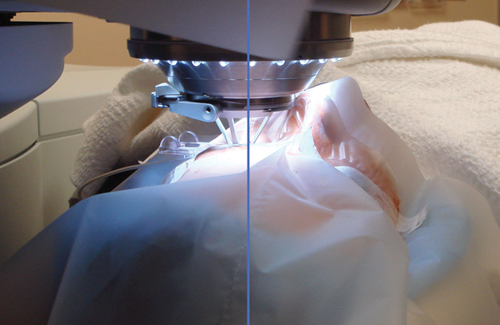
While surgeons agree that LASIK flaps created with femtosecond lasers have intraoperative and postoperative advantages over flaps created with microkeratomes, the exact size and shape of the optimal femtosecond flap is still being studied.
“Five years ago, I hung up my microkeratomes and never looked back,” says Steven E. Wilson, MD, professor of ophthalmology and staff cornea and refractive surgeon at the Cole Eye Institute of the Cleveland Clinic. “I can’t imagine making flaps any other way now. Femtosecond flaps are so much more precise, and there is less risk of anything seriously complicated happening as can occasionally happen with a microkeratome.”
Some of the specifics still being worked out include the optimal side-cut angle, flap size, flap shape and flap thickness.
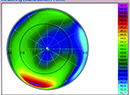
Side-cut Angle
According to Los Angeles surgeon Uday Devgan, MD, all side cuts were previously made at 90 degrees. “If you look at a manhole cover, it is a disc with edges at 90 degrees,” says Dr. Devgan. “With the new femtosecond lasers, you can change that side cut to be more or less than that. Some people make it a little bit less than 90 degrees so that when the flap comes down, it kind of locks into place. One advantage of femtosecond flaps is that you can have an edge cut of variable geometry.”
Daniel Durrie, MD, in private practice with Durrie Vision in Overland Park, Kan., uses a 120-degree, inverted side cut. “I do think an inverted side cut is an advantage,” Dr. Durrie says. “With this type of flap, the edge is tucked underneath, and there is less of a gutter. The flaps seem to fit better. Theoretically, that would avoid flap slips and edge wrinkles and may provide stronger adhesion.”
He notes that these flaps also look better cosmetically. “When you look at patients who have had an inverted side cut, you can barely tell that they have had anything done to their eyes,” he says.
Chicago-based surgeon Mitchell Jackson, MD, notes that the inverted side cut also induces less dry eye than other types of cuts. “There is improved severed nerve apposition and less reduction in corneal sensitivity with a 140-degree inverted side-cut versus a 30-degree side-cut femto flap. This results in less dry eye,” he explains.
|
Another topic up for debate is the perfect flap size. Dr. Devgan notes that some patients, such as a postop cataract patient in need of LASIK to enhance his or her vision, do not need a 9-mm flap. “A lot of times, these patients have smaller pupils, and we are doing very small corrections of 1 D or less. We could even make a 7.5-mm flap. There is a large difference in the surface area of the flap with a small change in the diameter,” he says.
Dr. Wilson, on the other hand, prefers very large-diameter flaps. “I don’t see much dry eye with a 9-mm to 9.3-mm flap,” he says. “Some people are trying smaller flaps, 8-mm to 8.5-mm, and the problem is that those have to be perfectly centered or the patient can get visual distortions, especially with night vision. I don’t see the utility in making those smaller-diameter flaps. My usual patient is a 9.3, and then I will reduce it if he or she has a smaller-diameter cornea, but I never go less than 9 mm.”
San Diego surgeon Steven Schallhorn, MD, also uses larger flaps. “The thought behind using smaller flaps is to reduce the chance of dry eye: The smaller the flap, within reason, the better,” he explains. “I don’t personally agree with that logic for several reasons. One is that I don’t think it makes a difference in postop dry eye. Also, a small flap has to be perfectly well-centered. If it’s not, the flap may not cover the ablation optical zone and could result in induced aberrations and quality-of-vision problems.”
