|
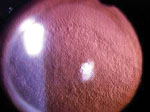
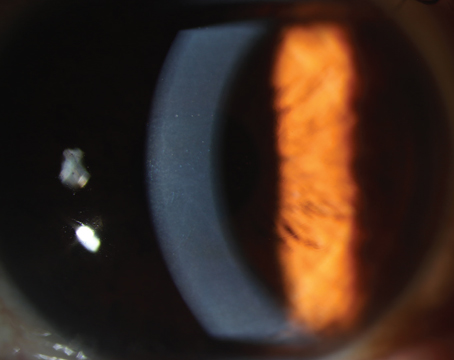
The mechanism of potential visual compromise is really twofold: the thickness of the cornea and the optical reflectivity of the endothelium. Those two characteristics don’t necessarily correlate. Many years ago, we would perform hard contact lens corneal endothelial stress tests and place a hard lens on the cornea. We measured serial pachymetry before and after the contact lens and the recovery time required for the cornea to return to its pre-contact lens thickness. We don’t perform this provocative test much anymore, yet we desperately need better physiologic analyses of the ability of the patient’s endothelium to perform adequately after the trauma of even the very best cataract surgery.
Additionally, we have to make a decision about every patient we see who has endothelial abnormalities and whether or not he or she will be able to tolerate routine cataract surgery without a severe postoperative corneal deturgescence deficit. This requires a lot of handholding and informed consent with patients. Fortunately, in my practice, we follow patients with Fuchs’ dystrophy for years and have established a rapport with our patients so they already accept and understand that there may be a bumpy road after they have their cataract surgery done in their 60s, 70s or 80s.
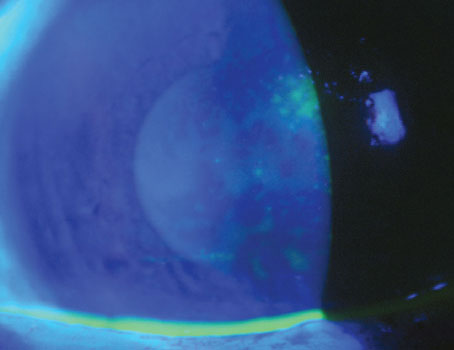
DSEK
With the advent of the Descemet stripping endothelial keratoplasty pro-cedure, our threshold for performing cataract surgery on a patient with Fuchs’ dystrophy is much lower: We can now frequently recommend a cataract operation for patients with non-decompensating Fuchs’ dystrophy at the same stage of visual function compromise as we would any patient with a normal cornea. A recent study has found that the quality of vision is severely impaired in patients with Fuchs’ dystrophy and improves significantly after DSEK.1 The study included 99 eyes with Fuchs’ dystrophy that were evaluated in the Netherlands and 48 eyes with Fuchs’ dystrophy that were evaluated at the Mayo Clinic. The study found that eyes with Fuchs’ dystrophy had decreased corrected distance visual acuity and increased straylight compared with normal eyes. Corrected distance visual acuity and straylight were correlated with corneal thickness. Corrected distance visual acuity and straylight improved at all postoperative examinations, and improvement in straylight from preoperatively to 12 months postoperatively was correlated with patient age.
| ||||
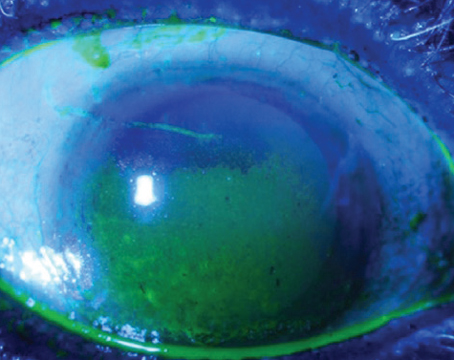
In all but the most severely pigmented endothelium, it is generally possible to consider cataract surgery alone, especially because we have adapted such efficient procedures now that really minimize phaco energy and minimize the amount of balanced salt solution that goes through the eye. I offer to all of my patients, unless there are obvious corneal folds present, the possibility of sequential surgery, hoping that the patient will not immediately or ever require the DSEK transplant procedure. This has been a very successful strategy.
Rarely, a patient with such horrible corneal edema presents that, despite maximal medical therapy, the cornea is simply not clear enough for a safe cataract operation. Then, the surgeon has two choices: Just do an old-fashioned triple procedure with a full-thickness transplant and cataract extraction and lens implant, or first perform the DSEK procedure, allow it to heal and then perform the cataract operation. The latter is certainly a viable alternative but not the preferred alternative for patients who must minimize the number of operations performed due to general health or personal reasons.
Most of the time, however, the patient has a pretty decent endothelium, specular counts somewhere between 500 and 1200/mm2 and pachymetry between 580 µm and 650 µm, and our goal is to minimize corneal edema postoperatively. If the endothelial reflectivity, however, is such that the patient is disturbed regardless and was disturbed by the reflectivity before the cataract formed, then we would elect to do a DSEK triple procedure, with the DSEK and the cataract removal and the IOL implantation at the same time, remembering of course that we need to be able to see through the cornea prior to the DSEK to do the cataract surgery. It is also possible to perform the DSEK procedure first and then the cataract operation.
