Keratoconus and ectasia have been successfully treated with both Intacs and corneal collagen cross-linking. For example, a recent study conducted in China showed long-term stability of post-LASIK corneal ectasia after cross-linking without any relevant side effects.1 The study concluded that cross-linking seems to be a safe and promising procedure to stop the progression of keratectasia, therefore avoiding or delaying keratoplasty.
The study included 20 eyes of 11 patients who underwent LASIK for myopic astigmatism and subsequently developed keratectasia. Cross-linking appeared to stabilize or partially reverse the progression of post-LASIK corneal ectasia. Improvements in uncorrected and best-corrected visual acuity were statistically significant 12 months after the procedure.
Similarly, in Iran, researchers found Intacs to be a safe and effective treatment option for patients who have keratoconus, clear central cornea and contact lens intolerance. In this study, 37 eyes of 36 patients with moderate to severe keratoconus, clear central cornea and contact lens intolerance underwent Intacs placement. Postoperative examinations demonstrated a clinically significant improvement in both uncorrected distance visual acuity and best-corrected distance visual acuity. Both had a continuous improvement throughout the follow-up period.2
“It’s all about access currently,” says Mitchell A. Jackson, MD, founder and director of Jacksoneye, in Lake Villa, Ill. According to Dr. Jackson Intacs are approved in the United States on an investigative device exemption. Surgeons must have IRB approval, which can be obtained through a central IRB associated with Addition Technology Inc. “Cross-linking is not FDA-approved yet,” he said. “You have to be in your own IRB-approved study or part of another larger study. [He cites a current clinical trial sponsored by Avedro looking at safety and efficacy of corneal collagen cross-linking in eyes with keratoconus.] If you’re not, you won’t have access to collagen cross-linking, but you can have access to Intacs immediately if you have a femto laser or if you have the prolate technology.”
 |
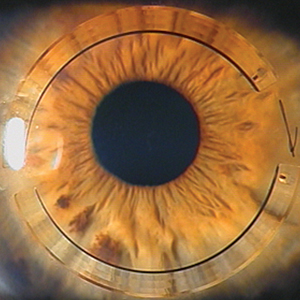
| Figure 1. Left to right, one-year postop and difference map after combined Intacs and corneal collegen cross-linking using asymmetric Intacs segments. |
Two Treatments, Two Goals
Intacs and cross-linking have two different primary goals, according to Peter S. Hersh, MD, of the Cornea and Laser Eye Institute–Hersh Vision Group, in Teaneck, NJ. “The goal of Intacs is to support the cornea with the ring segments in order to both flatten the cone, and almost more importantly, to make the corneal contour more symmetric—the ultimate goal there being to improve the patient’s spectacle-corrected vision as well as to give a better corneal contour for contact lens fitting,” says Dr. Hersh. “The goal of corneal collagen cross-linking is different. It is not so much to affect the corneal topography, but to strengthen the cornea in order to prevent progression of the disease over time. In theory, these are complementary interventions—the Intacs to improve the corneal shape and contour and the cross-linking to diminish progression of disease.”
Dr. Hersh and his colleagues are currently conducting a clinical study examining the combination of Intacs and collagen cross-linking. The goal of the study is to assess the safety and efficacy of doing the procedures in combination and to see if timing affects the outcome. In other words, is it better to combine the two procedures together, or is it better to do the Intacs first and do the cross-linking later on?
The study is ongoing, but the researchers have done a preliminary analysis of the results. Their latest report included 74 eyes, and these were stratified to concurrent treatments and consecutive treatments. “The bottom lines here were twofold: The two can be used successfully together, and they do not seem to have any ill effects upon one another, so doing both procedures on the keratoconic eye appears to be appropriate,” says Dr. Hersh. “Second, the results are preliminary, so we don’t have a final analysis, but our preliminary results show that there were no statistically significant differences between the two treatment groups at one year. For instance, the maximum flattening in the combination group was 5.84 D, and the maximum flattening in the Intacs first and cross-linking second group was 5.34 D. Most patients were stable, and we saw no difference in keratoconic progression between the two groups.”
|
According to Dr. Hersh, there is a clear role for Intacs in selected patients with or without cross-linking because the rings have an effect and goal different than cross-linking. “We have found with cross-linking alone an average improvement in keratometry readings,” he says. “You do get flattening on average, 1.7-D flattening in our previously reported study. You do get a little bit of spectacle-corrected vision improvement of about one line on average. The topographic improvement that you get with the addition of the Intacs is substantial, upwards of 5 D, as I mentioned, depending on the size and configuration of the Intacs segments. You need to look at these two procedures as having a different goal and attacking the keratoconus from two different but complementary directions. One is physically re-shaping the cornea with the insertion of the ring. The other is biomechanically restructuring the cornea and stabilizing it with secondary optical effects, but predominantly with the goal of stabilization of the ectatic disease process.”
