Differentiating between allergic conjunctivitis and dry-eye syndrome can be a challenging task. Patients may complain of non-specific symptoms like eye redness and irritation, and catching clinical clues can be difficult if patients are poor historians or can't recall the situations in which their symptoms are most prominent. To make matters worse, some patients may have both conditions.
In this article, we'll discuss the clinical tools that are available for diagnosing each of these conditions and how best to treat them. We'll then present a couple of case examples.
Diagnosing Allergic Conjunctivitis
Allergic disorders of the ocular surface include seasonal and perennial allergic conjunctivitis, vernal keratoconjunctivitis, atopic keratoconjunctivitis and drug-induced dermatoconjunctivitis.
It's estimated that ocular allergies affect one-fifth of the general population. Seasonal allergic conjunctivitis and perennial allergic conjunctivitis are the most common, prevalent in over 90 percent of allergic disorders.1 AKC and VKC are more severe ocular allergies, often having corneal involvement. Drug-induced allergies tend to affect the area where the drug is instilled (mainly the lower lids) and will normally clear up once the patient stops using the offending agent. We'll focus here on identifying the more common SAC and PAC.
The ocular allergic reaction is an IgE-dependent hypersensitivity response. In susceptible individuals, initial exposure of allergen to the ocular surface stimulates the production of allergen-specific immunologic antibodies (IgE), which bind to mast cells in the conjunctiva. The mast cell is a granulocyte containing a number of preformed mediators, primarily histamines. Once activated, newly formed chemical mediators such as prostaglandin D2, leukotrienes and platelet aggregating factor are synthesized. Exposure of allergen to the IgE-coated mast cells leads to the release of pre- and newly formed mediators contained within the mast cell.2
|
Most patients with ocular allergies will be asymptomatic during their office visits. The clinician must inquire about environmental triggers such as animal dander, trees, pollen, grass, ragweed, dust and molds. Many patients will forget their allergies in the off-season months. Only careful questioning may reveal that every spring their eyes bother them, or their symptoms are heightened when they mow the lawn or visit their cat-owning relative. They may reveal that their eyes only bother them when they go camping or spend more time outside. Some patients may take medications during allergy season, but won't report them when asked if they take any drugs. Occasionally, chart review will reveal that every May the patient visits the office. These are important clues. The month or season that the patient experiences symptoms is important. The intensity and frequency of the symptoms can help differentiate allergic conjunctivitis from dry eye.
Allergy skin testing can often reveal whether or not a patient is allergic to a variety of things. However, it's important to note that these tests don't always correlate with site-specific testing (i.e., measuring levels of tear IgE).5 In addition, skin testing may fail to reveal the allergen which provokes the allergic conjunctivitis. Also, patients with allergic conjunctivitis symptoms and a positive skin test for a specific allergen may not have a positive conjunctival allergen challenge to that antigen. Thus, a combination of testing and questioning is necessary.
An intense itch differentiates ocular allergies from the burning, stinging and foreign body sensation associated with dry eye. If a patient experiences intense itching and redness while outdoors, suspect seasonal ocular allergies. Depending on the time of year, there may be high pollen counts for a specific antigen. For example, in the northeastern United States, March is commonly tree pollen season, May is grass season and mid-August through mid-September is ragweed season. As another example, Sacramento has a particularly high incidence of panseasonal allergies.
Perennial ocular allergens such as dust, pet hair/dander and mold can present a constant aggravation. If a patient experiences intense itching, redness, and discomfort while indoors, and during times of the year inconsistent with seasonal allergens, then perennial ocular allergies may be involved. One study of allergens in homes found that the dust collected from nearly all of the houses sampled contained pet allergens, even though less than half of the homes had pets.6 Thus, it's difficult to avoid allergens.
