Workup, Diagnosis and Treatment
Upon presentation to the Wills Eye emergency room, the patient underwent CT of the orbits, which re-demonstrated the left orbital floor and medial wall fractures and also showed a prolapsed orbital mass in the left maxillary sinus (Figure 2A). The restricted vertical forced ductions on the left side were not thought secondary to an entrapped extraocular muscle, so the patient was discharged with a follow-up appointment with the oculoplastics service. He was seen the next day, at which time a prior history of a left orbital mass was elicited. MRI of the orbits had been performed prior to the trauma and had revealed an extraconal mass in the left inferomedial orbit (Figure 2B). Given the patient’s presentation with symptomatic diplopia, restriction of upgaze, and hypoglobus, the decision was made to perform surgery one week after the initial accident.
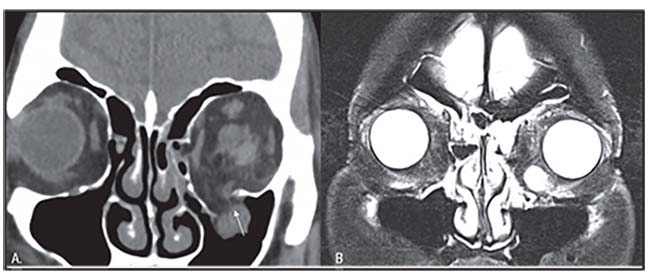 |
| Figure 2. CT of the orbits after a mechanical fall, showing left medial and orbital floor fractures with prolapse of an orbital mass into the left maxillary sinus (A, arrow). MRI of the orbits prior to trauma shows an enhancing mass in the left inferomedial orbit (B, arrow). |
The patient underwent orbital exploration, during which the orbital floor was exposed and a mass was found in the left maxillary sinus. A cryoprobe was used to elevate the mass out of the maxillary sinus, and it was resected and sent to pathology. The orbital floor fracture was then repaired with placement of a 1.5 mm porous polyethylene implant. Histopathologic examination of tissue from the orbital mass revealed an encapsulated mass composed of bland spindle cells that stained positively for S-100 protein and negatively for smooth muscle actin and Stat6 with the presence of nuclear palisading. The pathologic findings were consistent with a diagnosis of benign peripheral nerve sheath tumor, specifically orbital schwannoma. The patient healed well postoperatively with resolution of diplopia, restoration of extraocular motility and no recurrence of orbital schwannoma (Figure 3).
 |
| Figure 3. External photo showing resolution of left periorbital ecchymosis, edema and hypoglobus after removal of the left orbital mass and repair of the orbital floor fracture. |
Discussion
The differential diagnosis of a solitary orbital mass in an adult is broad and varies depending on the location within the orbit as well as the specific age of the patient. Overall, the most common benign orbital mass in adults is cavernous hemangioma, which is a well-encapsulated mass that tends to occur at the lateral aspect of the intraconal space.1,2 Also known as cavernous malformations, these are congenital vascular anomalies present at birth that grow slowly over time and tend to present in adults aged 43 to 48 years, particularly females.3 If small and asymptomatic, cavernous hemangiomas are observed with annual or biannual exams and imaging. However, if symptomatic with visual changes and/or diplopia, they are surgically excised.4
Initially, the patient in this case was thought to have a cavernous hemangioma that had prolapsed into the maxillary sinus after trauma, given that this is the most common benign orbital tumor in adults. In addition to cavernous hemangioma, the differential diagnosis of well-encapsulated orbital tumors includes peripheral nerve sheath tumors (schwannoma and neurofibroma), hemangiopericytoma, fibrous histiocytoma, solitary fibrous tumor and melanoma. If this patient’s lesion had been found without simultaneous trauma, the most likely management would have been observation. However, given recent trauma with concomitant orbital fractures and symptomatic diplopia, the orbital mass was removed surgically. It’s likely that the mass being pulled into the maxillary sinus worsened the patient’s restriction of upgaze. Upon histopathologic examination of the mass, a diagnosis of schwannoma was rendered.
Schwannomas, also known as neurilemmomas or neurinomas, are the most common type of benign peripheral nerve sheath tumor of the orbit, where peripheral nerve sheath tumors represent 2 percent of all orbital neoplasms.5 Orbital schwannomas grow slowly and tend to affect adults in the third to seventh decades of life.6 They typically arise from trigeminal nerve branches, particularly in the superior orbit with concomitant inferior displacement of the globe.7 Patients with orbital schwannomas present with insidious proptosis and lid swelling, with later signs and symptoms including diplopia, restriction of extraocular movements, decreased visual acuity and sequelae of optic nerve compression.8 Pain and paresthesia can also occur depending on the specific nerve involved and the extent of growth.
