Diagnostic Features
While conjunctivochalasis increases in incidence and magnitude with age,3 its appearance and location can vary. On average, it’s more common to see conjunctivochalasis of the inferotemporal bulbar conjunctiva than inferonasally.4 Many of the symptoms of conjunctivochalasis are similar to the complaints in dry-eye disease, including eye pain, blurred vision, epiphora, dryness and the presence of subconjunctival hemorrhages. If these symptoms worsen in downgaze, it’s more likely that they’re due to the redundant conjunctiva in conjunctivochalasis.4 Another
 |
| Figure 1. Mild conjunctivochalasis seen with normal illumination. It can be difficult to see the folds when they are this mild. However, this patient was still symptomatic with epiphora and no corneal staining. |
In regards to epiphora, conjunctivochalasis is hypothesized to contribute in two ways: First, the reduplicated folds of conjunctiva disrupt the inferior tear lake (Figures 1 and 2) and, second, the conjunctiva itself can cause a mechanical blockage of the inferior punctum.5-6 Blockage of the lower punctum is more common with nasal conjunctivochalasis or with gaze toward the punctum. Dr. Yan Wang and her group at Japan’s Keio
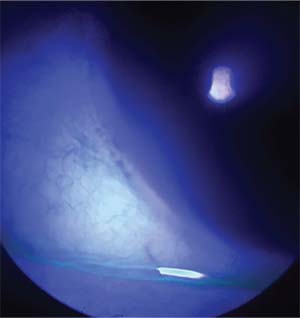 |
| Figure 2. The patient from Figure 1 seen with fluorescein dye and a cobalt blue filter. The conjunctival folds and their obliteration of the tear lake are more easily identifiable. |
Treatment
One of the most frustrating things about treating patients with ocular surface complaints is that they’re chronic and can be refractory to many treatments. Closely examining these patients can allow for targeted treatment that can start the patient in the right direction early on in their disease course. Though not all patients with conjunctivochalasis will have symptoms, a patient who’s complaining of burning, irritated or dry eyes should be examined closely for the presence of conjunctivochalasis. Using the following options, the treatment can be tailored to the patient and his specific pathology, yielding a better chance for success.
Medical Treatment
Before proceeding to surgery, it’s prudent to try to first medically treat the patient’s symptoms. Here’s how to approach the different severities of conjunctivochalasis:
• Mild. If patients are asymptomatic then they can simply be observed. The finding of conjunctivochalasis alone does not warrant treatment.
• Moderate. When patients become symptomatic, the first line of treatment is medical. The goal is to reduce the effects of conjunctivochalasis, especially in regards to the disruption of the tear film. Lubricants tend to be the first-line medications, and while there have not been specific studies looking at different viscosities and their effects, I tend to utilize the gel drop as first-linetreatment for these patients. The rationale for doing this is that the inferior tear meniscus has been obliterated by the multiple folds of conjunctiva and is not providing a supply of tears to be spread during the patient’s blink. Thin tears would continue to be disrupted by the conjunctival folds. However, more viscous drops are able to stay suspended on the surface of the conjunctiva and act in a fashion similar to a tear lake.
• Severe. In severe cases in which the conjunctivochalasis causes the conjunctiva to be exposed even when the eyelids are closed, using artificial tear ointment and patching the eyes at night can be beneficial.8 These patients may also need to use the ointment during the day if they have significant desiccation of the exposed conjunctiva.
In addition to the medical approaches described, any other underlying inflammatory conjunctival conditions should be treated to assist in controlling the patient’s symptoms. This includes treating allergic inflammation with topical antihistamines/mast cell stabilizers, and generally increased inflammation with topical steroids.8 If patients remain symptomatic despite medical treatment, then surgery becomes a reasonable option.
Surgical Treatment
When drugs aren’t enough, it’s time to move on to a surgical solution. Here’s the best way to proceed.
The first step of any surgical procedure is informed consent. However, trying to explain exactly what conjunctivochalasis is to a patient can be challenging. Often, patients think of the conjunctiva as the “white part of the eye.” You may find yourself trying to correct that belief by explaining that it is actually a semitransparent mucous membrane over the sclera, the “true” white part of the eye. Just explaining the anatomy typically requires more time than is available, and when you’re done you still haven’t even discussed the actual disorder or its treatment. To help in this situation, I find that it is easiest to explain to the patient using the analogy that conjunctivochalasis is like loose belly skin. Instead of skin hanging over the belt or the band of the pants, the redundant conjunctiva hangs over the lower lid. Just as there is occasionally the need for a “tummy-tuck,” they’ll understand the analogy to a “conj-tuck.”
