In an ideal world, we’d have unscarred conjunctiva to work with every time we perform filtration surgery. Unfortunately, many of us deal with patients who have had prior surgery or, in some cases, have inflammatory issues that have compromised the conjunctival tissue. As a result, in order to perform glaucoma surgery successfully, we have to know how to deal with less-than-virgin, and sometimes frankly scarred, conjunctiva.
How often is a glaucoma surgeon likely to encounter this problem? The
 |
| Assessing conjunctival mobility using a surgical spear during the preop exam. |
The good news is that, thanks to changes in the way cataract surgery is performed, we don’t en-counter this nearly as often as in the past. Years ago, cataract surgery was done extracapsularly with a large corneoscleral incision, or phacoemulsification was done through a scleral tunnel, causing a great deal of conjunctival scarring. Moving cataract surgery to clear cornea has made life much easier for glaucoma surgeons. Today, most of the conjunctival scarring we encounter is the result of glaucoma surgery, although that’s not the only thing that can cause this. Any surgery that manipulates the conjunctiva can lead to scarring. Sometimes conjunctiva can be very scarred without any prior surgery as a result of using topical medications or underlying inflammatory conditions.
When we encounter scarred conjunctiva, any glaucoma surgery we need to perform becomes more challenging and less likely to succeed. To ensure the best possible outcome, we need to do several things:
• First, we need to carefully assess the situation before surgery.
• Second, we need to come up with a plan to work around any obstacles created by the less-than-ideal conjunctiva.
• Third, we need to be prepared to do very meticulous tissue dissection.
• Finally, we need to have several tricks up our sleeve to help us if we find ourselves backed into a corner: We have to know how to make a creative conjunctival flap; we need to be aware of all of the options for working around the problem; and we need to be prepared to use autologous or exogenous grafts.
Assessing the Conjunctiva
When examining the patient, it’s crucial to ask the right questions:
• Has the patient had prior surgeries? This includes any done in childhood: trabeculectomies or tubes; extracap or scleral tunnel cataract surgery; transconjunctival blepharoplasties; pterygium or other excisions; muscle surgery (even as a child, because that will leave areas of conjunctival scarring); and retinal surgery—especially scleral bucking or encircling bands, which can cause 360 degrees of scarring, as well as posterior adhesions behind the muscles.
• If the patient’s previous surgery involved a conjunctival flap, was it limbus- or fornix-based? This is important because the scar lines will be in different places.
• If the patient had previous surgery, was mitomycin-C used? Mitomycin-C can leave the conjunctiva very vascularized and delicate. You could even see mitomycin toxicity, which causes a very avascular, thick, leathery, white, scarred conjunctiva.
• Has the patient used medications that might impact the eye? Prior use of glaucoma medications can greatly affect the quality of the conjunctiva and sometimes cause marked scarring.
• Does the patient have any relevant concomitant conditions? Problems such as pemphigoid, scleroderma, Sjögren’s and chemical injuries can cause conjunctival scarring.
The easiest way to directly assess the condition of the conjunctiva during the preop exam is to anesthetize the eye and use a surgical spear or cotton swab to gently move the conjunctiva over the sclera in all four quadrants, looking for mobility, injection, stiffness and inflammation. Check the limbus, but also check high in the fornix. It’s helpful to draw a map in the chart showing any prior surgical sites, as well as where you find the conjunctiva to be mobile or scarred.
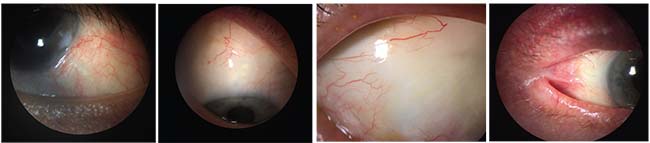 |
| Conjunctival issues a surgeon may encounter during glaucoma surgery include (left to right): Prior glaucoma drainage tube surgery; a prior trabeculectomy with a diffuse filtering bleb; avascular conjunctiva; and conditions such as symblepharon. |
You’ll need to assess the conjunctiva again once you have the patient in the operating room. One of the easiest ways to do that is by injecting fluid under the conjunctiva, which reveals the location of any scar bands. I use mitomycin-C for many of my surgeries, so we dilute it with anesthetic and inject it. It has a therapeutic effect and also helps us to assess where the scar tissue bands are. (I also recheck the condition of the conjunctiva using a surgical spear, as I did during the preoperative exam.)
You should detect most scarring when you’re examining the patient in the office. However, if you discover some scarring in the OR that you missed preoperatively, you may need to alter your planned strategy. If the scarring is very extensive, you may have to consider switching to a different quadrant, or even abandoning trabeculectomy and implanting a glaucoma drainage tube in-stead. A more likely scenario is that you’ll discover one or two bands of scarring that you’ll have to dissect very carefully. Hopefully, this won’t seriously alter your plan.