CT and MRI can both be used to further characterize orbital tumors. In the case of orbital schwannomas, CT scan will demonstrate a smooth, well-circumscribed mass that most commonly occurs in an extraconal location rather than the traditional intraconal location of cavernous hemangiomas.1 On MRI, the degree of heterogeneity of orbital schwannomas depends on the pathologic pattern of the tumor.6 Pathologically, orbital schwannomas stain positively for S-100 protein and demonstrate one of two patterns, termed Antoni A or Antoni B. The Antoni A pattern consists of tightly packed Schwann cells with nuclear palisading, as in our case, while the Antoni B pattern consists of loosely packed Schwann cells within the capsule.6
| Orbital schwannomas grow slowly and tend to affect adults in the third to seventh decades of life. |
One study found that the Antoni A pattern correlates with hyperintensity on T1-weighted and hypointensity on T2-weighted imaging, while the Antoni B pattern correlates with hypointensity on T1-weighted and hyperintensity on T2-weighted imaging.6 In addition, if an orbital schwannoma is long-standing, degenerative changes on MRI such as hemorrhage, cavity formation and calcification may be evident.7 In one retrospective interventional case series, patients with cavitary change or heterogeneous signal intensity on T2-weighted MRI images were more likely to demonstrate Antoni B patterns on pathologic examination, which also corresponded to a more friable tumor and fragmented surgical excision.9
Management of orbital schwannoma includes en bloc resection with preservation of capsular integrity of the tumor. Surgical approaches vary depending on tumor location, with anterior orbitotomies used for schwannomas in the superior orbit, lateral orbitotomies used for superolateral tumors and inferior transconjunctival approaches used for inferior or medial lesions.10 Alternatives for small, unresectable tumors include multisession gamma knife radiation therapy, though results are variable and the procedure involves a risk of vision loss from optic neuropathy.11 Orbital schwannomas require long-term follow-up to monitor for recurrence or malignant transformation, both of which rarely occur with total excision.12
In conclusion, orbital schwannoma should be considered on the differential diagnosis of a well-circumscribed extraconal orbital mass, although they are rare among all causes of orbital neoplasm. Although observation was an option, the patient in this case underwent resection since he had diplopia and restriction of extraocular motility in the setting of unrelated orbital fractures. REVIEW
1. Tailor TD, Gupta D, Dalley RW, et al. Orbital neoplasms in adults: Clinical, radiologic, and pathologic review. Radiographics 2013;33:6:1739-58.
2. Harris GJ, Jakobiec FA. Cavernous hemangioma of the orbit. J Neurosurg 1979;51:2:219–28.
3. Smoker WR, Gentry LR, Yee NK, et al. Vascular lesions of the orbit: More than meets the eye. Radiographics 2008;28:1:185.
4. Shields JA, Shields CL. Orbital schwannoma. In: Shields JA, Shields CL, eds. Eyelid, Conjunctival and Orbital Tumors. An Atlas and Textbook, 3rd ed. Philadelphia: Wolters Kluwer, 2016:552–5.
5. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:5:997–1008.
6. Pointdujour-Lim R, Lally SE, Shields JA, et al. Orbital schwannoma: Radiographic and histopathologic correlation in 15 cases. Ophthalmic Plast Reconstr Surg 2018;34:2:162-167.
7. Wang Y, Xiao LH. Orbital schwannomas: Findings from magnetic resonance imaging in 62 cases. Eye (Lond) 2008;22:8:1034–9.
8. Singh M, Singh U, Zadeng Z, et al. Clinico-radiological spectrum and management of orbital schwannomas: A tertiary care institute study. Orbit 2013;32:3:171-77.
9. Gunduz K, Shields CL, Gunalp I, et al. Orbital schwannoma: correlation of magnetic resonance imaging and pathologic findings. Graefes Arch Clin Exp Ophthalmol 2003;241:7:593-597.
10. Goldberg RA, Rootman DB, Nassiri N, et al. Orbital tumors excision without bony marginotomy under local and general anesthesia. J Ophthalmol [open-access journal] 2014;2014:424852.
11. Kim MS, Park K, Kim JH, et al. Gamma knife radiosurgery for orbital tumors. Clin Neurol Neurosurg 2008;110:10:1003-7.
12. Kapur R, Mafee MF, Lamba R, et al. Orbital schwannoma and neurofibroma: role of imaging. Neuroimaging Clin N Am 2005;15:1:159-74.