He believes that the ideal flap should be the same diameter as the full excimer treatment, including the transition zone. “For instance, many femtosecond lasers, such as the Intralase and the FS200, flat applanate the cornea,” says Dr. Schallhorn. “An anticipated 7-mm ‘flap diameter’ actually ends up being an arc length of 7 mm. Once the cornea rebounds to its original curvature at the conclusion of the procedure, the true flap diameter will be less than 7 mm and will be dependent on the steepness of the cornea. The chord length of the exposed stromal bed is what is important for the excimer ablation treatment, not the arc length. Those are some of the problems with the concept that a smaller flap is always better.”
Dr. Durrie recently conducted a study to evaluate the safety, efficacy, and patient satisfaction with regard to signs and symptoms of dry eye in patients undergoing bilateral LASIK procedures with two flap sizes. The study included 30 patients and was presented at the 2011 annual meeting of the American Academy of Ophthalmology. (Brinton JP, et al. Does flap size matter? A contralateral evaluation of safety, efficacy, and dry eye symptoms after bilateral LASIK with two flap sizes. Scientific Poster 471.) Flaps in both eyes were created with the Intralase 150-kHz femtosecond laser. One randomly selected eye in each patient had an 8.0-mm round corneal flap, and the other eye had a 9.0-mm round corneal flap.
At one month after surgery, there was no statistical difference in the uncorrected visual acuity, best-corrected visual acuity, tear breakup time or Schirmer results. There was also no difference in the patients’ symptoms. “This is one of the real values of a contralateral study,” he says.
Dr. Durrie notes that there was a mild, transient increase in dry-eye symptoms both objectively and subjectively at one month, but the symptoms returned to normal baseline at three months. At six months, subjectively, the symptoms were better than they were preoperatively. “The notion that LASIK causes dry eyes may need a further look because this study, which was well-controlled, really showed that LASIK did not induce any more than a temporary one-month dry eye. It also showed, and this is with femtosecond high-quality flaps and modern excimer lasers, that it didn’t cause halo or glare either,” he adds.
Shape
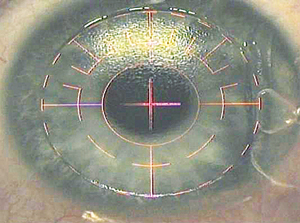
Because the shape of the cornea is slightly oval, the femtosecond laser’s ability to create an oval flap may be an additional advantage. “You can make an oval flap and increase the diameter in one meridian and have it smaller in the other meridian,” Dr. Schallhorn says. “The idea is to optimize the flap so it is just the right size, including the hinge.
The hinge would be located at the major axis of the ellipse. You can have almost an ideal-shaped flap for the excimer laser treatment profile by making this oval flap.”
|
Thickness
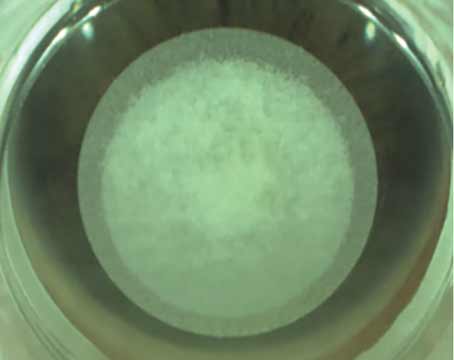
Surgeons are also trying to determine the perfect flap thickness. Dr. Schallhorn points out that the trend used to be toward thinner, sub 100-µm, flaps, but that trend may be reversing. “Many surgeons are choosing flap thicknesses between 100 µm and 120 µm. Most surgeons are not going thinner than 100 µm,” he explains.
A recent study conducted in India found no differences in predictability and clinical outcomes when comparing four flap thicknesses.1 The study included 240 eyes with four thicknesses of 60-kHz laser-assisted LASIK flaps: 90 µm, 100 µm, 110 µm and 120 µm. Postoperative vision and refractive outcomes were similar in the four groups. The study found that the predictability and planarity were satisfactory in all four groups; however, the indices were slightly better in the 110-µm and 120-µm groups.
