The Irish physicist and engineer Lord Kelvin famously said, “To measure is to know,” and used this attitude of scientific rigor to advance research in a number of fields. Dry-eye researchers are beginning to appreciate the power of quantifiable values as well, as new devices for measuring aspects of tears begin to work their way into practice. Here is a look at the research behind these new instruments and experts’ opinions on their ability to aid diagnosis and treatment by adding a quantifiable dimension to the process.
LipiView
|
LipiView uses interferometry to measure the lipid layer’s thickness between blinks, and gives a quantitative assessment in interferometric color units, which the company says are close to, but not exactly, nanometers. One study of lipid layer thickness found a connection between a patient’s lipid layer thickness and his dry-eye symptoms. In the study, researchers had 137 consecutive patients complete the Standard Patient Evaluation of Eye Dryness questionnaire, and then measured their lipid layers with interferometry. For patients with severe dry-eye symptoms (a SPEED score of 10 or greater), 74 percent also had LLT of 60 nm or less. On the other end of the spectrum, 72 percent of patients with no symptoms (SPEED score of zero) had a LLT of 75 nm or thicker. When the researchers performed a linear regression analysis, there was a statistically significant relationship between LLT and symptom score, and as LLT increased, symptom score decreased (p=0.0014).1
“I’ve seen patients with signs and symptoms of evaporative dry eye who come in and undergo LipiView, confirming a deficient lipid layer,” says Duke surgeon Alan Carlson, who consults for TearScience and has been using the LipiView/LipiFlow system for 11 months. “It’s not uncommon for a patient to have, for example, 28 to 35 ICU values measured by LipiView that improve after a LipiFlow treatment and a regimen to get the glands functioning again. They may even double or triple their lipid layer. And this often correlates with a notable improvement in their symptoms. Dry-eye patients are heterogeneous and complex, and are dealing with a chronic disease process. The duration and severity of disease can cloud the patient’s own assessment and measure of improvement. LipiView testing that shows a two- to threefold increase in lipid layer thickness in addition to the improvements seen on examination can further encourage the patient with respect to progress and prognosis.”
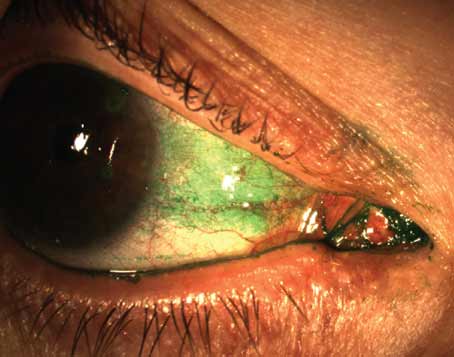
Dr. Carlson says LipiView has worked its way into the set of tests he administers. “I perform a meticulous slit lamp exam, assessing blink, lid margin, the meibomian glands and gland orifices,” he explains. “Then I look at staining patterns, tear film stability, LipiView and meibography. This combination of testing helps us sort out the root cause. We’re finding that it is a minority of patients who have dry eye whose primary cause is deficient tear production, while the majority of patients with tear-film instability [evaporative dry eye] have issues related to meibomian gland dysfunction and gland obstruction.”
Though the LipiView system is approved and in use, physicians and the company are still learning the best ways to use it in a clinical setting. “We haven’t been able to precisely correlate LipiView in every case with outcomes and perceived patient response,” says Dr. Carlson. “We’d like to be able to. There is a company-sponsored study looking at this as well as looking at the test’s correlation with other dry-eye findings and tests, and the data is still being gathered. While we look forward to improving our ability to better define the magnitude and duration of response to LipiFlow based on a multitude of findings—including LipiView—it’s remarkable to reflect on the progress we’ve made in a single year with respect to diagnosing and understanding the treatment needed for dry-eye patients who have their condition on the basis of MGD leading to deficient tear-film stability rather than inadequate tear production.”
