Here, several surgeons with experience using the procedure discuss what they’ve learned about cross-linking with the epithelium on (rather than off); which parameters of light, riboflavin and timing work the best; and how these answers are modified when cross-linking is used in different ways.
Epi-on vs. Epi-off
In order for stromal cross-linking to take place, riboflavin must make it past the epithelium and permeate the corneal stroma. Because the corneal epithelium is an effective barrier to most formulations of riboflavin, the original protocol for cross-linking, now known as the Dresden protocol, required removing the epithelium before applying the riboflavin solution to the cornea. While this protocol is undeniably effective, from the outset researchers hoped to find a way to make the procedure work without having to remove the epithelium.
A. John Kanellopoulos, MD, clinical professor of ophthalmology at NYU Medical School and medical director of the Laservision.gr Institute in Athens, Greece, notes that the desire to make epi-on cross-linking work is understandable. “If collagen cross-linking were to become a purely epithelium-on procedure, the morbidity, the patient’s everyday activity disturbance and possibly a large number of potential complications that relate to healing and infection could be minimized,” he says. “In the early 2000s I saw a few of the initial epi-on treatment attempts in the United States in an investigative protocol. Four out of the five ectasia patients I saw continued to progress. In fact, in vitro work in the laboratory showed that using the classic Dresden protocol with the epithelium on resulted in almost no riboflavin penetrating the epithelium and little cross-linking taking place in the stroma.
“However, a lot of things have changed since then,” he continues. “Multiple techniques have been developed that help to get the riboflavin molecules past the epithelium, such as iontophoresis, adding special ‘epi-abrasive’ ingredients to the riboflavin solution, using higher concentrations of riboflavin, and also a technique that we introduced: creating a femtosecond laser pocket in the cornea and placing the riboflavin inside it, thus bypassing the issue of riboflavin penetrating through the intact epithelium. Some of the data regarding these variations, although anecdotal, appears promising. If we can facilitate riboflavin penetrance into the cornea, I think epi-on will be a valid technique.”
Dr. Kanellopoulos points out that leaving the epithelium on not only makes it difficult to get the riboflavin into the stroma but also can minimize passage of the UV light into the stroma. “If you place the riboflavin solution on the cornea with the epithelium intact, the epithelium becomes soaked with riboflavin molecules,” he explains. “Then, during the exposure to UV light, the epithelium acts as an umbrella, absorbing a lot of the light. Depending on which study you look at, 20 to 80 percent of the UV light intended to reach the corneal stroma may be blocked. Clearly, this will reduce the amount of cross-linking achieved. Also, based on what I’ve seen clinically and the laboratory work we’ve done ex vivo, I’m convinced that effective epi-on cross-linking will require increasing the amount of energy we deliver.”
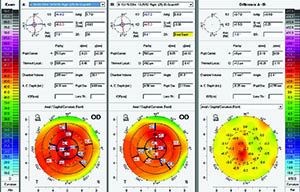
Despite these caveats, Dr. Kanellopoulos says some of his group’s work with using cross-linking to cause a refractive change has supported the potential efficacy of epi-on approaches. “In a study we conducted of the refractive effect of customized, very high-fluence cross-linking, the epi-on cases did have a quite impressive refractive effect,” he says. (See example, p. 26.) “This demonstrates that epi-on cross-linking can be effective in certain areas of the cornea, although it appears to be about half or one-third of the amount achieved using epi-off.”
Of course, in some cases an epi-off procedure may be a good thing; there can be advantages to removing the epithelium besides giving the riboflavin easier access. Like many surgeons who perform cross-linking, Arturo S. Chayet, MD, who practices at the CODET Vision Institute in Tijuana, Mexico, still does epi-off exclusively. “The potential advantages of epi-on are obvious, but we still use the Dresden protocol,” he says. “One reason for this is that most of our patients receiving cross-linking have a moderate to high spherical equivalent and amount of cylinder, so we’re removing the epithelium using phototherapeutic keratectomy. This has an effect similar to topography-guided ablation; the epithelium breaks first in the area of the steeper cornea where the cone is. We’re getting really good refractive results just by doing this, followed by the cross-linking. So at this point, even if I had the opportunity to do epi-on, I would continue to do epi-off because of the refractive issues.”