Personally, I much prefer sequential surgery because first, both procedures seem to do better when performed alone. Second, it is less stressful for the patient. Third, they don’t want to get the transplant unless they really have to, and you don’t really know how each patient will fare until you actually perform the cataract surgery. Fourth, reimbursement is simpler and fairer for sequential surgery. And fifth, sequential is technically safer and easier. We can get better pupillary constriction when the IOL has been in place for a number of months and the patient is not dilated from the cataract operation. Furthermore, with the IOL capsule unit fully formed through adhesions with the haptics and the bag, we see a much more stable anterior chamber, less difficulty with vitreous pressure and negligible IOL prolapse when performing the sequential DSEK surgery.
|
I find that Viscoat has the best adhesive qualities to the endothelium even to the extent of using a larger vial or a separate vial that really genuinely protects the endothelium in adequate quantity. In fact, a recent study conducted in Greece found that Viscoat is safer and more protective for the corneal endothelium than Visthesia during uneventful phacoemulsification cataract surgery.2
I use Viscoat before the capsulorhexis as well as before the phacoemulsification after the hydrodissection has been performed. That second application is probably the key step. The next most important step is to use as little flow as possible and to minimize the amount of BSS that circulates and regurgitates through the eye. This is done with low-flow techniques and a careful phacoemulsification in the bag or iris plane if at all possible. I find that the OZil on our Infiniti markedly reduces the amount of phaco energy required.
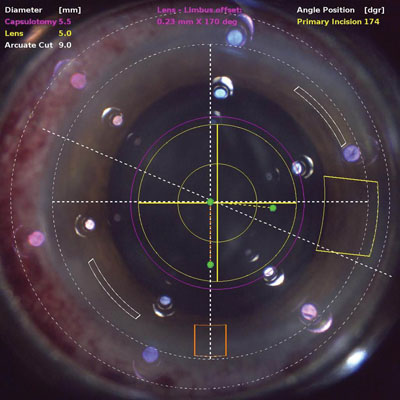
Femtosecond Cataract Surgery
Finally, the new frontier in the minimization of trauma to the corneal endothelium at the time of cataract surgery is utilizing femtosecond lasers for cataract surgery. The advantages of the femtosecond laser are many. It performs the capsulorhexis, which minimizes surgery time for the doctor. The capsulorhexis is perfectly centered so, in theory, we have the best possible access to the cortex. Finally, and most importantly, a great deal of the fractionation and division of the nucleus has already taken place with the femtosecond laser when the actual surgery begins.
I have found that I’m able to reduce the total cumulative phaco energy by about 50 percent when I switch to femtosecond laser surgery. Reducing that phaco energy is very important. Other strategies that may be beneficial are using BSS Plus in the irrigating solution. Also, chilling the solution may reduce metabolic damage to the endothelium. Intensive preoperative topical administration of steroids reduces the inflammatory potential of the endothelium by downregulating the inflammatory cascade prior to and after the surgery. Additionally, intensive steroids also minimize inflammatory damage to the endothelium.
An outstanding approach to minimizing endothelial damage is using some of the newer steroids available. First of all, I can treat the patient overnight with preservative-free Lotemax ointment. It is very potent and well-tolerated by the patient and provides a preservative-free night-long application of steroid for the patient. Remember that patients with Fuchs’ dystrophy are most edematous in the morning. The hypertonicity of the gel provides an excellent preparation overnight to minimize the period of time the cornea remains edematous.
Another welcome new addition to our pharmaceutical approach is difluprednate (Durezol), which provides a very intensive pharmaceutical anti-inflammatory effect on the cornea due to its unique preparation and doubly fluorinated steroid biochemistry. Difluprednate emulsion has demonstrated exceptional protection against corneal thickening following cataract surgery.3
So, we have many new tools to use in providing the patient with mild to moderate Fuchs’ dystrophy with the very best chance for an excellent result in cataract surgery without a corneal transplant. It’s faster, less stressful, less expensive, less disruptive of lifestyle or employment activities and promises fewer potential complications for the patient than having either sequential surgery or a triple procedure with a DSEK. REVIEW
Dr. Sheppard is president of Virginia Eye Consultants and a professor of ophthalmology, microbiology & molecular biology at Eastern Virginia Medical School in Norfolk, Va.
1. Van der Meulen IJ, Patel SV, Lapid-Gortzak R, Nieuwendaal CP, McLaren JW, van den Berg TJ. Quality of vision in patients with Fuch’s endothelial dystrophy and after Descemet stripping endothelial keratoplasty. Arch Ophthalmol 2011;129:1537-1542.
2. Moschos MM, Chatziralli IP, Sergentanis TN. Viscoat versus Visthesia during phacoemulsification cataract surgery: Corneal and foveal changes. BMC Ophthalmol 2011;11:9.
3. Donnenfeld ED, Holland EJ, Solomon KD, et al. A multicenter randomized controlled fellow eye trial of pulse-dosed difluprednate 0.05% versus prednisolone acetate 1% in cataract surgery. Am J Ophthalmol. 2011;152(4):609-617.