Treating Allergic Conjunctivitis
Although total avoidance of environmental allergens is nearly impossible, patients can still find relief by reducing their exposure. For instance, staying inside on days with high pollen counts can help decrease symptom severity. However, in most cases, use of ocular allergic medications is warranted. There are a variety of available products, but the most effective for treating a topical disease such as allergic conjunctivitis are topical ocular treatments that are effective against all signs and symptoms.
Topical treatment of ocular allergies has proven superior to systemic treatment as it ensures direct delivery to the tissue. Additionally, topical treatment avoids the drying effects that have been shown to result from use of certain systemic antihistamines.7 Ocular drying is counterproductive for the treatment of ocular allergies since a healthy, functioning tear film is vital for flushing away allergens.
Over-the-counter antihistamines or antihistamine/vasoconstrictor combinations offer quick onset, but short duration of action. Most are indicated for q.i.d. dosing, but the dose duration is only two to four hours. This regimen, therefore, cannot always provide all-day coverage for ocular allergic signs and symptoms.
The more potent prescription agents with antihistamine and mast-cell stabilizing activity provide the most effective treatment for ocular allergies. This class of dual-action agents includes Patanol (Alcon), Zaditor (Novartis), Elestat (Inspire/ Allergan) and Optivar (MedPointe). These products have comfortable formulations, rapid onset and long duration of action (dosed b.i.d.). Patanol is the only eyedrop within this category that is indicated for the full range of ocular allergic signs and symptoms.
Diagnosing Dry Eye
|
One of the most troubling aspects of dry eye is that symptoms don't always correlate with signs. Patients may complain bitterly of burning and stinging yet have very little staining. Other patients may have severe staining yet only mildly complain of photophobia or have no symptoms at all. Researchers have discovered that dry eye progressively reduces corneal sensitivity, which may account for these findings.10 Therefore, diminishing discomfort scores can be correlated with an increase in ocular-surface disease. This can make identification and treatment of dry eye a monumental task.
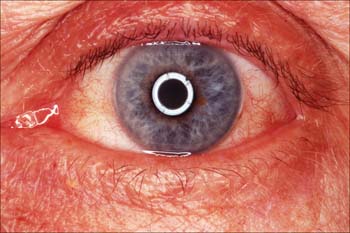
Patients with dry eye present with dryness, burning, stinging, grittiness, foreign body sensation, blurred vision and photophobia. It's important to distinguish between foreign body sensation (dry eye) and itch (allergy) by asking about the intensity and frequency of the symptoms. Tearing is another symptom that needs to be specifically elicited because most people don't associate it with dry eye. However, many dry-eye subjects will experience reflex tearing as a result of environmental stimuli, such as wind.
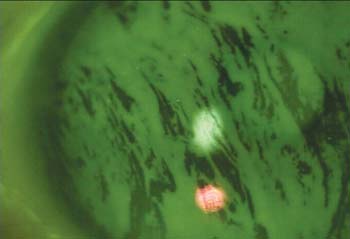
Dyes can aid in the diagnosis of dry eye by identifying dry areas of the conjunctiva and cornea. Fluorescein is known to identify disruptions between corneal epithelium and conjunctival epithelium at intercellular junctions (dry, dead cells). Lissamine green is an alternative dye that is good for identifying degenerated cells and mucus. In studies, typically only 5 µl of fluorescein or 10 µl of lissamine is instilled. This administration of micro-quantities of dye is important to eliminate the oversaturation of the epithelium, making it easier to distinguish between actual staining and quenching. Time to fluorescence can vary from patient to patient, depending on tear volume and tear turnover rate, but may take two to five minutes. Barrier filters such as Wratten #12 or Tiffen #11 under 16X magnification can help highlight staining.11 A tear-film breakup time shorter than five seconds (with 5 µl of fluorescein) is indicative of dry eye.12 Dye can also be instilled using fluorescein or lissamine green strips.
Blinking is crucial for maintaining the integrity of the tear film. Some of the factors that can influence blink rate are environmental (e.g., humidity, temperature, airflow and lighting), activity-related (e.g., computer use, reading and driving), psychological (e.g., emotional state and mental load) and physiological (e.g., gender, ocular surface conditions, corneal sensitivity and muscular tension).