TearLab Osmolarity Testing
The TearLab system uses a small sample of a patient’s tears to test the concentration of electrolytes in the tear film, which gives an osmolarity reading. Patients with higher levels of osmolarity, especially within certain ranges, are likely to have dry-eye disease.
|
When the measurement is returned, the physician can identify a dry-eye patient in one of two ways: one of the eyes has an osmolarity of 308 mOsm or higher; or there is a difference between the two eyes of 8 mOsm or greater, since tear-film instability between eyes is also a hallmark of the disease. The device itself has a variability of 1.5 percent, which Dr. Lemp says translates into about 5 mOsm. “In addition, we’ve found that a reading of 316 mOsm is a good cutoff between mild and moderate dry-eye disease,” he adds.
Dr. Lemp says assigning a value to the patient’s ocular surface helps ferret out patients who might otherwise go undiagnosed. “We know that in mild to moderate dry-eye disease, less than half of the patients have any corneal staining,” he says. “Yet many doctors might think if a patient doesn’t have staining he doesn’t have disease, and would miss 50 percent of patients with mild to moderate disease. Also, up to 40 percent of patients with clear objective evidence of dry eye are asymptomatic.”
Dr. Lemp says that there have been some articles published that question TearLab’s utility. A poster presented at the annual meeting of the Association for Research in Vision and Ophthalmology found no correlation between signs and symptoms of dry eye, including tear osmolarity. (Sullivan BD, et al. IOVS 2012;53:ARVO E-Abstract 550) The researchers noted, though, that the “clinical presentation of dry eye is multifactorial, with each test contributing different information, thus correlation between different tests should not be expected.”
A recent study from Hungary reported that tear osmolarity wasn’t able to distinguish between normals and patients with dry eye,2 but Dr. Lemp says that the study had issues, and is drafting a response letter to the journal. “In that study, the researchers tested only one eye rather than two, so they didn’t understand about variability,” he avers. “And the study is guilty of selection bias, in that they qualified people for inclusion in the study by using the results of Schirmer’s, tear-film breakup time and corneal staining, but not osmolarity testing. Then, during the study, the researchers asked how well the first three tests correlated in each patient, and found that the tests correlated well. This is no surprise, though, because these initial tests all needed to be positive in order for the subjects to enter the study. The researchers then reported that tear osmolarity didn’t correlate well, but this wouldn’t be unusual because it wasn’t one of the entry criteria like the others.”
Other studies, meanwhile, have found good reliability from tear osmolarity measurements.3,4 One multicenter study performed by Dr. Lemp and several colleagues analyzed 314 patients to see how well six major dry-eye tests (including osmolarity, Schirmer’s and tear-film breakup time) correlated to the increasing severity of dry-eye disease. The researchers say that, using a cutoff of 312 mOsm/L, tear hyperosmolarity exhibited 73-percent sensitivity and 92-percent specificity. They say that the other tests exhibited either poor sensitivity or poor specificity. Also, inter-eye differences in osmolarity were found to correlate with increasing disease severity (r2 = 0.32).
Dr. Lemp says they’re always learning more about the disease and what osmolarity can tell them about it. “In work we’ve done in Turkey, over a three-month period of treatment with cyclosporine in bona fide cases of dry eye, it took two months before we saw a profound lowering of osmolarity,” he says. “However, the symptoms didn’t go down by a statistically significant amount until three months. This lag is understandable, because even though the surface has gotten better at two months, it hadn’t gotten better to the point where the patient could perceive it. We’ve learned it takes some reparative time before that occurs.”
