug, the nature of the polymer and the thickness of the polymer film,” he says. He adds that biocompatibility has not been a problem so far, although human testing will be necessary to confirm that this extends to people.
|
Trials with dogs and non-human primates have already begun. “As those trials wind down we’ll start lining up human trials,” he says.
A High-Tech Eye Drop
Another promising approach to long-term drug delivery is under development at the University of Pittsburgh McGowan Institute for Regenerative Medicine and UPMC Eye Center in Pittsburgh. In this technology, drug-imbued microspheres are embedded in a reverse-thermal gel liquid that becomes a flexible, shape-conforming solid when it reaches body temperature. The patient can place a drop of the gel in the fornix, where it remains for an extended period while the microspheres slowly elute their drug content. The research, being conducted by Morgan V. Fedorchak, PhD, Steven R. Little, PhD, Ian Conner, MD, PhD and Joel S. Schuman, MD, is showing promise as a means to circumvent issues of patient adherence. (The University of Pittsburgh has applied for a patent.)
“Using a rabbit model, we found that if we injected the microspheres subconjunctivally they provide IOP reduction for as long as a month,” says Dr. Schuman. “When I heard about the reverse-thermal gel I wondered whether we could combine the gel with the microspheres to circumvent the need for the injection. It turns out this works just fine, so we switched from injecting the microspheres to putting them in the gel. The substance comes out of the bottle as a drop; it warms up against the eye and becomes a flexible solid that conforms to the shape of the fornix, where it can remain as long as necessary. We’ve tested drug delivery lasting a month, but that length of time could be made shorter or longer as necessary.
“Our goal is to be able to enhance adherence to therapy by giving patients the ease of just taking a drop once a month instead of multiple times,” he continues. “Having the drug available as an eye drop should eliminate some of the problems we saw with the Ocusert device many years ago. The drug we tested in this case was brimonidine, but you could have any drug in this vehicle. This technology should allow a patient to undergo treatment for a long period of time with minimal effort, which we believe will enhance the effectiveness of treatment.”
Dr. Schuman notes that eye rubbing shouldn’t be a problem. “We haven’t tested the device in a human cohort yet, but there’s no reason to think this would be a concern,” he says. “This approach might be contraindicated if a patient constantly rubs his eyes, but generally that should not be a problem.
“Right now we’re testing it in animals and it’s working great,” he adds. “Of course, lots of things work in animals that don’t work in humans, so we’re keeping our expectations realistic. But we’re very hopeful, because the studies so far have given us a lot to be encouraged about. Next, we’ll most likely be looking to file with the FDA.” REVIEW
1. Ciolino JB, Hoare TR, Iwata NG, Behlau I, Dohlman CH, Langer R, Kohane DS. A drug-eluting contact lens. Invest Ophthalmol Vis Sci 2009;50:7:3346-52.
2. Ciolino JB, Stefanescu CF, Ross AE, Salvador-Culla B, Cortez P, Ford EM, Wymbs KA, Sprague SL, Mascoop DR, Rudina SS, Trauger SA, Cade F, Kohane DS. In vivo performance of a drug-eluting contact lens to treat glaucoma for a month. Biomaterials 2014;35:1:432-9.