Of course, it is possible to mobilize even a large area of scarred tissue using very meticulous dissection. However, this can be challenging to accomplish, and even if you succeed the success rate for filtration surgery in that situation decreases dramatically.
Location, Location, Location
When performing glaucoma surgery on an eye with problematic conjunctiva, deciding how to proceed is all about conjunctival real estate. If the patient has had a prior trabeculectomy, can you fit in a second trabeculectomy? Can you implant a tube after a failed trabeculectomy? Can you perform a trabeculectomy after a failed primary tube? Every patient is different, so you have to look carefully to decide what real estate is available to work with.
There are many different scenarios. If you’re considering doing a trabeculectomy, you need to be able to mobilize the conjunctival flap without resistance. For example:
• If you find that mobile con-junctiva is only available inferiorly, trabeculectomy is contraindicated. You’ll have to alter your surgery and consider placing a glaucoma drainage device inferiorly.
• If there’s scarring, but only at the limbus, you can plan a fornix-based conjunctival flap and dissect that scarred conjunctiva off the limbus.
• If the failed surgery was done a little to the temporal or nasal side instead of exactly at 12 o’clock, you can try to fit in another trabeculectomy in the opposite quadrant. However, you want to be very careful about creating a trabeculectomy that’s too nasal or temporal, because that can lead to extension of the bleb into the interpalpebral fissure, which may cause dysesthesia—especially with nasal extension of the bleb.
Other things to consider include:
• If you’re trying to perform a second trabeculectomy, avoid dissecting into the old bleb. You could suddenly get that old surgery working again, and that drainage combined with your new surgery could lead to unexpected hypotony that you might not be able to control.
• Watch out for a scar band that’s high in the fornix. This can happen if the prior trabeculectomy was limbus-based.
• Consider implanting a XEN. When real estate is limited but you have a decent quadrant to work with, a XEN implant might be a good alternative to a trabeculectomy—although the XEN implant is very new, so the decision tree here is still a little unclear. Sometimes it’s hard to mobilize a second trabeculectomy flap; a XEN implant avoids the need for conjunctival and scleral dissection.
The role of the XEN implant is going to grow, especially in those patients that have had surgery in one quadrant and still have an available quadrant. You’ll still need mobile conjunctiva, however, so you don’t want to put the XEN in a quadrant that has significant scarring, and you’ll still need
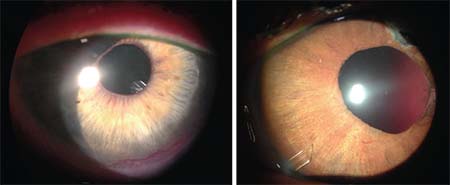 |
| If there’s too much scar tissue superiorly for a trab or tube, consider placing a glaucoma drainage tube inferiorly. Left: tube placed inferiorly in the ciliary sulcus. Right: tube placed inferiorly in the anterior chamber. |
• If you’re dealing with a failed tube, you may be able to do a trabeculectomy, but be aware of the limitations. If the tube was placed pretty far temporally or nasally, you may have enough real estate left to make a good trabeculectomy. However, you need to be sure you can mobilize the flap, and the success rate is going to be lower than it would be with a primary trabeculectomy.
• If there’s too much superior scarring for a trabeculectomy or a tube, place a glaucoma drainage tube inferiorly. However, avoid placing an Ahmed valve inferonasally if the eye is small. The posterior edge of the plate could impinge on the optic nerve.
When Conjunctiva Won’t Reach
When a patient has scarred conjunctiva from a previous surgery, you can sometimes create a good flap with the intention of implanting a drainage tube. However, once you put the tube and plate in, you may sometimes find it hard to get the conjunctiva back to the limbus. When the conjunctiva comes up short, here are a few strategies you can try:
• Remobilize scarred tissue and perform meticulous dissection. Be sure to release the traction suture and rotate the eye back towards the operative quadrant. Then use a blunt cannula or spatula to sweep back deep into the fornix to free the scarred conjunctiva and remobilize the flap; be meticulous in your dissection. Then, use a spear to gently sweep the conjunctiva back towards the limbus.
• If the conjunctiva is very friable and thin, use fibrin glue to secure the flap to the limbus. Sometimes you start passing sutures through the conjunctiva in these patients and you can see that it’s just going to tear the tissue. In this situation, fibrin glue is wonderful; you simply glue the conjunctiva down to the limbus. You still need to anchor the lateral margin to be sure there’s tight closure. Fibrin glue can be a real game-changer in those situations. In fact, I use it on all of my tubes. It’s a great addition to this type of surgery, but it is expensive, and a lot of surgical centers don’t want to have that expense.
