These features were suggestive of an epithelial downgrowth cyst or, more
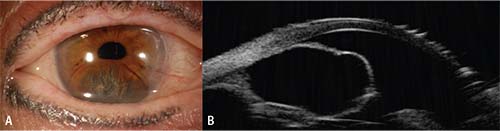 |
| Figure 3. One year after aspiration and cryotherapy, the right eye shows recurrence of the cyst (A). On UBM, the cyst was extending into the anterior chamber, distorting the pupil and adherent to the endothelium (B). However, it was smaller than it had been prior to treatment. |
One year later, the patient returned with recurrent symptoms. On examination, her best corrected visual acuity was 20/80 OD and 20/30 OS. Anterior segment assessment OD again revealed a large cystic mass at the inferior region of the iris measuring 7 mm x 4 mm and with endothelial touch inferiorly (Figure 3A). UBM disclosed recurrence of the cystic iris lesion with endothelial touch (Figure 3B). Treatment options were reviewed, and the patient underwent fine needle aspiration with ethanol irrigation (alcohol sclerosis of the cyst wall). Postoperatively, the patient noted improvement of symptoms.
On one month follow-up, there were no visual symptoms and visual acuity and intraocular pressures remained stable. External and slit lamp examination showed that the partially deflated flat-surfaced cyst was hung up on the endothelium anteriorly and the lens capsule posteriorly.
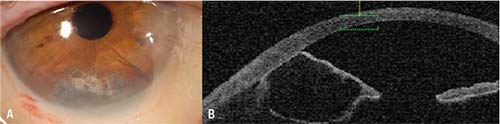 |
| Figure 4. One month after aspiration and alcohol-induced sclerosis, the right eye shows clinical resolution (A), but OCT documents a partially involuted, flat-surfaced cyst adherent to the endothelium and the lens capsule (B). |
Discussion
Iris tumors are characterized as either solid or cystic.1-4 Solid iris tumors are more common than cystic, accounting for 79 percent vs. 21 percent of cases, respectively.2-4 Iris cysts can be further classified as primary or secondary cysts.1-6 Primary cysts are categorized anatomically into iris pigment epithelium (IPE) cysts and iris stromal cysts. Secondary cysts are categorized by etiology into epithelial downgrowth cysts, cysts secondary to intraocular tumors, and parasitic cysts.1-4
Primary IPE cysts are the most common type of iris cyst and the second most common iris tumor, following iris nevus, accounting for 19 percent of all iris tumors.3-5 IPE cysts are classified as pupillary margin, midzonal, peripheral, dislodged and free-floating.1-5 Peripheral and midzonal cysts are the most frequent, accounting for 72 and 21 percent of IPE cysts, respectively.1-5 IPE cysts tend to have a benign clinical course. Importantly, pupillary margin IPE cysts can be associated with a mutation of smooth muscle alpha-actin2 (ACTA2) and the smooth muscle gene (MYH11), which have been associated with thoracic aortic artery aneurysm and dissection.7-10
Iris stromal cysts are far less common than IPE cysts, representing only 3 percent of all iris tumors. These cysts are categorized as either congenital or acquired.1-4,6 Iris stromal cysts are characterized as a unilateral, smooth-surfaced, translucent mass and often contain a fluid-debris level.1,3,4,6 A series of 17 congenital iris stromal cysts found that, compared to older patients, patients younger than 10 had a more aggressive cyst that resulted in worse visual prognosis.6 Iris stromal cysts have a propensity to recur, and there are several proposed treatments in the literature.6,11-19
The appearance of the cystic lesion in our patient is classic for an acquired iris stromal cyst. However, the patient’s history of previous ocular surgery encourages the consideration of an epithelial downgrowth cyst. Similar treatment modalities can be considered for both entities. The patient initially underwent treatment elsewhere with Nd:YAG laser prior to presentation. Nd:YAG laser cystotomy involves laser-induced puncture of the cyst wall in a non-invasive manner, but this tends to have a high rate of recurrence due to healing of the rupture and reformation of the cyst.11-13
Fine needle aspiration of the cyst can also be performed but tends to result in a fairly high recurrence rate, especially if the cyst occurs in a younger individual.6 Multiple surgical resection techniques have been described for simple unroofing of a cyst, complete cyst removal, and en bloc cyst plus partial cornea/sclera removal.6,14-18 Shen et al., described four cases of congenital iris cysts that underwent surgical excision and microdiathermy which resulted in no recurrence on one to six years of follow-up.14 Shin et al., described aspiration combined with endophotocoagulation and cryoablation for recurrent iris stromal cyst that resulted in resolution and no recurrence at 43 months of follow-up.15 There have been attempts to treat both iris stromal cysts and epithelial downgrowth cysts with aspiration and chemical irrigation using agents such as 5-fluorouracil, mitomycin-C and absolute ethanol.16-19 One study described using intracystic ethanol irrigation to treat 99 epithelial iris cysts, which led to resolution in 93 of 99 after one procedure, 96 of 99 after two procedures and 98 of 99 after three procedures.18 One of this case report’s co-authors, Dr. Shields, utilized a modified technique in the treatment of 16 patients with iris stromal cyst using aspiration and alcohol-induced sclerosis with special T-connector tubing.19 Control of the cyst with involution or stabilization was achieved in 14 of 15 patients, 10 of which improved after a single treatment.19
In conclusion, iris cysts represent a broad group of lesions with a varied natural course, systemic associations, prognoses and treatment modalities. Iris stromal cysts and epithelial downgrowth cysts are often burdened with a high rate of recurrence and may require multiple procedures to control. Aspiration with alcohol-induced sclerosis appears to be an effective alternative in the management of these lesions without the need for open surgical resection. REVIEW