|
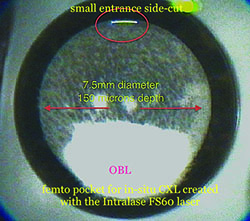
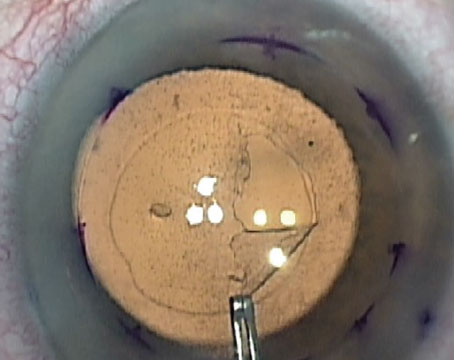
Putting It in the Pocket
One approach that allows riboflavin to get into the stroma without having to breach the epithelium is the creation of a corneal pocket using a femtosecond laser. Dr. Kanellopoulos describes the method his group has developed. “In our original study we created a femtosecond laser pocket and placed riboflavin 0.1% in the pocket, avoiding any contamination of the riboflavin solution with the surface of the cornea,” he says. (See picture, above.) “Then we performed high-fluence, high-energy cross-linking using 10 mW/cm2 exposure for about 10 minutes. The cross-linking this produced was very similar to that achieved with the Dresden protocol, although the corneal strength measurement methods we used to gauge the results were a bit different.
“We’ve studied this technique more elaborately ex vivo in the past few years, comparing the use of a femtosecond laser pocket, and/or a LASIK flap,” he continues. “In one set of eyes we placed the riboflavin in the corneal pocket. We performed mock LASIK in the LASIK eyes, placed riboflavin in the stromal bed and replaced the flap. Then we exposed both sets of corneas to very high-fluence and high-energy UV light. To determine how much cross-linking took place, we analyzed the corneas biomechanically by two-dimensional stretching and by resistance to enzymatic digestion. In the pocket eyes we found almost a 100-percent increase in the biomechanical rigidity of the cornea. So ex vivo we showed that we can double the strength of the cornea if we place riboflavin in the cornea and have the UV light go through the intact epithelium and reach that riboflavin midway in the cornea.
“As you might expect, the corneal strength was not as great in the mock-LASIK eyes, because we were only cross-linking the part of the cornea left after making the flap,” he notes. “When we create a pocket, the rest of the cornea is intact and it retains its biomechanical stability. In the LASIK corneas, we were trying to minimize the flaps’ exposure to the riboflavin, and we succeeded; postop, control and cross-linking flaps had equal biomechanical strength. That means that after the LASIK procedure we were testing the biomechanical rigidity of just the residual cornea—perhaps a 320-µm cornea instead of a 550-µm cornea. And of course the strongest tissue in the cornea is in the anterior cornea, which becomes part of the flap.”
Dr. Kanellopoulos notes several advantages to the pocket technique. “This is a surgical procedure, of course, but horizontal incisions in the cornea do not affect biomechanics,” he says. “It’s the vertical incisions made in LASIK flaps that cause more than 95 percent of the biomechanical changes in the cornea after LASIK. When creating a pocket, the only biomechanically active part of the pocket would be the little incision that gives you access to the pocket; the rest of the pocket has no effect on the biomechanical strength of the cornea. There’s also minimal danger of cutting corneal nerves. The nerve plexus is in the anterior 100 µm of the cornea, while the pocket is between 150 and 200 µm in depth, so you’re way under the superficial cornea nerve plexus. Of course, it’s possible that the cross-linking procedure itself may affect the nerves, but that’s entirely theoretical at this point.”
Cristhian Sancho, MD, who works at the Laser Center Visión 20/20 in Pichancha, Ecuador, and is an ophthalmology consultant at Fundacion Vista Para Todos, has been using cross-linking since 2008. “At this point in time we’ve tried most of the cross-linking machines,” he says. “We’ve tried treatments ranging from 3 to 45 mW and from 3 to 15 J. We’ve done monocular and binocular treatments and tried both epi-off and epi-on. In terms of epi-on, we’ve tried different riboflavin formulations without much success, so I recommend using epi-on only in very mild cases.”
