 |
As a busy cataract and refractive surgeon, I examine a large number of general ophthalmology patients. Over a short period of time at the end of 2010, I examined four extremely interesting patients, which will hopefully be instructive and heighten your own diagnostic skills. I received late night phone calls from radiologists on all four patients!
 |
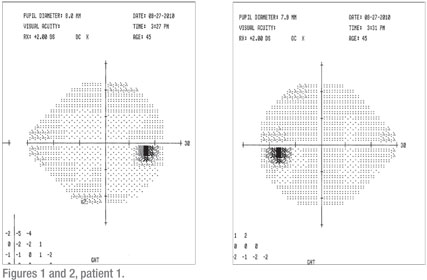
DC is a healthy 45-year-old man who was referred by a local optometrist with a chief complaint of “loss of peripheral vision in the left eye” for the previous few days. Past medical history was not contributory. No other neurological complaints were offered. Uncorrected distance vision was 20/20 in each eye. Color vision was full OU. Motility and pupils were normal. Intraocular pressures were normal. Slit lamp and dilated retinal exam with 90-D and indirect ophthalmoscopy were normal. Formal visual field testing (24-2) was unremarkable and normal statistically (See Figures 1 and 2).
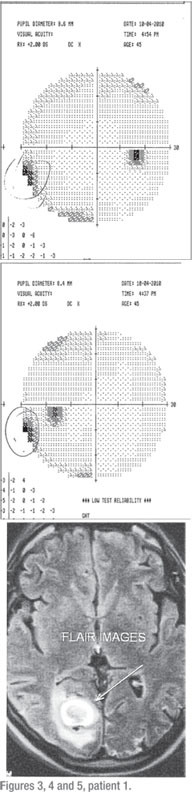
Because of the complaints and the normal exam, I had him return one week later for a repeat evaluation. Everything was unchanged. His complaint was consistent that there was a loss of peripheral vision in his left eye. He demonstrated that there was a missing spot in the very outer aspect of his left eye. The dilated exam was unchanged. Repeat visual field testing, this time with a 30-2, revealed a very small, but significant, left, inferior homonymous defect (See Figures 3 and 4).
An MRI of the head with and without gadolinium revealed “a 27-mm hemorrhagic mass lesion in the right occipital lobe” associated with edema and a mass effect (See Figure 5). The differential diagnosis was an astrocytoma, AVM and cavernous hemangioma. After repeated evaluations and MRIs by the neurosurgeon, the lesion was diagnosed as a cavernous malformation.
There are some critical diagnostic issues in this case. First, patients commonly complain of vision changes, especially peripherally. Even after reviewing the abnormal visual field, the patient still denied any complaints in his right eye. Clearly, if the visual complaint can be elicited in both eyes, the neurological significance is completely different than if the complaint is unilateral.
The initial “unilateral” nature of his complaint made an optic nerve or retinal problem seemingly very likely. However, patients often ignore any visual field defect that is nasal, which is why it is so imperative to be vigilant about making sure that the visual fields are normal in both eyes. It is extremely common for patients, as well as ER doctors and internists, to mistakenly confuse a visual field cut in both eyes with loss of vision in one eye.
I recently had a patient with known age-related macular degeneration call me from out of town in a panic complaining of sudden loss of vision in one eye. It turned out she had suffered an occipital lobe stroke with an obvious and severe vertical field cut bilaterally.
Secondly, having patients return for a repeat exam within a few days is helpful. Patients appreciate our concern. If the complaint persists or worsens, further testing should be done or a referral to a specialist should be made.
Finally, the 30-2 visual field should have been ordered initially. I routinely do 24-2 visual field testing on glaucoma and glaucoma suspects. A 30-2 is obviously better for detecting neurological deficits.
Patient 2
UB is a healthy 31-year-old man who had a chief complaint of “my right eye has lost quite a bit of clarity in the past few months.” Past medical history was not contributory. He had no neurological complaints. Best-corrected vision OD was counting fingers, and OS was 20/20 with minimal myopic astigmatism. Pupils were equal and reactive to light and accommodation. There was a 1-2+ afferent papillary defect OD with a subjective APD of “75 cents.” Motility was normal. IOPs were normal, as was the slit-lamp exam.