He adds that one of the things he has learned from his general work and also from the study is that the use of asymmetric Intacs, with the larger Intacs segment beneath the cone and the smaller Intacs segment above, or the use of a single segment below the cone may be more efficacious in making the corneal topography more symmetric than symmetric Intacs segments. “In most patients where we have asymmetry of the cone, where the cone is not centered and where the patient has a substantial amount of astigmatism, which most patients with noncentered cones have, the use of asymmetric Intacs or a single inferior segment can be indicated,” says Dr. Hersh. “A year or so ago, the larger Intacs segments were approved to 400- and 450-µm segments. In addition, they have a 210-µm segment. Using a bigger segment, one can get more robust results, and using the larger one below and the smaller one above can give you a more profound effect to make the cornea more symmetric afterwards.”
In another study he is doing, he has had very good success with contact lens fitting after the dual approach. He has looked at 33 patients with Intacs and cross-linking, and he has found a very high success rate (more than 90 percent) in fitting either with a hybrid lens or a mini-scleral contact lens. “Undergoing these interventions seems to prepare the cornea to achieve good contact lens fit, comfort, and visual result. Patients on average improved to 20/28. That was our final contact lens-corrected visual acuity, which is remarkable in these patients,” he adds.
Majid Moshirfar, MD, notes that questions remain regarding which procedure should be done first. “For mild keratoconus, especially if a patient is young, I will do collagen cross-linking,” he says. “On the other hand, if the patient is middle-aged and has moderate keratoconus, I will most likely place the Intacs first. Some surgeons are creating the channels for the Intacs with the femtosecond laser or their mechanical system, and then they inject the riboflavin into the channels and then they put the rings in simultaneously,” says Dr. Moshirfar, a professor of ophthalmology at the John A. Moran Eye Center in Salt Lake City, Utah.
A study conducted in Turkey has found that combined Intacs placement and corneal collagen cross-linking treatment with intracorneal riboflavin injection was effective in keratoconic eyes.3 The study concluded that “intracorneal riboflavin injection into the tunnel was safe and may provide more penetration without epithelial removal.”
This study included 131 eyes in 105 patients with a mean follow-up of 7.07 months. The mean improvement was 0.26 ±0.16 logMAR in uncorrected distance visual acuity and 0.24 ±0.16 logMAR in corrected distance visual acuity.
According to Dr. Moshirfar, combining corneal collagen cross-linking and PRK is also an option. “There are many patients who come to our office who really don’t need to get Intacs,” he says. “They have forme fruste keratoconus. They have a very mild pattern of irregularity. They have excellent visual acuity with glasses or contact lenses. They are interested in refractive surgery, and we tell them they cannot get refractive surgery. Many of these patients end up getting collagen cross-linking with secondary PRK.”
A recent study conducted in Canada found that the combination of Intacs placement followed by sequential same-day PRK and collagen cross-linking may be a reasonable option for improving visual acuity in some patients with keratoconus.4 The study included five eyes in four patients. All eyes first underwent laser-enabled placement of Intacs, followed by same-day PRK and collagen cross-linking. Six months after the procedures, significant improvements were seen with regard to uncorrected and corrected distance visual acuity, spherical equivalent refraction, keratometry and total aberrations. None of the patients lost lines of corrected distance visual acuity or developed haze.
The Future
Dr. Jackson notes that, in the near future, studies sponsored by Avedro will involve collagen cross-linking at the time of LASIK (LASIK Extra), which is using cross-linking under the LASIK flap to “freeze” the cornea to prevent ectasia and prevent regression of effect, especially in hyperopia.
A recent study conducted in Turkey found that LASIK with accelerated cross-linking appears to be promising to prevent corneal ectasia after LASIK.5 Four patients between the ages of 22 and 39 years underwent LASIK with concurrent accelerated cross-linking in one eye and LASIK alone in the fellow eye to treat myopia or myopic astigmatism. At the one-year follow-up, the group that underwent the combined treatment had an uncorrected distance visual acuity and manifest refraction equal to or better than those in the LASIK-only group. Endothelial cell loss in the combination group was not greater than in the LASIK-only group. REVIEW
1. Li G, Fan ZJ, Peng XJ. Corneal collagen crosslinking for corneal ectasia of post-LASIK: One-year results. Int J Ophthalmol 2012;5(2):190-195.
2. Niknam S, Shamshiri M, Shahrzad SS, Alipour A, Rajabi MB, Rajabi MT. Treatment of moderate to severe keratoconus with 6-mm Intacs SK. Int J Ophthalmol 2012;5(4):513-516.
3. Kilic A, Kamburoglu G, Akinci A. Riboflavin injection into the corneal channel for combined collagen crosslinking and intrastromal corneal ring segment implantation. J Cataract Refract Surg 2012;38:878-883.
4. Iovieno A, Legare MI, Rootman DB, Yeung SN, Kim P, Rootman DS. Intracorneal ring segments implantation followed by same-day photorefractive keratectomy and corneal collagen cross-linking in keratoconus. J Refract Surg 2011;27(12):915-918.
5. Celik HU, Alagoz N, Yildirim Y, et al. Accelerated corneal crosslinking concurrent with laser in situ keratomileusis. J Cataract Refract Surg 2012;38:1424-1431.