Although researchers have developed a precise method for measuring blink rate that uses a digital camera and infrared illuminator to track pupil diameter (Casavant J, et al. IOVS 2004;45: ARVO E-abstract 77)
, there are other ways to measure blink rate in the office. Blinks can be simply counted while a patient is reading the eye chart. Dividing the number of blinks per minute into 60 seconds gives the inter-blink interval (IBI).
|
The Ocular Protection Index, which measures the relationship between TFBUT and IBI, has recently been developed as an accurate and reproducible tool for diagnosing dry eye. The OPI is calculated by dividing TFBUT by the IBI. If the OPI is less than 1, a patient's cornea is at risk for environmental exposure, since the tear film is breaking up before the patient is blinking. If the OPI is 1 or more, a patient's cornea has reduced risk because the patient is blinking before the tear film breaks up. The OPI is also a useful tool for evaluating dry-eye treatments.(Ousler GW, et al. IOVS 2002;43:ARVO E-abstract 56)
Treating Dry Eye
Dry-eye treatment usually begins with increased education and a trial of artificial tears. Once patients learn about dry eye, they can begin to modify their behavior to avoid aggravating factors such as environmental stimuli or prolonged visual tasking.
Aside from education and modification of behavior, most patients can benefit from artificial-tear therapy. There are a number of available artificial tears, each with a different mechanism of action. Some examples include Soothe (Alimera), GenTeal (Novartis), Systane (Alcon) and the Refresh products such as Refresh Tears, Liquigel and Endura (Allergan).
Soothe and Refresh Endura are emulsions that work by enhancing the lipid layer of the tear film. GenTeal, Refresh Tears and Refresh Liquigel increase the viscosity of the aqueous portion of the tear film and help prevent evaporation. Systane works through a pH-dependent polymerization of HP-guar, creating a gelatinous consistency, which covers and protects the ocular surface. After a period of frequent artificial tear use with no relief, punctal plugs may be inserted to help retain tears. However, punctal plugs usually reduce the quality of tears by preventing tear turnover. At this point, it may be wise to turn to a prescription dry-eye medication.
Restasis (Allergan) is the only approved medication for increasing tear production due to ocular inflammation associated with dry eye, and is recommended for patients with more severe dry eye. Research has demonstrated that an artificial tear used in conjunction with Restasis, such as Systane, is a compatible and effective treatment.13 This is especially important during the period of time before the true benefits of Restasis kick in, which may be up to six months. There are also numerous products currently in clinical trials, which may prove to be beneficial treatments.
Clinical Examples
Case #1
• History: A 60-year-old male in Sacramento, Calif., has glaucoma, and has been taking Alphagan (brimonidine, an alpha-2 agonist) twice a day for three months. He presents with red and itchy eyes. Upon further questioning, he reveals that he has nasal congestion at the same time every year.
• Exam: His eyelids are non-injected and non-edematous. The conjunctiva is non-injected and there are no follicles. Mild chemosis is present. His intraocular pressure is 16 mmHg OU.
• Diagnosis: This patient likely has seasonal allergies, unrelated to his glaucoma medication. Drug-induced dermatoconjunctivitis is less likely, as there is no evidence of lid involvement. Typically, in drug-induced allergies, the lower lid becomes excoriated and red. There is often redness in the inferior aspect on the bulbar conjunctiva. Drug-induced allergic reactions will progress relentlessly. Inferior palpebral follicles are also commonly seen in allergies to brimonidine, but are absent in this patient. He should continue using Alphagan. The seasonality of his complaints is a clue that he has allergic conjunctivitis.
• Treatment: A topical antihistamine/mast-cell stabilizer.
Case #2
• History: A 55-year-old woman has itchy and burning eyes. She lives in New Hampshire, and it is mid-winter. She has a cat and has been taking oral antihistamines. Her mouth is dry.