• If you’re placing a patch graft over a tube and you can’t get the conjunctiva to reach the limbus, try the “graft and glue” technique. I glue a split-thickness corneal graft in place to cover and lock the tube in position. The nice thing about the glue is that when you put the patch graft on, it’s not just covering the tube; it’s actually sealing it. The whole undersurface of the graft is adherent to the tube and the sclera.
Once you’ve done that, bring the conjunctiva as close as possible, covering as much of the graft as possible, and glue that into position; then anchor it with a few sutures. The tube is protected and sealed under the flap; the conjunctiva will heal over the corneal graft by secondary intention.
Note: When we put Baerveldt implants in, we put venting slits in the tube which must be able to drain. Make those far posteriorly and keep the fibrin glue close to the limbus, away from the venting site.
• To repair a tube erosion, know your options. In this situation you often have a functioning tube, and the intraocular pressure may be under control, so you don’t want to disturb the capsule around the plate. You do want to be able to mobilize the conjunctiva, reposition the tube, and then re-cover everything.
If there’s too much scarring to re-create a conjunctiva flap, you have several options:
— You can try to mobilize conjunctiva from an adjacent quadrant;
— you can cover the exposed tube with amniotic membrane;
— you can cover it with an adjacent or free conjunctival graft;
— you can use a pedicle graft, in which you slide over a pedicle of conjunctiva; or
— you can use the graft-and-glue technique, which works very well for tube erosion.
• Consider other options when repairing a bleb leak. Old trabeculectomies sometimes leak, which increases the risk of blebitis and endophthalmitis. In the past we’ve tried many techniques to manage this that were less than successful, such as autologous blood injections. The mainstay for treating bleb leaks is conjunctival advancement, excising the surface of the old bleb and then remobilizing the flap and bringing it back down to the limbus.
Today I try my best to avoid conjunctival advancement, because there’s a significant failure rate for trabeculectomies when you use this technique. Instead, I’ll leave the bleb intact and try direct suturing, especially when the leak is limbal or in a somewhat vascular area. I may also needle the bleb, to create more diffuse filtration and put less vertical pressure on it. Then I’ll use a mattress suture to either close the leak or wall off the leaking area of the bleb.
• If you need to do conjunctival advancement, excision of the old bleb may be best. If the bleb is small, extremely thin and walled off with a dense scar band, excision of the old bleb and conjunctival advancement may be your best option. If you need to do conjunctival advancement, dissect posteriorly as far as possible.
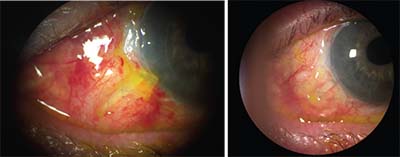 |
| Left: A corneal graft glued over a tube to seal the tube to the sclera, with the conjunctiva glued to cover the edges of the graft, one day postop. Right: The same eye 10 days later with conjunctiva healed over the graft by secondary intention. |
• Try releasing conjunctiva by making an incision up by the fornix. If you can’t relieve the traction with simple dissection, make a horizontal incision up in the fornix, allowing the conjunctival tissue to be pulled toward the location at which it’s needed. You can suture it at the limbus and then suture the posterior aspect as well. Don’t worry about the exposed sclera deep in the fornix; it will heal by secondary intention.
Other options for managing a shortage of tissue include mobilizing conjunctiva from an adjacent quad-rant; a Z-plasty or conjunctival rotational graft; using a conjunctiva free graft; or using amniotic membrane. (Peter A. Netland, MD, PhD, who has written about this topic, says he prefers using an autologous patch graft, or free graft, that’s oversized by at least 1 mm, taken from an area away from the location of the bleb.)1
What if you can’t do any of these things? Such cases should be rare, but if they happen, you may have no option except to abandon ship. If that becomes necessary, close the flap, cover it with a donor graft, let things heal over and then plan for a tube in another quadrant.
Going In with Eyes Open
Conjunctival scarring or deficiencies are never fun to manage, but in the vast majority of cases one of these techniques will save the day. Just remember to:
• Be prepared; know what you’re getting into. Do a very thorough pre-operative assessment and have a clear plan in mind.
• Reassess your plan in the OR.
• Perform meticulous dissection of scarred tissue.
• Know how to make a creative conjunctival flap and what your other options are.
• Be prepared to use autologous or exogenous grafts.
• Remember that fibrin glue is your BFF (Best Friend Forever!). REVIEW
Dr. Piltz-Seymour is an adjunct professor at the Perelman School of Medicine at the University of Pennsylvania, and director of the Glaucoma Care Center at Valley Eye Professionals in Huntingdon Valley. She has no financial ties to any products mentioned.
1. Lawrence SD, Netland PA. Inadequate conjunctival coverage. In: Feldman RM, Bell NP, eds. Complications of Glaucoma Surgery. New York, NY: Oxford University Press, 2013, pp. 258-264.



