|
Clinically, chorioretinal folds appear as alternating yellow and dark bands, most frequently involving the posterior pole.2,3 Angiographically, the appearance of chorioretinal folds is often striking, consisting of alternating bands of hyper- and hypofluorescence. Chorioretinal folds are usually curvilinear and oriented more or less parallel to one another, but may be circular, radial or randomly distributed as well. Patients with chorioretinal folds may be asymptomatic, or they may present with metamorphopsia or hyperopia. Management, when indicated, is dictated by the underlying etiology.
Pathophysiology
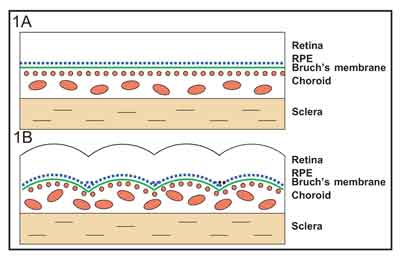
As originally described, and now commonly accepted as the most frequent mechanism at play, any condition that causes relative compression of the inner surface of the sclera may cause the inner choroid, Bruch's membrane, retinal pigment epithelium and neurosensory retina to be thrown into a series of folds. Consequently, any intraocular or extraocular process that alters the normal anatomic relationship of the sclera to the retina may produce chorioretinal folds.2
Historically, however, other mechanisms have been proposed to explain the development of chorioretinal folds. These theories have included choroidal congestion and an anatomic attachment of Bruch's membrane to the underlying choriocapillaris,3 change in the tension of Bruch's membrane with secondary involvement of the RPE,4 and any factor that forces Bruch's membrane to fold.5 Chorioretinal folds have also been attributed to biomechanical properties in the choroid and sclera and their response to compressive stress.6
Clinical, Angiographic Appearance
The folding of the choroid and RPE is responsible for the characteristic appearance seen on clinical examination and fluorescein angiography.2,7 The RPE stretches and becomes relatively thin over the crest or elevated portion of the fold, and, conversely, becomes relatively compressed or compacted at the trough (See Figure 1).2 On clinical examination, the crests of the folds appear yellow or less pigmented, corresponding to the areas of thinned RPE, whereas the troughs appear dark, corresponding to the areas of compressed RPE (See Figure 2A). The overlying retinal folds may have a different contour than the underlying choroidal and RPE folds. On fluorescein angiography, the relatively thin RPE transmits the background choroidal fluorescence better than the compressed RPE, creating a pattern of alternating hyper- and hypofluorescent streaks. The hyperfluorescent bands correspond to the crests of the folds with the thin RPE and the thickened choroid beneath the crests, while the hypofluorescent bands correspond to the dark troughs with the compressed RPE (See Figure 2B).2,7 Fine lines may represent folds confined to the RPE and Bruch's membrane, while broad lines may represent full thickness chorioretinal folds.
|
Causes: "THIN RPE"
Although there are a limited number of causes of chorioretinal folds, they are, for the most part, etiologically unrelated, and so can be challenging to remember. We have, therefore, found the simple mnemonic, "THIN RPE," quite useful. The mnemonic is easy to remember since chorioretinal folds produce "THIN RPE" at the crest of the fold, thereby producing angiographic hyperfluorescence. The causes, each covered in turn below, are as follows:
• Tumors. Choroidal tumors, such as melanoma and metastasis from sites such as breast and lung, may produce chorioretinal folds. Other less common lesions such as melanocytoma, choroidal hemangioma and choroidal osteoma may induce similar findings. These linear or curvilinear folds typically occur at the base of the tumor from mechanical displacement of the choroid, as well as from compression of the choroidal vessels resulting in vascular engorgement, choroidal edema and scleral thickening (See Figure 3).2 Localized suprachoroidal hematomas following intraocular surgery have also been reported to cause chorioretinal folds, and these are typically self-limited.10
|
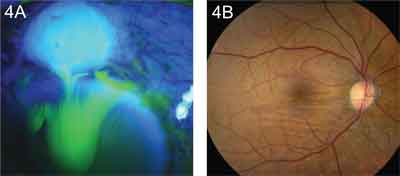
• Inflammation. Thickening and inflammation of the sclera may result in chorioretinal folds. This can occur in posterior scleritis (See Figure 6) and a variety of other disorders. These include orbital inflammatory pseudotumor, thyroid eye disease, autoimmune connective tissue diseases such as rheumatoid arthritis, and vasculitides such as Wegener's granulomatosis and polyarteritis nodosa.2 Patients with scleral inflammation may present with pain, tenderness, proptosis and loss of vision. A thickened posterior sclera may be demonstrated by ultrasound, CT scan or MRI. B-scan ultrasonography is particularly useful in detecting thickening of the choroid and sclera, and edema in Tenon's space, which are characteristic of posterior scleritis (See Figure 6C). The chorioretinal folds often resolve following treatment of the underlying condition.