Dr. Wilson notes that there is some variability in flap thickness, albeit smaller than with the microkeratome, even with the femtosecond laser. When a surgeon aims for 90-µm or 80-µm flaps, some are going to approach the epithelial thickness, and wound healing will be more like PRK than LASIK, including some corneas developing late haze due to basement membrane damage.
Dr. Schallhorn also notes that femtosecond flaps have encouraged surgeons to return to LASIK. “Eight years ago, with mechanical keratomes, there was a movement away from LASIK and toward surface ablation. With the femtosecond laser, there has been a gradual return to LASIK,” he says.
One of the many reasons for that is the improved postoperative stability of the flap with the femtosecond laser. Dr. Schallhorn and his colleagues recently published a study that found that the risk of early flap displacement was higher after microkeratome surgery than after femtosecond laser surgery.2
The study included 81,238 eyes, of which 14,555 were hyperopic and 66,681 were myopic or mixed astigmatic. A total of 57,241 eyes were treated with the Intralase FS-60 femtosecond laser, and 23,997 were treated with the Moria SA ONE Use-Plus automated microkeratome.
Ten eyes (eight hyperopic eyes and two myopic eyes) experienced flap displacements. All displacements occurred within 48 hours of surgery, and none were preceded by ocular trauma. The incidence of early flap displacement was 0.033 percent (eight eyes) after microkeratome surgery and 0.003 percent (two eyes) after femtosecond laser surgery.
The Future
While LASIK-designed femtosecond lasers are only being used in the United States to create LASIK flaps, they are currently being used in Europe for other procedures, as well. For example, European surgeons are already performing femtosecond lenticule extraction (FLEx), which basically corrects vision with only a femtosecond laser. No excimer laser is required. This procedure entails making a flap and then using the same femtosecond laser to carve out a small lenticule.
|
Another procedure is small-incision lenticule extraction (SMILE). “Instead of making the large corneal flap and then taking the lenticule out, surgeons just make a tiny 4-mm incision, go in with forceps, and pull the lenticule out. There is no flap at all,” Dr. Devgan explains.
A recently published study has found that this technique is safe, predictable and effective for treating myopia and myopic astigmatism.4 The study included 51 eyes of 41 patients. The VisuMax femtosecond laser system was used to perform SMILE to treat refractive errors. The laser was used to cut a refractive lenticule intrastromally. The lenticule was then extracted from the stroma through a 3.0-mm to 5.0-mm incision. Patients’ mean spherical equivalent was -4.87 D ±2.16 (SD) preoperatively and +0.03 ±0.30 D six months postoperatively. Refractive stability was achieved within one month. Six months postoperatively, 79 percent of all full-correction cases had an uncorrected distance visual acuity of 20/25 or better. The six-month postoperative corrected distance visual acuity was the same as or better than the preoperative corrected distance visual acuity in 95 percent of eyes.
“Perhaps, the future direction of laser vision correction will be purely femtosecond laser. Excimer lasers may not be needed,” Dr. Devgan says. REVIEW
1. Prakash G, Agarwal A, Yadav A, et al. A prospective randomized comparison of four femtosecond LASIK flap thicknesses. J Refract Surg 2010;26(6):392-402.
2. Blum M, Kunert KS, Engelbrecht C, Dawcynski J, Sekundo W. [Femtosecond lenticule extraction (FLEx)—Results after 12 months in myopic astigmatism]. Klin Monbl Augenheilkd 2010;227(12):961-965.
3. Clare G, Moore TC, Grills C, Leccisotti A, Moore JE, Schallhorn S. Early flap displacement after LASIK. Ophthalmology 2011;118:1760-1765.
4. Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: All-in-one femtosecond laser refractive surgery. J Cataract Refract Surg 2011;37:127-137.