Here is a look at two VR cataract surgery simulators: the venerable Eyesi (VRMagic, Manheim, Germany) and relative newcomer MicroVisTouch (ImmersiveTouch, Chicago).
MicroVisTouch
Shameema Sikder, MD, director of Johns Hopkins University School of Medicine’s Center of Excellence for Ophthalmic Surgical Education and Training, says her program is an early adopter of the MicroVisTouch. “We have one; the University of Illinois at Chicago has one. We set one up at our sister institution in Saudi Arabia. I know that they’re working on getting it distributed throughout China and India,” says Dr. Sikder, who is also an unpaid advisor to ImmersiveTouch.
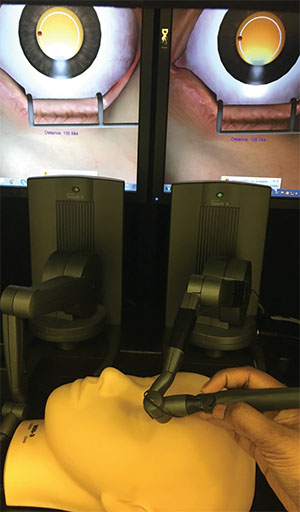 |
| The MicroVisTouch features a blunt-tip handpiece attached to a robotic arm. The virtual reality platform transforms the handpiece into whichever cataract instrument the trainee needs to perform a given surgical step during a simulated procedure. |
The MicroVisTouch can simulate the capsulorhexis, clear corneal incision and phacoemulsification steps of cataract surgery, and additional modules representing other steps are in the works. The MicroVisTouch doesn’t come with a tangible set of instruments: instead, a robotic arm holds a handpiece “that looks kind of like an enlarged pen,” according to Dr. Sikder; trainees hold that blunt-tip instrument to simulate the appropriate instrument for whatever stage of surgery they are performing. In the VR immersion, the handpiece becomes a keratome, hook or forceps, for example, as the simulated procedure requires. One key difference between the MicroVisTouch and the Eyesi is that while the MicroVisTouch has a model head like the Eyesi does, the surgical trainee doesn’t interact with it in the same way. It’s there only for the trainee to practice proper hand placement on the patient’s forehead and cheek as part of the surgeon’s real-life posture.
Although MicroVisTouch users don’t touch a physical representation of a patient in the same manner as Eyesi users, ImmersiveTouch claims that they experience haptic feedback—something new to the VR cataract surgery simulator market. “One could argue that microsurgery is largely visual,” says Dr. Sikder. “How much are you really feeling when you’re tearing a 15-micron membrane when you’re doing capsulorhexis? But there are certain steps that do have tactile feedback. For example, when you’re making a clear corneal incision in cataract surgery, that situation does offer tactile feedback in real life. To be able to simulate that adds value to the trainee’s experience.
“It closely
 |
| The MicroVisTouch cataract surgery simulator has foot pedals that allow trainees to practice the phacoemulsification step. |
Dr. Sikder and colleagues studied VR phacoemulsification simulators, and were able to validate the MicroVisTouch’s ability to improve capsulorhexis skills,3 but she acknowledges that validating the benefits to residents of having access to a VR simulator of any type is challenging. “What we’re relying on, diffusely, is anecdote,” she says, “and then some of the studies we are trying to do attempt to validate the existence of a skill improvement, or quantify how much a skill improved or determine which interventions led to the most improvement. In my current position, we’re looking at technology, and we’re trying to understand how we can assess surgical skills.”
Eyesi
The Eyesi is the most prevalent of the commercially available VR surgical simulators in U.S. ophthalmic residency training programs. Its hardware consists of a model head on an adjustable table with a mechanical eye that is wired to a computer interface and a microscope. This setup allows the surgical trainee to assume a realistic posture. The Eyesi includes cataract surgical instruments and foot pedals. The mechanical eye has a series of holes in it for the trainee’s instruments to enter. Entry into the eye generates a high-fidelity virtual image of the operative eye that is viewable through the microscope. Access can be superior or temporal.
Trainees can practice independently anytime, since the Eyesi is touchscreen activated and users can log in and get started immediately. Trainees can practice the steps in a divide-and-conquer phaco, with the exception of suturing. The latest software update, Eyesi 3.0, adds surgical scenarios including capsulorhexis on a milky-white cataract. The Eyesi platform can also be used with a vitroeretinal package for added flexibility. The Eyesi can play back simulated surgeries, allowing trainees to see what went right—or wrong.
Andrew Hendershot, MD, ophthalmology residency program director and clinical assistant professor of ophthalmology at Ohio State University’s Wexner Medical Center, says that residents there use the Eyesi during all three years of training, most heavily during their second year. “The benefits of the Eyesi are far-reaching,” he says. “Residents learn the foot controls in a no-stress environment, and they can work on posture and hand position. They also learn to work while looking through a microscope.” He adds that the Eyesi allows for focused practice if a resident is struggling with a particular step of surgery. It also enforces the habit of learning incrementally even if a mentor is not present. “The Eyesi has a built-in curriculum that a resident must work through to unlock the next step,” he says.
Use of the Eyesi has been shown in studies to correlate with real-life surgical skills in experienced cataract surgeons,4 and one study5 suggested that training with the Eyesi gave residents who trained on it shorter phaco times and fewer intraoperative complications in the OR.
Dr. Hendershot observes that the skills acquired on the Eyesi carry over into real-life procedures. “In terms of surgery,” he says, “there is proven benefit in lower complications and shorter OR times.”
Anecdotally, Dr. Sikder agrees with Dr. Hendershot that simulators deserve a place in the curriculum. Across a variety of medical and surgical specialties, simulator training has demonstrably increased trainee knowledge and skill, although the effects on patient outcomes are less marked.6
“I like making the analogy between the simulator and exercise equipment,” she says. “If I asked you to hop on a treadmill and do half a mile, and then told you that you were ready for a marathon, you’d probably disagree, even though it’s the same principle of putting one foot in front of the other. Simulators play a role, but in isolation they cannot really prepare you for the actual experience of performing surgery. That’s why it’s critical to have them as one element of a program that includes supervised wet-lab use, independent wet-lab use and review of surgical video. I think the use of simulators in that way is the next step in surgeon education.” REVIEW
Dr. Hendershot disclosed no financial interest in the products discussed in this article. Dr. Sikder has no financial interest, but disclosed her role as an unpaid advisor to ImmersiveTouch.
1. Rowden A, Krishna R. Resident cataract surgery training in United States residency programs. J Cataract Refract Surg 2002:28(12):2202-5.
2. Thomsen AS, Subhi Y, Kiilgaard JF, et al. Update on simulation-based training and assessment inophthalmology: A systematic review. Ophthalmology 2015;122(6):1111-1130.
3. Sikder S, Tuwairqi K, Al-Kahtani E, et al. Surgical simulators in cataract surgery training. Br J Ophthalmol 2014:98:154-148.
4. Thomsen AS, Smith P, Subhi Y, Cour M, et al. High correlation between performance on a virtual-reality simulator and real-life cataract surgery. Acta Ophthalmol 2016 Sep 29. doi: 10.1111/aos.13275. PMID: 27679989. Accessed 2 Feb 2017.
5. Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg 2011:37(10):1756-6.
6. Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: A systematic review and meta-analysis.JAMA 2011:306:978-88.