Dr. Sancho says he has also tried the technique of using a femtosecond laser to create a pocket for the riboflavin solution. “The advantage is the recovery time,” he notes. “The downside is the cost.”
Independent Research
The problems with epi-on cross-linking center around the difficulty of getting riboflavin through the intact corneal epithelium. However, different formulations have different levels of success because of their chemical structure, and it appears that a consortium of American doctors interested in studying cross-linking, known as CXL-USA, may have discovered a formulation that penetrates the epithelium quite rapidly.
| ||||||
Dr. Rubinfeld says it’s been very helpful to do this research without commercial involvement. “In a commercial trial, whatever protocol you go in with is what you have to continue to do for the next few years,” he says. “Once you set up an FDA trial, for example, you have to stay with the chosen technique, metrics and timing. In general, no matter what you learn during the years of conducting the trial, you can’t use any of that knowledge to innovate and improve. You have to follow the pre-established
protocol.
“In our world, because we write our protocols with some flexibility in them and the ability to incorporate innovation, we haven’t had that limitation,” he says. “When we’ve figured out that something works better, we’ve switched to it. For example, we tried many riboflavin formulations that took one to three hours to load into the stroma through intact epithelium. We just kept modifying them and the delivery techniques until we found ways to consistently, reliably and homogenously load through intact corneal epithelium in 20 minutes or less, and then we switched to that protocol. We’ve been able to be much more innovative and agile than commercial trials can be.”
Perfecting Epi-on
Dr. Rubinfeld notes that finding a formulation of riboflavin that could readily penetrate intact epithelium has been a central focus of the CXL-USA group. “If you can do cross-linking without scraping off the epithelium, anybody would prefer that,” notes Dr. Rubinfeld. “Even people who have strongly defended the epi-off approach are now saying, ‘If you can get the riboflavin in, and the UVA light gets in and the oxygen is present in the corneal stroma, you’re going to get good cross-linking.’ And everyone agrees that it would be great if patients didn’t have to undergo four to seven days of discomfort and the risk of infection, haze, scarring and perforation—all of which have been reported with epi-off. Epi-on is an inherently noninvasive treatment, and everybody wants epi-on to work.
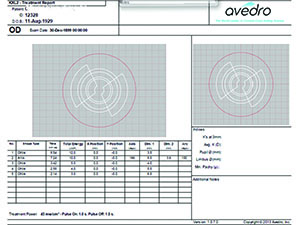
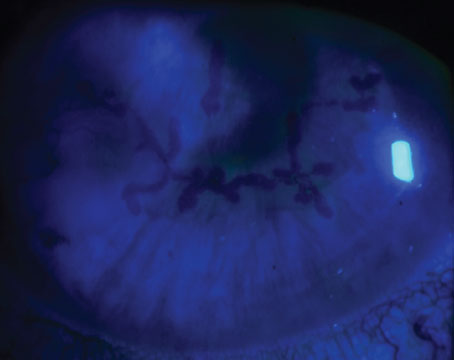
“At CXL-USA we have developed a proprietary, patent-pending riboflavin formula that’s specifically formulated for rapid, consistent, homogeneous riboflavin stromal loading with the epithelium intact,” he explains. “We’ve tried and observed many other formulations in our many studies, including two commercial formulations available in Europe that are specifically designed for transepithelial cross-linking. However, we were disappointed with the results they produced. Using our new formulation, our investigators across the United States have been able to load both eyes in 20 minutes or less. We also have a proprietary, patent-pending loading delivery system that does not involve iontophoresis. Based on our formulation and protocol, we’re consistently able to load the stroma quickly and easily and get very effective cross-linking. (See example, above.) Of course I’m biased, but if I were having cross-linking, this would be my preferred approach. In fact, William Trattler, MD, one of our key investigators, did treat his 12-year-old daughter with our epi-on technology. It not only stopped her disease progression but improved her acuity as well.”