There are a number of different techniques that have been described to correct conjunctivochalasis. Some of these are minimally invasive and can be done in the office, while others require a controlled environment, like a procedure room or operating room.
• Cautery approaches. Most of the in-office procedures involve some type of thermally-induced shrinkage or excision to get rid of the redundant folds of conjunctiva clinically visible and resting on the lower lid. One study described using thermocautery as a way to excise the excess conjunctiva at the slit lamp with results showing greater than 90-percent improvement in both subjective and objective findings.9 Their technique involved grasping the redundant conjunctiva with smooth forceps and then excising the grasped portion with a handheld low-temp cautery. There was scarring noted postoperatively in 15 percent of their patients, but it didn’t have any sequelae.
Diana Muñoz, MD, and her colleagues in Bogota, Columbia, describe using a bipolar electrocautery forceps to apply the treatment directly to the symptomatic fold itself, which they identify by positive lissamine green staining. The procedure uses a traction suture through the inferior limbus to rotate the eye superiorly, so this may best be done in a controlled environment. After anesthetizing the area, the stained portion of conjunctiva is elevated and its base is grasped using the bipolar forceps. Energy is applied to the area directly at a rate of 30mA until “complete shrinkage” is achieved. The benefit of this technique is that you target the exact area the symptoms are coming from for that individual patient, whether it is nasal, inferior or temporal. Dr. Muñoz’s group noted that all of their patients had complete resolution of their symptoms without scar development.10
• Argon laser. Argon laser has also been used to “shrink” the redundant conjunctiva. In South Korea, Sangkyung Choi, MD, and his group describe using a 532-nm argon green laser set at 500 µm and ranging in power from 600 to 1200 mW for a duration of 0.5 seconds to treat the inferior conjunctiva. They apply approximately 100 burns during the treatment using “proper shrinkage” as the endpoint for their procedure. Their results showed a statistically significant improvement in the Ocular Surface Disease Index and in tear breakup time, improving from 9.2 seconds to 10.2 seconds. The treatments were more successful in mild and moderate cases.11
• Incisional/glue approaches. In the operating room, the redundant conjunctiva can be removed in a number of ways previously described in the literature, including: simple excision with direct closure;6 injection of fibrin glue subconjunctivally, then pinching and excising;12 as well as a technique in which a limbal peritomy is made with radial relaxing incisions, allowing the loose conjunctiva to be pulled anteriorly and excised with subsequent approximation of the cut edge of conjunctiva to the limbus.13
However, the most highly recommended surgical procedures not only excise the redundant folds of the conjunctiva or tighten it, but also reestablish the fornix. This is because if excision alone is performed, one of the possible complications is scarring leading to foreshortening of the fornix and the possible development of a cicatricial entropion. It’s now believed that, when attempting to improve the function of the tear film, returning the depth of the fornix to its physiologic baseline is as important as removing the redundant conjunctiva. Scheffer Tseng, MD, and his group at Bascom Palmer showed that the tear reservoir in the inferior fornix will rapidly replenish the tear meniscus in normal patients, but that this process is blocked by the additional redundant conjunctiva in the fornix of conjunctivochalasis patients.14 The group showed that repairing this surgically and deepening the inferior fornix reestablishes the normal function of the reservoir and thus provides better resolution of dry eye and ocular surface discomfort symptoms than excision alone.
Dr. Tseng describes being able to normalize the fornix during excision of the conjunctiva by making a crescentic excision of the loose inferior bulbar conjunctiva starting with a peritomy approximately 2 mm posterior to the limbus. He excises all of the loose and thin conjunctival tissue, allowing the remaining conjunctiva to recess into the fornix. The bare scleral defect is then covered with cryopreserved amniotic membrane and anchored using either sutures15 or fibrin glue.16 Glue has become preferred due to less inflammation and better patient comfort. In a retrospective review by Dr. Tseng’s group, there was significant improvement in dry-eye symptoms and clinical findings. An added benefit was that 56 percent of their patients who had a prior diagnosis of aqueous-deficient dry eye, which they termed aqueous tear deficiency, had normalized on their fluorescein clearance testing.17 They hypothesize that the conjunctivochalasis caused so much disruption and blockage in the fornix that it had created an aqueous-deficient state.
