In a September presentation to the 34th Congress of the European Society of Cataract and Refractive Surgeons in Copenhagen, Denmark, Dr. Will demonstrated his novel system, which supplements the AcuTarget HD (AcuFocus) diagnostic and surgical planning tool by providing direct intraoperative guidance for KAMRA centration. “We still recommend the AcuTarget HD as the final gold standard,” he notes. “The challenge is that to use the AcuTarget HD, the patient must be moved from the OR to the AcuTarget HD, and then back to the OR if inlay position is unacceptable.” This back-and-forth, he cautions, might lead surgeons to settle for suboptimal KAMRA placements to maintain efficiency in the operating room.
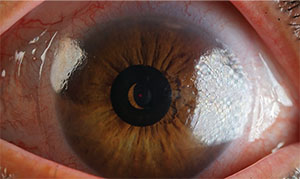 |
| The KAMRA inlay’s position is analyzed intraoperatively in the OR by the system’s metrology software, which was developed by Brian Will, MD. |
Dr. Will’s repurposed digital camera and its accompanying software helps KAMRA inlay surgery flow smoothly without sacrificing precision, to help spare patients from subsequent repositioning surgery. “In some cases the inlay surgery is performed in a dedicated surgical center that may not have an AcuTarget HD system, where the system is in a different clinic miles away. As a result, the centration can’t be checked until another day—a bit too late to make intraoperative adjustments,” he says. “The value of this system is speed and the ability to make accurate decisions intraoperatively.”
Dr. Will’s invention uses a digital camera because, unlike a surgical microscope with a camera attached, it provides a single-lens, coaxial view of the surgical field, elimating offset error. The Sony Alpha a7 RII digital camera has a 44-MP sensor, and a black-and-white setting aids centration in eyes with dark irides. “We need the highest resolution possible to mitigate against image pixelation caused by the digital sensor in the camera,” he says.
Clear, error-free visualization is critical to outcomes that will enhance near vision while minimizing impact on distance vision in the implanted eye. Using his system in the OR, Dr. Will can get constant feedback and redirection, positioning the KAMRA in the stromal pocket until he hits his target, which is pre-programmed into his software.
“We have a software program that performs the necessary calculations, then provides the surgeon with a graphic showing target position, achieved position and the metrics describing the centration error. It also provides directions on where to move the inlay, and by how much, in order to bring achieved position versus target to an acceptable margin,” he explains. Another plus of the digital camera is immediate transfer of images onto his computer workstation. “We can’t be sitting around waiting to pull an SD card or take one photo at a time,” Dr. Will notes.
At the ESCRS meeting, he discussed the use of his system in 24 patients. He explains, “Using the feedback from our system, we were able to obtain much better accuracy compared to the method of using just the AcuTarget HD, as we could quickly move the inlay based on the intraoperative feedback from the system, without having to move the patient.” He compared 42 consecutive eyes implanted with KAMRA using manual marking and deductive reckoning based on anatomic landmarks in the OR, to 24 consecutive eyes implanted using his camera-based centration system in the OR. Dr. Will’s experimental group showed a significantly lower average centration error, at 85 µm (standard deviation: 24 µm; range: 22 to 155 µm), versus 171 µm (standard deviation: 33 µm; range: 57 to 263 µm) for the manual-marking group.
Dr. Will’s adaptation of a conventional camera body is garnering the interest of surgeons and vendors alike. “We are considering taking this system to a commercial product,” he says. Although its current iteration is meant to assist in KAMRA inlay surgery, he thinks its applications could expand. “We believe that it can be used to check inlay position for the Raindrop (ReVision Optics, Lake Forest, Calif.) and Flexivue inlays (Presbia, Irvine, Calif.), as well,” he says. REVIEW
Dr. Will has no financial relationships to any of the companies mentioned in this article.