Dr. Rubinfeld says the surgeons in CXL-USA started with epithelium-off treatments at the outset. “Like everyone else, we simply didn’t believe that epi-on could work,” he notes. “With those early formulations, it took two to three hours or more to get adequate stromal loading through the epithelium in the first set of corneas we treated. It was not a pleasure for the patients or the staff. Over time we’ve adjusted key characteristics of the formulation until we developed the current version. It makes the loading process work consistently, smoothly and easily. Patients really appreciate a short procedure—lying there for 20 minutes listening to music, as opposed to an hour or more. The next day, they’re back to their normal activities because we haven’t removed their epithelium. They’re seeing well. Usually they drive to the office for their one-day-postoperative visit.”
|
“The other nice thing is that once you get the riboflavin through the epithelium, it diffuses nicely through the stroma,” he adds. “The epithelium has a lot of lipids and other barriers to penetration of water-soluble solutions on the surface, whereas the stroma is mostly water and is completely water-soluble. Riboflavin is also incredibly water-soluble, so it diffuses easily throughout the stroma. That’s one reason other innovations like femto pockets or channels or partial-scraping procedures work. They just need to get the riboflavin through the intact epithelium; then it spreads throughout the stroma. Of course, with our riboflavin formulation, laser pockets and channels are not necessary. Those approaches were developed because other riboflavin formulations are unable to penetrate the epithelium well.”
Dr. Rubinfeld agrees that riboflavin in the epithelium can theoretically block some of the UV light from reaching the stroma. “Not only will that block some UVA light, it will also consume some of the oxygen needed in the stroma for cross-linking to occur,” he says. “We don’t want that. But in our proprietary technique the epithelium is crystal clear after loading, indicating that the riboflavin isn’t getting trapped there. At the same time, the stroma is well-loaded with green in a homogeneous concentration. So our protocol avoids this problem.”
Fine-tuning Parameters
One of the big questions still being resolved is what combination of fluence and timing is most effective in any given version of cross-linking. In theory, increasing the amount of light being used should decrease the time required to complete the cross-linking.
“This is another point that has not been studied thoroughly,” says Dr. Kanellopoulos. “I know that Avedro has conducted a multicenter study in the United States addressing this question by comparing the effect of several different fluences, and I understand that the preliminary data indicate pretty similar results. However, we’d like to see this studied by an independent body or in a multicenter trial, because Avedro has a vested interest in higher-fluence cross-linking being better. I believe their instrument is still the only device that can generate more than 30 mW/cm2 of fluence.
“We use a big spectrum of fluences and energy levels in our practice,” he continues. “They’ve changed significantly over the years. Cross-linking is 50 percent of our practice, and the standard keratoconus patient—usually a young male—accounts for about 80 percent of the cross-linking we perform. In the great majority we perform the Athens protocol, which has now been established as a valid treatment, although many centers use slight variations of it under a different name such as the Dubai protocol, the Montreal protocol or the Dublin protocol.
|
Dr. Kanellopoulos adds that when performing epi-on cases he may use energies up to 20 J. “This is four times the Dresden protocol,” he notes. “But as I said before, one has to take into account that a lot of this energy may get lost on its way to meeting the riboflavin in the cornea.”
In terms of finding the right protocol for a basic epi-off procedure, Dr. Kanellopoulos notes that you have to balance the advantages and disadvantages of changing the parameters. “We started using double the classic Dresden protocol energy levels as far back as 2006,” he says. “We found that doubling the levels minimized most of the corneal dehydration problems and corneal thinning, while shortening the procedure from 30 minutes to 15. When higher-fluence devices became available, we tried using even more fluence for less time, but we found that we achieved a more superficial cross-linking effect. That is not ideal, because in keratoconic eyes we want to cross-link as deeply as possible to ensure long-term stability. So we went from 6 mW/cm2 to 10, to 15, to 30. Finally we went back to 6 mW/cm2, because we found by studying these corneas with OCT that we had the deepest and widest distribution of cross-linking effect in the corneas at this fluence. These parameters gave us the greatest efficacy, while minimizing dehydration problems and potential epithelial toxicity.