Ocular surface discomfort is a common and often frustrating condition for both patients and physicians. It’s important to look at the entire ocular surface to diagnose and appropriately treat a patient’s symptoms. With targeted treatment, there is a much better chance for success. To that effect, don’t overlook the amount that conjunctivochalasis contributes to these symptoms. After trying conservative management with topical medications, if a patient is still symptomatic, then it’s beneficial to take them to the operating room. While all of the surgical procedures discussed here produce great outcomes, I would recommend excision of the redundant and loose conjunctiva with the attempt to reestablish the normal contour of the inferior fornix. By surgically returning the ocular surface to a more normal state, we help to create an environment in which it’s easier for the body to maintain homeostasis. REVIEW
Dr. Bert is a Health Sciences assistant professor at the Doheny and Stein Eye Institutes, David Geffen School of Medicine, UCLA. He has no financial interest in any product mentioned.
1. Hughes WL. Conjunctivochalasis. Am J Ophthalmol 1942;25:48-51.
2. Elschnig A. Beitrag zur aetiologie und therapie der chronischen konjunktivitis. Dtsch Med Wochenschr 1908;34:1133-1155.
3. Gumus K, Pflugfelder SC. Increasing prevalence and severity of conjunctivochalasis with aging detected by anterior segment optical coherence tomography. Am J Ophthalmol 2013;155:2:238-242.
4. Balci O. Clinical characteristics of patients with conjunctivochalasis. Clin Ophthalmol 2014;28;8:1655-60.
5. Liu D. Conjunctivochalasis. A cause of tearing and its management. Ophthal Plast Reconstr Surg 1986;2:1:25-8.
6. Erdogan-Poyraz C, Mocan MC, Irkec M, Orhan M. Delayed tear clearance in patients with conjunctivochalasis is associated with punctal occlusion. Cornea 2007;26:3:290-3.
7. Wang Y, Dogru M, Matsumoto Y, Ward SK, Ayako I, Hu Y, Okada N, Ogawa Y, Shimazaki J, Tsubota K. The impact of nasal conjunctivochalasis on tear functions and ocular surface findings. Am J Ophthalmol 2007;144:6:930-937.
8. Meller D, Tseng SC. Conjunctivochalasis: Literature review and possible pathophysiology. Surv Ophthalmol 1998;43:3:225.
9. Nakasato S, Uemoto R, Mizuki N. Thermocautery for inferior conjunctivochalasis. Cornea 2012;31:5:514-9.
10. Arenas E, Muñoz D. A new surgical approach for the treatment of conjunctivochalasis: Reduction of the conjunctival fold with bipolar electrocautery forceps. Scientific World Journal 2016;2016:6589751.
11. Yang HS, Choi S. New approach for conjunctivochalasis using an argon green laser. Cornea 2013;32:5:574-8.
12. Doss LR, Doss EL, Doss RP. Paste-pinch-cut conjunctivoplasty: Subconjunctival fibrin sealant injection in the repair of conjunctivochalasis. Cornea 2012;31:959–962.
13. Serrano F, Mora LM. Conjunctivochalasis: A surgical technique. Ophthalmic Surg 1989;20:12:883-4.
14. Huang Y, Sheha H, Tseng SC. Conjunctivochalasis interferes with tear flow from fornix to tear meniscus. Ophthalmology 2013;120:8:1681-7.
15. Otaka I, Kyu N. A new surgical technique for management of conjunctivochalasis. Am J Ophthalmol 2000;129:3:385-7.
16. Kheirkhah A, Casas V, Blanco G, Li W, Hayashida Y, Chen YT, Tseng SC. Amniotic membrane transplantation with fibrin glue for conjunctivochalasis. Am J Ophthalmol 2007;144:2:311-3.
17. Cheng AM, Yin HY, Chen R, Tighe S, Sheha H, Zhao D, Casas V, Tseng SC. Restoration of fornix tear reservoir in conjunctivochalasis with fornix reconstruction. Cornea 2016;35:6:736-40.