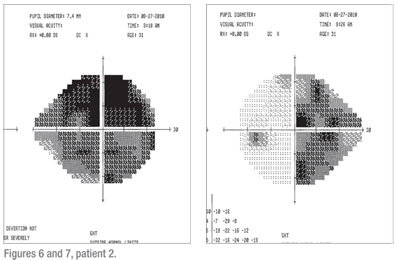
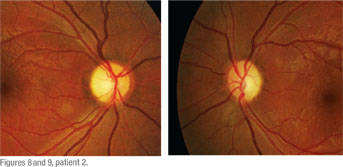
Visual field testing revealed complete and total depression OD. There was a dense vertical cut OS nasally (See Figures 6 and 7). Dilated fundus exam revealed optic nerve pallor OU, but worse OD than OS (See Figures 8 and 9). Color vision was 0/15 correct OD and 4/15 correct OS. An MRI of the brain and orbits with gadolinium revealed a large, 3 x 3 x 3 cm macroadenoma with the suprasellar component severely compromising the first portion of the optic nerves, the right greater than the left as well as the optic chiasm and proximal optic tracts (See Figure 10). It turned out to be a prolactinoma.
The severe loss of vision in a relatively short period of time is most concerning. It is doubtful that this degree of vision loss and optic nerve pallor occurred in “the past few months.”
Regardless of whether the patient was a poor observer, in denial or had been to another doctor who missed the problem, it is truly disheartening given his young age, irreversible changes, and completely curable disease if caught in a timely manner.
Patient 3
RG is a 77-year-old, generally healthy man with a history of chronic sinusitis. He presents with a few-hour history of vertical, binocular diplopia, pain and a droopy left upper eyelid. His VA is excellent OU. Pupils were equal and reactive to light and accommodation. No APD was noted. Extraocular movements were normal. He had a small-angle esotropia with a slight left hypertropia. He was mildly proptotic OS with a mildly ptotic left upper lid. There was moderate chemosis of the bulbar conjunctiva on the left. IOPs were normal. No optic nerve swelling or vascular congestion was noted.
Because of the complaints and the normal exam, I had him return one week later for a repeat evaluation. Everything was unchanged. His complaint was consistent that there was a loss of peripheral vision in his left eye. He demonstrated that there was a missing spot in the very outer aspect of his left eye. The dilated exam was unchanged. Repeat visual field testing, this time with a 30-2, revealed a very small, but significant, left, inferior homonymous defect (See Figures 3 and 4).
An MRI of the head with and without gadolinium revealed “a 27-mm hemorrhagic mass lesion in the right occipital lobe” associated with edema and a mass effect (See Figure 5). The differential diagnosis was an astrocytoma, AVM and cavernous hemangioma. After repeated evaluations and MRIs by the neurosurgeon, the lesion was diagnosed as a cavernous malformation.
There are some critical diagnostic issues in this case. First, patients commonly complain of vision changes, especially peripherally. Even after reviewing the abnormal visual field, the patient still denied any complaints in his right eye. Clearly, if the visual complaint can be elicited in both eyes, the neurological significance is completely different than if the complaint is unilateral.
The initial “unilateral” nature of his complaint made an optic nerve or retinal problem seemingly very likely. However, patients often ignore any visual field defect that is nasal, which is why it is so imperative to be vigilant about making sure that the visual fields are normal in both eyes. It is extremely common for patients, as well as ER doctors and internists, to mistakenly confuse a visual field cut in both eyes with loss of vision in one eye.
I recently had a patient with known age-related macular degeneration call me from out of town in a panic complaining of sudden loss of vision in one eye. It turned out she had suffered an occipital lobe stroke with an obvious and severe vertical field cut bilaterally.
Secondly, having patients return for a repeat exam within a few days is helpful. Patients appreciate our concern. If the complaint persists or worsens, further testing should be done or a referral to a specialist should be made.
Finally, the 30-2 visual field should have been ordered initially. I routinely do 24-2 visual field testing on glaucoma and glaucoma suspects. A 30-2 is obviously better for detecting neurological deficits.
 |
UB is a healthy 31-year-old man who had a chief complaint of “my right eye has lost quite a bit of clarity in the past few months.” Past medical history was not contributory. He had no neurological complaints. Best-corrected vision OD was counting fingers, and OS was 20/20 with minimal myopic astigmatism. Pupils were equal and reactive to light and accommodation. There was a 1-2+ afferent papillary defect OD with a subjective APD of “75 cents.” Motility was normal. IOPs were normal, as was the slit-lamp exam.