“I’m aware that some surgeons are currently using higher fluence,” he adds. “I applaud them for collecting data and showing its effect. But I think for the patient, going from 15 minutes to 10 or 8 minutes doesn’t make that much difference. On the other hand, I think going from 30 minutes to 15 is a huge difference.”
Dr. Rubinfeld says he is not an advocate of high fluence. “More is not always better,” he notes. “The rate-limiting factor in the cross-linking reaction is oxygen, and the more UV you use, the more you deplete that rate-limiting agent. I think of it as being like a recipe. If the recipe says to bake a pan of brownies for 30 minutes at 300 degrees, trying to bake it for three minutes at 3,000 degrees probably won’t produce the result you’re hoping for. You might be able to improve upon the original formula, but there are bound to be limits. We [at CXL-USA] have aimed to create a highly effective corneal strengthening procedure that’s the least inflammatory and most respectful of the health of the corneal cells and the patient’s comfort.”
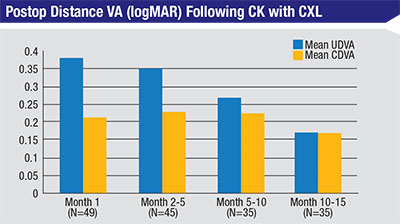
Adjusting by Procedure
As surgeons around the world try cross-linking for purposes beyond controlling keratoconus and ectasia, they’re finding that different parameters make sense in different situations. “Today we’re using cross-linking technology not only for keratoconus but for refractive corrections and treating bacterial keratitis and corneal ulcers,” says Dr. Sancho. “When treating bacterial keratitis, I’ve found that a long exposure time is better, since we’re using the UV light to eradicate the bacteria. We also combine refractive surgery with cross-linking. We don’t need too much exposure time to get a reproducible result in refractive cases.”
|
“The protocols we use are always changing depending on the case to be treated,” notes Dr. Sancho. “The fluence we use depends on the instrument being used and the riboflavin vehicle; there are different indications depending on the manufacturer. Using the wrong fluence or riboflavin can produce severe endothelial damage. At the same time, using less than sufficient energy produces less effect and not much change in keratometry. Generally, we’ve gotten better results with more fluence. That’s especially true with our new custom system with eye tracking that makes it possible to apply different fluences in different areas. To treat keratoconus I currently use 7.2 J at 30 mW with 10 minutes of induction time. That has resulted in reproducible results for the past two years.
“Using more fluence we’re able to get refractive changes,” he adds, “but it’s important to choose the case. In the future I believe we will be able to do effective refractive correction by reshaping the cornea with cross-linking. I’m working on that today, with very promising early results. So far I’ve only done 120 cases, with various results, but I believe that’s the future.”
What We’ve Learned
As individuals and groups continue to research cross-linking, several things are becoming clear.
• It’s reasonable to expect some individual variation in outcomes. Dr. Kanellopoulos notes that when performing refractive cross-linking with an epi-on protocol, some patients showed less of an effect than others. “We’ve had good results in most patients, but there have been a few outliers who showed little or no effect from the procedure,” he says. “We have no explanation for that. We don’t know if it’s because of a glitch in the epithelium, a problem with our technique or an intrinsic behavior of the cornea. Maybe not every cornea reacts the same to the cross-linking effect.
“It’s worth noting that we see far less variability in the effect in different corneas when performing epi-off procedures,” he adds. “The standard deviation is smaller by a factor of four when you’re studying epi-off.”
• More riboflavin is not necessarily better. Dr. Rubinfeld says that many surgeons believe that using more riboflavin is better because it will result in more cross-linking. “That’s not correct,” he says. “Riboflavin acts much like a catalyst. Chemists used to talk about ‘adding a pinch of catalyst.’ The reality is, you need a certain amount of riboflavin to trigger the cross-linking reaction, but adding more doesn’t make the reaction go faster or produce better results. In fact, if you get too much riboflavin in the path of the UV light, you’ll just attenuate or block the light available for the reaction.”
