A 38-year-old Hispanic woman presented to the Wills Eye Hospital emergency department with a four-day history of left greater than right eye decreased vision.
Recent medical history revealed admission to the Neurology service at our hospital two months prior for headaches and optic disc edema in the right eye. Inpatient ophthalmology consultation was obtained, and an evaluation for typical and atypical causes of optic nerve edema was recommended. Serologic workups for lyme, sarcoidosis, syphilis and tuberculosis were negative. Magnetic resonance imaging of the brain, orbit and cervical and thoracic spine was negative for optic nerve enhancement or demyelinating lesions. Chest radiography showed no infiltrates or lymphadenopathy. Lumbar puncture for infectious and autoimmune etiologies of optic nerve edema returned normal results. She had been empirically diagnosed with idiopathic optic neuritis and treated with three days of high-dose IV methylprednisolone with resolution of her symptoms. She was discharged on an oral taper of prednisone with gradual return of her symptoms bilaterally after she had completed the taper. Review of systems during her current presentation revealed left-sided headache, malaise, nausea, vomiting, photophobia and neck pain.
 |
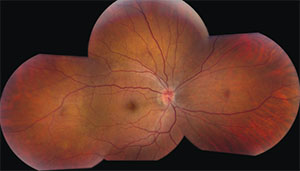
| Figure 1B. The left eye displays serous macular detachment, multifocal exudative retinal detachments temporal to the macula and optic disc edema. |
Medical History
Past medical history revealed migraines, hypothyroidism and anxiety. Social history was unremarkable. Family history disclosed a sister with sarcoidosis.
The patient’s medications included oxycodone for chronic lower back pain, as well as carisoprodol, nortryptiline, clonazepam and levothyroxine.
 |
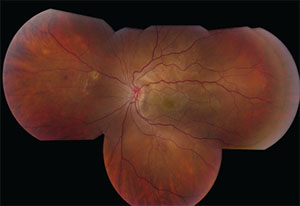
| Figure 1A. Fundus photograph of the right eye showing retinal pigment epithelial mottling and optic disc edema. |
Examination
Corrected visual acuity was 20/30 in the right eye and count fingers at three feet in the left eye. A relative afferent pupillary defect was present in the left eye. Intraocular pressure was 12 mmHg in both eyes, and extraocular motility was full. Confrontation visual fields were full in the right eye but could not be assessed in the left eye due to decreased visual acuity. Anterior segment exam showed 2+ temporal conjunctival injection, fine keratic precipitates and 1+ anterior chamber cell and flare, as well as trace vitreous cell in both eyes.
Dilated examination of the right eye showed faint retinal pigment epithelium changes in the macula and 1+ nerve edema with mild hyperemia. The left eye revealed a multi-lobed serous retinal detachment involving the macula and multiple serous retinal detachments temporal and nasal to the macula (See Figure 1).
Please click this link for diagnosis, workup, treatment and discussion.