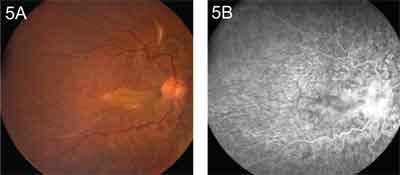
• Idiopathic. When no pathologic condition can be found in association with chorioretinal folds, they are considered to be idiopathic. These patients are often male and present with acquired hyperopia and normal or near normal visual acuity.13 The folds are often bilateral and symmetric, with a variety of patterns depending on location.
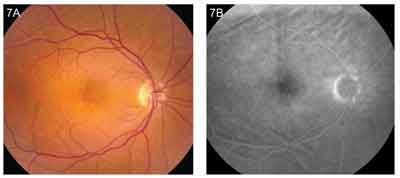
The folds typically radiate from the optic disc, are horizontal in the macula, and are irregularly oblique when located superior or inferior to the posterior pole (See Figure 7). High-resolution CT may demonstrate a flattened posterior pole, thickened sclera, optic nerve enlargement and a space between the optic nerve and its sheath.14 It has been suggested that idiopathic folds may be caused by structural alterations of the sclera that compress the choroidal vasculature, or by an undetected prenatal or childhood inflammatory process that caused scleral shrinkage.2 Some patients with chorioretinal folds may have a constricted scleral canal causing optic disc congestion and a crowded disc, and they may be predisposed to ischemic optic neuropathy, optic disc drusen, papilledema and juxtapapillary choroidal neovascularization.2,15
|
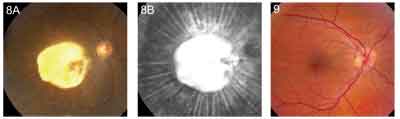
• Neovascular Membrane. A choroidal neovascular membrane associated with age-related macular degeneration may contract spontaneously or following laser photocoagulation, resulting in focal shrinkage of the choroid, thereby producing chorioretinal folds. These folds typically exhibit a radial pattern from the edge of a subpigment epithelial choroidal neovascular membrane. In rare circumstances, the folds may be present prior to other biomicroscopic signs of choroidal neovascularization.16 Disciform scars may produce striking chorioretinal folds (See Figure 8).
• Retrobulbar Mass. Both benign and malignant orbital masses may indent the globe and cause scleral edema and congestion of the choroidal vasculature, resulting in chorioretinal folds. The differential diagnosis of orbital tumors is broad and includes cavernous hemangioma, lymphangioma, hemangiopericytoma, glioma, meningioma, rhabdomyosarcoma, lymphoma, fibrous histiocytoma, epithelial tumors of the lacrimal gland, neuroblastoma, and metastatic tumors.2 Intraconal tumors typically induce hyperopia, while extraconal tumors are often associated with astigmatic refractive errors. Furthermore, intraconal tumors often produce linear chorioretinal folds that radiate from the disc, while extraconal tumors produce curvilinear folds with their convex side directed toward the disc. Chorioretinal folds may be more common in eyes with anteriorly located retrobulbar tumors and in eyes with more severe proptosis.17 The chorioretinal folds typically resolve following treatment or surgical removal of the retrobulbar mass (See Figure 2).
• Papilledema. Increased intracranial pressure from a variety of etiologies including intracranial tumors, pseudotumor cerebri, benign intracranial hypertension and dural arteriovenous malformations can result in papilledema associated with chorioretinal folds. Elevated intracranial pressure may result in increased optic nerve sheath pressure sufficient to obstruct axoplasmic flow.
This may induce optic nerve head swelling and sheath distention, detectable by ultrasound, which may ultimately apply pressure to the globe, causing chorioretinal folds and acquired hyperopia. Rarely, chorioretinal folds precede the disc edema, suggesting that increased sheath pressure may even indent the globe prior to reducing retrolaminar flow.18 Chorioretinal folds associated with papilledema are typically coarse and horizontal in the macula and fine and curvilinear at the nasal side of the optic disc (See Figure 9). In some cases, they may even be circular. The chorioretinal folds may persist after resolution of the papilledema but rarely affect visual acuity.2,18
|
• Extraocular Hardware. A scleral buckle used for the treatment of rhegmatogenous retinal detachment may result in scleral thickening in the vicinity of the buckle, occasionally producing chorioretinal folds near the posterior slope of the buckle.2 Plaque radiotherapy employed in the local treatment of choroidal melanoma, as well as orbital implants used for repair of orbital wall fractures, may also cause chorioretinal folds.