• Previous cross-linking doesn’t seem to reduce the effect. “We’ve been surprised to discover that we are able to get a significant refractive cross-linking effect in corneas that were previously cross-linked,” says Dr. Kanellopoulos. “If I had to guess, I would have thought that in corneas that had been cross-linked before you’d see less of a cross-linking effect. But we found that even patients who had the Athens protocol six years ago showed a very compelling refractive effect when treated with refractive cross-linking this year.”
• The presence of oxygen may be crucial. “The chemistry involved in the cross-linking process isn’t complicated,” says Dr. Rubinfeld. “You need an adequate amount of riboflavin; you need UV light; and you need oxygen. We used to think that oxygen didn’t play a very important role, but it turns out that it does—in fact, it’s the rate-limiting factor. The problem is, when the light is on, you’re depleting molecular oxygen in the cornea, and oxygen can’t diffuse back into the cornea to replenish the supply with the UVA light on. Essentially, you’re making the cornea hypoxic. That’s why oxygen is the rate-limiting factor in the cross-linking reaction.
|
What’s Next?
With so many different ways of using cross-linking, and so many ideas about the optimum parameters, the field of cross-linking is currently awash with uncorrelated observations and data sets. “I think the global ophthalmic community has matured to the point that we need to correlate the work we’ve done so far before we make another leap forward,” says Dr. Kanellopoulos. “We’re growing exponentially in completely different directions without finding the correlations between the different pathways we’re taking.
“At the European Society of Cataract and Refractive Surgery meeting last year our team submitted a protocol for studying different collagen cross-linking epi-on and epi-off techniques ex vivo, to try to establish some order of relative efficacy between the different techniques,” he continues. “We need a large study comparing difference fluences, techniques and riboflavin solutions. We don’t know how much we’re achieving with each one of these techniques. We’ve yet to define the actual spectrum of cross-linking’s use, titrate its effect and above all establish its safety.
“The ophthalmic community has to push the industry to conduct these studies,” he continues. “Our center is just a small, clinical investigative center, and we have no financial interest in any of the studies we’ve conducted. We conducted them purely because we saw the void and pieces of the puzzle missing from the literature. In the meantime, there are still many pieces missing from the scaffold we’re building. We need to be cross-referencing our work. What is the actual effect of each different technique?
“Once those questions have been answered, there are other horizons for cross-linking,” he notes. “Cross-linking may be a valuable adjunct or even primary treatment for infection. In the developing world, this treatment only costs a few cents, and it could save hundreds of thousands of people from blindness. In the meantime, once the United States’ clinical body of work becomes a part of cross-linking technique and technology development, I believe cross-linking will become the mainstay of ectasia stabilization, as well as a tool for biomechanically modulating corneas.”
And what about the ongoing debate regarding epi-on vs. epi-off treatment? Asked whether he thinks epi-on will eventually replace epi-off as the cross-linking procedure of choice, Dr. Rubinfeld gives a qualified yes. “If the patient just needs cross-linking to stabilize the cornea, then I think epi-on will become the standard over time,” he says. “Cross-linking is great at stopping the progression of vision loss. So, if someone comes into the office and has early keratoconus and hasn’t yet lost vision, cross-linking is the procedure for that person. In that situation, if epi-on works fine, why wouldn’t you use it? But if a patient is only correctable to 20/80 because of advanced keratoconus and irregular astigmatism, then you’ll want to try and find a way to not just stop the progression but also make the patient see better. Cross-linking alone is not very good at that, for most patients. That’s where you want to combine cross-linking with something else, such as Intacs, topography-guided ablation or standard PRK. If you’re going to do PRK, you’re going to have to remove the epithelium anyway, so in some situations, epi-off will continue to make sense.”
“The reality is, regardless of how much finesse we think we have incorporated into cross-linking, it’s currently a very gross procedure,” concludes Dr. Kanellopoulos. “We’re throwing flour and water into a pot and hoping to get the same result at the end of the day. The cornea is a living, dynamic structure; we don’t even know if the riboflavin bioavailability in the cornea is the same from patient to patient. Corneal curvature, corneal density and even keratocyte population may play a role in the efficacy of the procedure. There are so many variables in corneas from patient to patient that even though we’ve worked with cross-linking for 15 years, I personally think we’ve only scratched the surface.” REVIEW