Inflammadry
Inflammadry (Rapid Pathogen Screening, Sarasota, Fla.) is a test similar to an at-home pregnancy test that takes a sample of a patient’s tears and gives a positive (ocular surface disease) or negative (no ocular surface disease) result. Users say that, though it doesn’t give a numerical result, the test’s reading is actually based on a quantifiable value of the amount of matrix metalloproteinase-9 in the tears. “If the test is positive, then basically that means there’s over 40 ng/ml for the level of MMP-9,” says Ottawa’s Bruce Jackson, MD, who has done studies with Inflammadry but has no financial interest in the device. “The company has looked at the levels in a normal eye, and found 40 ng/ml to be the upper range of normal.
|
To perform the test, the clinician takes a sample of tears from the inside lining of the lower lid. Ten minutes later, if a red line appears in the result window of the detector, that indicates elevated MMP-9. There isn’t a lot of independent research on Inflammadry at the moment, but in RPS studies, the company found the test to have 85-percent sensitivity and 94-percent specificity.5
Dr. Jackson says that, using the Dry Eye Workshop levels of tear dysfunction, patients ranked as “mild” are more in the normal range of Inflammadry, “but you start to pick up abnormal levels at level two, three and four,” he says. “And, the stronger the red line, the higher level. It goes up in both Sjögren’s and MGD, so it can give you a really good idea of whether there are inflammatory mediators in the tears.”
Inflammadry isn’t approved in the United States and, though it’s approved in Canada, it currently has no distributor there, so Dr. Jackson can only use it for research projects at the moment. “When it’s available, though,” he says, “I’ll combine it with the use of the TearLab osmolarity test and get a better idea of where it fits in the clinic.”
Anterior-segment OCT
A system currently more in the research realm than the everyday practice is anterior-segment optical coherence tomography (coupled with custom-made, third-party image processing software) for the measurement of tear characteristics. Here’s a look at what researchers are finding with these systems.
In one study of 48 aqueous-deficient patients and 47 controls, researchers found clues for diagnosing dry eye on OCT: They reported that the cutoff value for an abnormal lower tear meniscus radius was 182 µm and the value for a an abnormal lower tear meniscus height was 164 µm. They added that the LTMR diagnostic sensitivity and specificity were 0.92 and 0.87, respectively, and that the LTMH diagnostic sensitivity and specificity were 0.92 and 0.90. The tear meniscus was smaller in aqueous-deficient patients than in healthy subjects.6
Looking at treatment, researchers used OCT to image the upper and lower tear menisci in 14 consecutive dry-eye patients. They then started the treatment group on daily cyclosporine administration and repeated the measurements at one and two months.
They found that, in the treatment group, measurements showed significant increases of both upper (p=0.003) and lower (p=0.0003) tear menisci heights, after a month of cyclosporine. The tear meniscus volumes in the treatment group after one month of treatment showed significant increases of both upper (p=0.007) and lower (p=0.007) tear menisci. At two months, the increase in the tear meniscus was still evident (p<0.05).7
Though the expense of acquiring a high-res OCT, and the intricacies of dealing with third-party custom software for image management prohibit OCT tear measurement from being widespread, researchers say that the rapid, noninvasive, and detailed images from OCT can often provide them with helpful insights about the presence of dry eye and the effectiveness of therapies. REVIEW
1. Blackie CA, Solomon JD, Scaffidi RC, et al. The relationship between dry eye symptoms and lipid layer thickness. Cornea 2009;28:7:789-94.
2. Szalai E, Berta A, Szekanecz Z, et al. Evaluation of tear osmolarity in non-Sjögren and Sjögren syndrome dry eye patients with the TearLab system. Cornea 2012;31:8:867-71.
3. Versura P, Profazio V, Campos EC. Performance of tear osmolarity compared to previous diagnostic tests for dry eye diseases. Curr Eye Res 2010;35:7:553-64.
4. Jacobi C, Jacobi A, Kruse FE, et al. Tear film osmolarity measurements in dry eye disease using electrical impedance technology. Cornea 2011;30:12:1289-92.
5. Data on file, Rapid Pathogen Screening, Protocol #100310.
6. Meixiao Shen, Jianhua Li, Jianhua Wang, et al. Upper and Lower Tear Menisci in the Diagnosis of Dry Eye. Invest Ophthalmol Vis Sci 2009;50:2722–2726.
7. Wang J, Cui L, Shen M, et al. Ultra-high resolution OCT for monitoring tear meniscus volume in dry eye after topical cyclosporine treatment. Clin Ophthalmol 2012:6:933–938.