Nevertheless, placing drops on the eye is still the method of delivery almost every patient uses, and that old-school technology is likely to remain in use for the foreseeable future. That brings us back to a basic, well-known problem: Many patients have difficulty using eye drops properly.
Faced with a dismal rate of accurate drop use among patients, most doctors focus on trying to teach patients better eye drop application technique or try to get someone else to help the patient instill the drops. However, there are some clever, readily available low-tech eye drop application devices that may do a lot to help your patients succeed in getting their drops onto their eyes. These devices fall primarily into three categories: those that attempt to position the bottle over the eye in a consistent manner while holding the eyelids open; those that use surface tension to deliver a drop onto the eye via an intermediary device; and one or two that offer unique approaches to getting the drops onto the eye. Here, we’ll provide a review of some of the products in each category.
Bottle Managers
The first category is the simplest: The eye dropper bottle is snapped into, or otherwise
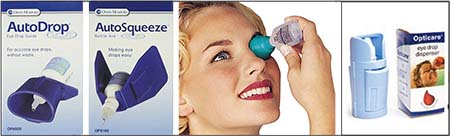 |
| Some products claim to help position the bottle over the eye and make it easier to squeeze. |
Products in this category (see pictures, below) include:
• AutoDrop Eye Drop Guide. The tip of the dropper bottle clips into the lid of this guide, which the manufacturer says was developed in collaboration with the British Royal National Institute for the Blind. The guide, which holds the eye open with the bottle positioned over the eye, has a pinhole that lets light in; according to the manufacturer, when the patient looks at the pinhole, the eye is correctly positioned to receive the drop. This device can be used in conjunction with AutoSqueeze, another plastic device that goes around the bottle itself (rather than clipping onto the tip); it uses the lever principle to make it easier to squeeze the bottle. You can find more information about both items at: maddak.com/autodrop-eye-drop-guide-p-28115.html.
• Flents Ezy Drop Guide & Eye Wash Cup. This plastic bottle holder resembles an eye-wash cup, and the manufacturer claims it can be used for that purpose as well. You can check it out at amazon.com/Flents-Drop-Guide-0-058-Pound/dp/B0011YK3NS.
• Opticare Eye Drop Dispenser. In addition to positioning the bottle over the eye, this device is designed to make it easier for the patient to squeeze the bottle. The manufacturer claims that it essentially makes a small bottle as easy to manage as a larger bottle. For more information, visit guldenophthalmics.com/products/index.php/opticare-eye-drop-dispenser.html.
Using Capillary Action
A less intuitive but more interesting approach to getting drops onto the eye involves placing a single drop into a
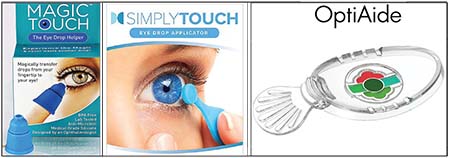 |
| Several products use capillary action to make the drop “jump” from the device onto the eye. |
• Magic Touch: The Eye Drop Helper. This device, which resembles a small rubber bell about the size of a thimble, is placed on a fingertip; with the finger held vertically, a drop is placed into a small dimple at the tip of the device. The patient then leans forward, and when the device gets close to the eye, the drop “jumps” onto the eye. Designed by Julius Shulman, MD, the Magic Touch device is BPA-free and made of medical-grade silicone. The manufacturer says that antimicrobial silver ions in the material eliminate up to 99.99 percent of microbes, so the device can be kept clean by simply rinsing under warm water after use. You can find more information at magic-touch-eye.myshopify.com.
• SimplyTouch. This device is a small, reusable handheld applicator with a tiny disc at the top, onto which a drop is placed; surface tension keeps the drop in place. One side of the disc has no rim; the other has a rim to help less viscous drops stay on the disc. The patient places a drop onto the plastic applicator, pulls down the lower lid while looking in a mirror, brings the tip of the applicator close to the eye, and the drop jumps onto the eye. Advertised features include that the device can be used with or without glasses on, and that the device is easy to clean and store after use. Because it’s easier for the patient to control the drop usage, the manufacturer claims that patients get up to 50 percent more uses per bottle. You can learn more at simplytouchusa.com.
• OptiAide. This device, which looks more high-tech than the others, can hold up to five drops in its five chambers. (In the product photo, each chamber has been filled with different food coloring to make them easier to see.) Unlike the other devices, this one is held in front of the eye, allowing the drop to jump onto the eye, theoretically preventing the device from contacting the cornea. However, it does require moving the eyelids and lashes out of the way. You can find more information at contactlenskit.com/optiaide/.
A Targeted Approach
One of the most unique dropper-assist designs was created by Jonathan Cress, MD, an ophthalmologist in Santa Cruz, Calif., who’s been in practice for more than 40 years. “The Cress dropper is an arched tube that screws onto the dropper bottle,” he explains. “It references the nose so the tip can be comfortably and steadily placed in the medial canthal area. Once the tip is properly placed, the bottle is squeezed; the drop leaves the aperture, slides down and off the little ramp onto the delivery tip and into the eye. (See photos, facing page.) The patient releases the bottle when she feels the drop. The current version of the dropper has no metering component, but most patients learn to adjust their bottle squeeze to release just one drop.”
Asked about keeping the drops sterile, Dr. Cress notes that the delivery tip is designed to physically isolate the distal aperture from the delivery surface. “The purpose of this design is to prevent conjunctival or skin bacteria from being aspirated back into the bottle, contaminating the drops,” he says. “Cleaning the tip after each use would be ideal, but it’s not
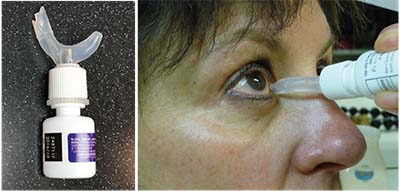 |
| The Cress Dropper allows a drop to slide into the eye. |
Dr. Cress says that patients who use the dropper are almost universally happy with it. “I have a substantial population of patients who can’t get drops in their own eyes with a standard dropper,” he says. “Those patients have to have their spouse or someone else instill their drops. With my dropper, most of them can do it themselves. However, some patients who lack manual dexterity or have weak hands still may find it difficult or impossible to meter a drop by squeezing accurately. They still waste drops and occasionally miss, so they’re less happy with it.”
Dr. Cress says he’s observed a difference in outcomes when glaucoma patients switch to his device, although he doesn’t have concrete data to prove it. “I’ve had patients who seemed to be failing at drop therapy, but after using this device, their intraocular pressure stabilizes and their visual field loss ceases,” he says. “To me, this indicates that they weren’t effectively instilling drops before, but with the dropper they are. Additionally, patients using the dropper rarely run out before a refill is due.”
Dr. Cress says he originally created the device for his 9-year-old son who was suffering from dry eye. “Once I had a working model I licensed it to Wilson Ophthalmic, who made about 20,000 of them,” he says. “I’m currently working on improvements to the design. The next version accurately meters a single drop, is easier to squeeze and makes it easier to get the drop into the eye. I’m open to proposals for manufacturing the new model.” For more information about the original version, visit amazon.com/Cress-Dropper-EyeDrops-Professional-Model/dp/B004R8TOGM. REVIEW