Retinal Folds
 |
They may be concentric around a swollen optic disc, in which case they are referred to as Paton's lines. Retinal folds may radiate from the center of the macula in conditions such as hypotony, scleritis and uveal effusion syndrome with or without chorioretinal folds. Irregular, broad, outer retinal folds are commonly seen in bullous rhegmatogenous retinal detachment, and prominent full-thickness retinal folds may occur after surgical repair of retinal detachment with a scleral buckle or intravitreous gas injection.2 In children, large, full thickness, falciform retinal folds may be seen. These may be congenital or they may occur in association with retinopathy of prematurity, toxocariasis and other conditions.
In conclusion, chorioretinal folds are seen in association with a limited number of etiologies that can be categorized with the mnemonic "THIN RPE:" tumors, hypotony, inflammation/idiopathic, neovascular membrane, retrobulbar mass, papilledema, and extraocular hardware. Chorioretinal folds have a characteristic appearance seen as alternating yellow and dark bands on ophthalmoscopy and as alternating bands of hyper- and hypofluorescence on fluorescein angiography. Patients may be asymptomatic, they may present with acquired hyperopia, or they may complain of metamorphopsia and loss of vision. When the etiology is unknown, imaging should be considered to rule out serious conditions such as tumors and inflammation. Treatment is dictated by cause and often results in resolution of the chorioretinal folds. REVIEW
Dr. Gasperini is a resident in the Department of Ophthalmology at Kresge Eye Institute-Wayne State University. Dr. Eliott is director of clinical affairs and a professor at the Doheny Retina Institute of the University of Southern California, Keck School of Medicine, 1450 San Pablo St., Los Angeles, Calif. 90033. Contact him at (323) 442-6303 or e-mail deliott@doheny.org. All correspondence should be directed to Dr. Eliott. Dr. Cunningham is director of the Uveitis Service at California Pacific Medical Center and a clinical professor at Stanford University School of Medicine, Stanford, Calif. Contact Dr. Cunningham at (650) 238 5014, fax (650) 238 5001, or e-mail emmett_cunningham@yahoo.com.
1. Nettleship E. Peculiar lines in the choroid in a case of post-papillitic atrophy. Trans Ophthalmol Soc UK 1884;4:167-8.
2. Gass JD. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment. Fourth Edition. St. Louis. Mosby, 1997.
3. Newell FW. Choroidal folds. Am J Ophthalmol 1974;75:930-42.
4. Wolter JR. Parallel horizontal choroidal folds secondary to an orbital tumor. Am J Ophthalmol 1997;77:669.
5. Bullock JD, Egbert PR. Experimental choroidal folds. Am J Ophthalmol 1972;75:930.
6. Friberg TR. The etiology of choroidal folds. A biomechanical explanation. Graefe's Arch Clin Exp Ophthalmol 1989;227:459-64.
7. Norton, EWD. A characteristic fluorescein angiographic pattern in choroidal folds. Proc R Soc Med 1969:62:119-28.
8. Atta HR, Byrne SF. The findings of standardized echography for choroidal folds. Arch Ophthalmol 1988;106:1234-41.
9. Haruyama M, Yuzawa M, Kawamura A, Yamazaki C, Matsumoto Y. Indocyanine green angiographic findings of chorioretinal folds. Jpn J Ophthalmol 2001;45:293-300.
10. Augsburger JJ, Coats TD, Lauritzen K. Localized suprachoroidal hematomas. Ophthalmoscopic features, fluorescein angiography, and clinical course. Arch Ophthalmol 1990;108:968-72.
11. Dellaporta A. Fundus changes in postoperative hypotony. Am J Ophthalmol 1955;40:781-785.
12. Kokame GT, de Leon MDL, Tanji T. Serous retinal detachment and cystoid macular edema in hypotony maculopathy. Am J Ophthalmol 2001;131:384-386.
13. Kalina RE, Mills RP. Acquired hyperopia with choroidal folds. Ophthalmology 1980;87:44.
14. Dailey RA, Mills RP, Stimac GK, Shults WT, Kalina RE. The natural history and CT appearance of acquired hyperopia with choroidal folds. Ophthalmology 1986;93:1336-42.
15. Sarraf D, Schwartz SD. Bilateral choroidal folds and optic neuropathy: A variant of the crowded disk syndrome? Ophthalmology 2003;110:1047-1052.
16. Gass JDM. Radial chorioretinal folds: A sign of choroidal neovascularization. Arch Ophthalmol 1981;99:1016.
17. Friberg TR, Grove AS. Choroidal folds and refractive errors associated with orbital tumors. An analysis. Arch Ophthalmol. 1983;101:598-603.
18. Cassidy LM, Sanders MD. Choroidal folds and papilloedema. Br J Ophthalmol 1999;83:1139-1143.