• Exam: Her lids appear normal. Her tear meniscus height is slightly reduced at 0.1 mm and fluorescein staining shows a pattern in the palpebral conjunctiva.
• Diagnosis: Burning is highly likely to be dry eye, exacerbated by oral antihistamine use, which causes oral and ocular drying. An allergy to cat fur or dander is probably inducing itching in the eye.
• Treatment: She should frequently use a tear substitute, drink plenty of water and try to be conscious of her blink rate. She can use a humidifier for the dry eye. She should stop the oral antihistamines and use a topical antihistamine/mast-cell stabilizer and a nasal steroid for itching and nasal congestion. Restrict the cat to certain rooms and keep the house ventilated if weather permits.
• Comments: Due to her decreased tear volume from dry eye, this woman is more likely to react to antigens, which are causing the itching. She should benefit from treating both conditions. Also, she should be re-evaluated for dry eye once she stops taking the oral antihistamine.
Dr. Torkildsen is in private practice with Andover Eye Associates, serves as a principal investigator for numerous studies and consults in ophthalmic pharmaceuticals. Ms. Plumer is medical communications manager and Mr. Workman is a clinical research associate at Ophthalmic Research Associates in North Andover.
1. Abelson MB, Chapin MJ. Current and future topical treatments for ocular allergy. Comp Ophthalmol Update 2000;1:303-317.
2. Abelson MB, Smith L, Chapin M. Ocular Allergic Disease: Mechanisms, Disease Sub-types, Treatment. The Ocular Surface 2003;1:3:127-149.
3. Abelson MB, Allansmith MR. Histamine in the eye. In: Silverstein A, O'Connor G, eds. Immunology and Immunopathology of the Eye. New York: Masson Publishing, 1979:362-364.
4. Abelson MB, Udell IJ. H2-receptors in the human ocular surface. Arch Ophthalmol 1981;99:302-422.
5. Leonardi A, Battista MC, Gismondi M, et al. Antigen sensitivity evaluated by tear-specific and serum-specific IgE, skin tests, and conjunctival and nasal provocation tests in patients with ocular allergic disease. Eye 1993;7(Pt 3):461-4.
6. Arbes SJ, Cohn RD, Yin M, Muilenberg ML, Friedman W, Zeldin DC. Dog allergen (Can f 1) and cat allergen (Fel d 1) in US homes: Results from the National Survey of Lead and Allergens in Housing. J Allergy Clin Immunol 2004;114:1:111-7.
7. Ousler GW, Wilcox KA, Gupta G, Abelson MB. An evaluation of the ocular drying effects of 2 systemic antihistamines: Loratadine and cetirizine hydrochloride. Annals of Allergy, Asthma and Immunology 2004;93:460-464.
8. Brewitt H, Sistani F. Dry eye disease: the scale of the problem. Surv Ophthalmol 2001;45:199-201.
9. Baudouin C. The pathology of dry eye. Surv Ophthalmol. 2001;45:2:S211-20.
10. Xu KP, Yagi Y, Tsubota K. Decrease in corneal sensitivity and change in tear function in dry eye. Cornea 1996;15:235-239.
11. Ousler GW, Gomes PJ, Welch D, and Abelson MB. Methodologies for the study of ocular surface disease. The Ocular Surface 2005;3:3:143.
12. Abelson, MB, Ousler GW, Nally, LA, et al. Alternative reference values for tear film break up time in normal and dry eye populations. In: Sullivan D, ed. Lacrimal Gland, Tear Film, and Dry Eye Syndromes. New York, Boston , London, Moscow: Kluwer Academic/Plenum Publishers, 2002:1121-1125.
13. Sall K, Cohen SM, Christensen MT, et al. An evaluation of the efficacy of a cyclosporine-based dry eye therapy when used with marketed artificial tears as supportive therapy in dry eye. Eye & Contact Lens 2005;31:3: [in press].