Visual field testing revealed complete and total depression OD. There was a dense vertical cut OS nasally (See Figures 6 and 7). Dilated fundus exam revealed optic nerve pallor OU, but worse OD than OS (See Figures 8 and 9). Color vision was 0/15 correct OD and 4/15 correct OS. An MRI of the brain and orbits with gadolinium revealed a large, 3 x 3 x 3 cm macroadenoma with the suprasellar component severely compromising the first portion of the optic nerves, the right greater than the left as well as the optic chiasm and proximal optic tracts (See Figure 10). It turned out to be a prolactinoma.
 |
 |
Pituitary adenomas are very prevalent,being found in almost 15 percent of autopsies and 22 percent of radiological studies. Classically, the visual field defect is bitemporal because the nasal retina fibers (providing temporal peripheral vision) crossing through the chiasm are the ones typically compressed by the pituitary tumor. In this patient however, there was a nasal defect OS. This is most commonly due to involvement with the optic tract or optic nerve. Furthermore, acute bleeding within the pituitary can cause this type of visual field defect.
 |
RG is a 77-year-old, generally healthy man with a history of chronic sinusitis. He presents with a few-hour history of vertical, binocular diplopia, pain and a droopy left upper eyelid. His VA is excellent OU. Pupils were equal and reactive to light and accommodation. No APD was noted. Extraocular movements were normal. He had a small-angle esotropia with a slight left hypertropia. He was mildly proptotic OS with a mildly ptotic left upper lid. There was moderate chemosis of the bulbar conjunctiva on the left. IOPs were normal. No optic nerve swelling or vascular congestion was noted.
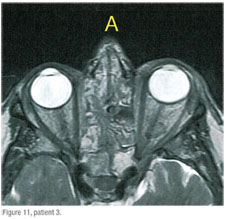
An MRI of the brain and orbits with gadolinium showed extensive panparanasal sinus disease with secondary orbital inflammation on the left, preseptal swelling, and proptosis (See Figure 11).The patient was started on prednisone and antibiotics orally by our practice’s oculoplastics specialist and subsequently improved immediately.
The rapid onset of ptosis, diplopia, pain and chemosis certainly indicated a serious orbital process and the need for urgent neuroimaging.
The differential diagnosis is broad and includes infectious (orbital cellulitis), idiopathic (pseudotumor), immune-mediated (thyroid-related orbitopathy, systemic vasculitis), and neoplastic causes. Working closely with internists, head and neck surgeons, and neurosurgeons in these cases is critical.
 |
The rapid onset of ptosis, diplopia, pain and chemosis certainly indicated a serious orbital process and the need for urgent neuroimaging.
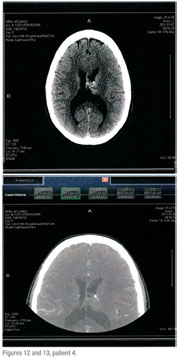 |
KP is a very healthy 43-year-old woman who underwent bilateral cataract surgery as a child and then secondary intraocular lenses six years ago. She presents with a one-week history of a painless, droopy left upper lid. Her best spectacle-corrected visual acuity was unchanged. Pupils were irregular from prior surgery. No APD was noted. She had about 4 mm of ptosis with normal levator function. There appeared to be some lid retraction on the right. No proptosis was noted. Motility exam was normal. Slit-lamp and dilated exam were normal. Because of the recent onset of the ptosis, inability to evaluate the pupils adequately, and the possibility of thyroid-related orbitopathy, an MRI of the head and orbits, with and without contrast was obtained. It showed a 3.1 x 2.4 x 2.1-cm cystic mass in the left lateral ventricle, which is probably a central neurocytoma (See Figures 12 and 13). The mass in the ventricle was apparently incidental and not causative of the ptosis. Interestingly, the ptosis resolved soon thereafter.
Dr. Elkins is in private practice at Ophthalmology Associates of the Valley in Encino, Calif. Contact him at strybr@aol.com.