1. Shields JA. Primary cysts of the iris. Trans Am Ophthalmol Soc 1981;79:771-809.
2. Shields JA, Shields CL. Intraocular Tumors: An Atlas and Textbook. 3rd ed. Philadelphia: Wolters Kluwer/Lippincott Wiliams & Wilkins, 2016.
3. Shields CL, Kancherla S, Patel J, et al. Clinical survey of 3680 iris tumors based on patient age at presentation. Ophthalmology 2012;119:2:407-14.
4. Shields CL, Shields PW, Manalac J, et al. Review of cystic and solid tumors of the iris. Oman J Ophthalmol 2013;6:3:159.
5. Lois N, Shields CL, Shields JA, Mercado G. Primary cysts of the iris pigment epithelium. Clinical features and natural course in 234 patients. Ophthalmology 1998;105:10:1879-85.
6. Lois N, Shields CL, Shields JA, et al. Primary iris stromal cysts. A report of 17 cases. Ophthalmology 1998;105:7:1317.
7. Shields JA, Magrath GN, Shields C, et al. Dissecting aortic aneurysm 55 years after diagnosis of iris flocculi. Ocul Oncol Pathol 2016;2:4:222-225.
8. Guo DC, Pannu H, Tran-Fadulu V, et al. Mutations in smooth muscle alpha-actin (ACTA2) lead to thoracic aortic aneurysms and dissections. Nat Genet 2007;39:12:1488-93.
9. Risma TB, Alward WL. Successful long-term management of iris flocculi and meiosis in a patient with a strong family history of thoracic aortic aneurysms and dissections associated with an MYH11 mutation. JAMA Ophthalmol 2014;132:778–780
10. Disabella E, Grasso M, Gambarin FI, et al. Risk of dissection in thoracic aneurysms associated with mutations of smooth muscle alpha-actin 2 (ACTA2). Heart 2011;97:4:321-6.
11. Gupta V, Rao A, Sinha A, et al. Post-traumatic inclusion cysts of the iris: A long-term prospective case series. Acta Ophthalmol Scand 2007;85:8:893-6.
12. Gupta A, Pandian DG, Babu KR, Srinivasan R. Primary stromal iris cysts treated successfully with ab externo laser Nd:YAG photocoagulation. J Pediatr Ophthalmol Strabismus 2010;47:Online:e1-4.
13. Baranwal VK, Kumar S, Gaur S, et al. An uncommon case of primary iris cyst managed with Nd YAG laser. Med J Armed Forces India 2015;71(Suppl 1):S82-4.
14. Shen CC, Netland PA, Wilson MW, Morris WR. Management of congenital nonpigmented iris cyst. Ophthalmology 2006;113:9:1639.
15. Shin SY, Stark WJ, Haller J, Green WR. Surgical management of recurrent iris stromal cyst. Am J Ophthalmol 2000;130:1:122.
16. Yu CS, Chiu SI, Tse RK. Treatment of cystic epithelial downgrowth with intralesional administration of mitomycin C. Cornea 2005;24:7:884-6.
17. Shaikh AA, Damji KF, Mintsioulis G, et al. Bilateral epithelial downgrowth managed in one eye with intraocular 5-fluorouracil. Arch Ophthalmol 2002;120:10:1396-8.
18. Behrouzi Z, Khodadoust A. Epithelial iris cyst treatment with intracystic ethanol irrigation. Ophthalmology 2003;110:8:1601
19. Shields CL, Arepalli S, Lally EB, et al. Iris stromal cyst management with absolute alcohol-induced sclerosis in 16 patients. JAMA Ophthalmol 2014;132:6:703-8.



