For ocular therapies that are most often delivered topically, combination therapy development is much more nuanced than a simple mix and match. The critical issue is establishing that the combination of drugs is a demonstrably better therapy than any of the individual active ingredients. Drug regulators believe firmly in an economic version of Occam’s Razor: The most parsimonious solution, or in this case therapy, is best. Those wishing to use combinations have a high bar to clear. Yet, we all know that there are many examples of drug mixtures that are excellent medicines. This month we’ll delve into the why and how of combination drugs, focusing primarily on therapies for ocular surface conditions.
Pharmaco-matchmaking
A need for combination therapies typically stems from some limitation of existing agents. Issues such as suboptimal efficacy, short duration of action or tachyphylaxis can spawn the need for a combination approach when no single agent is available that provides a sufficient degree of therapeutic relief. Combining two or more active ingredients is about balance and synergy. When pharmacokinetic or pharmacodynamic profiles complement each other, a mixture can yield a treatment that’s superior to existing monotherapies.
In practice, combination formulations are often an attempt to address specific limitations of existing treatments. A classic example of combination therapy directed at altering drug kinetics is the insulin mixture. In these mixtures, short-acting insulin is combined with a longer-acting variant to reduce the number of injections patients need.1 The components act independently to provide a bolus of insulin followed by a prolonged duration of glucose control. In practice, many combinations have some aspect of both pharmacokinetic- and pharmacodynamic-based effects. The combinations used for ocular hypertension provide one of the best examples of this type of formulation.
Prior to the advent of prostaglandin analogs, three classes of compounds were used to lower intraocular pressure: β-adrenergic antagonists (such as timolol); α-adrenergic agonists (brimonidine); and carbonic anhydrase inhibitors such as dorzolamide.2 Each of these agents came with a set of limitations, such as application discomfort, hyperemia, cardiac effects, visual effects and tachyphylaxis. All three drug classes act by decreasing the amount of aqueous humor, yet each has a unique mechanism for achieving that outcome. β-blockers lower aqueous humor formation pharmacologically, while CA inhibitors do so enzymatically. The α-agonists are thought to act by a combination of decreased AH formation and increased uveoscleral outflow. These differences in PD allow for additive effects on IOP when used in combination. In addition, combinations can use decreased doses of each component, providing relief from some of the adverse effects of each class of compounds. For example, the combination of timolol and brimonidine had fewer adverse events than either single-agent therapy.3 The gold standard is head-to-head comparisons of efficacy: In one head-to-head study, the combination of β-blockers and α-agonists proved superior to either single agent for lowering IOP in controlled clinical trials.3 Currently, all three possible combinations of β-blockers, α-agonists and CA inhibitors are available as Food and Drug Administration-approved therapies for treatment of ocular hypertension.
The benefit of improved efficacy isn’t the only reason for combination therapies, and treatment of patients with glaucoma provides a good example of another important benefit: improved patient compliance. The single largest hurdle in compliance for these drugs is often the difficulty patients have administering drops,2,4 so combining two agents into a single drop provides a clear benefit regardless of whether the drop is for IOP, allergy or dry eye. Combination treatments are also often more comfortable than higher concentration monotherapies, further improving patients’ inclination to properly medicate.4
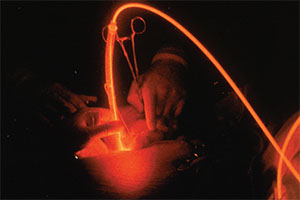 |
| Photodynamic therapy is a unique type of therapy where laser light and a photosensitizing agent are combined to target specific tissues. |
Secret Ingredients to Success
Sometimes, combination therapies involve a single active agent combined with a second, inactive compound that can impact the overall efficacy. A classic example of this is clavulanic acid, a compound without any antibiotic activity that acts as an inhibitor of bacterial β-lactamases, enzymes that can significantly reduce the effectiveness of sensitive β-lactam antibiotics.5 This compound prevents breakdown of drugs such as ampicillin, and in doing so enhances both potency and spectrum of the drug’s action. This rationale of one active agent and one “facilitator” may become more common as we gain a better understanding of the mechanisms and limitations of existing therapeutics.
Another important class of this type of combination therapy is represented by the benzoporphyrin photosensitizers, including verteporfin (Visudyne; Valeant), compounds that are used in treatment of a number of diverse diseases. By selectively targeting tissue absorption of specific wavelengths of light, these compounds have been used to apply selective laser ablation to treat skin diseases, some cancers and choroidal neovascularization. Here, the idea of a combination therapy is extended to include a combination of interventions, but again the same standard applies: The combination must be superior to either of the individual component interventions. Photodynamic therapy is an important therapeutic option in treating neovascular disease, and its value derives from the underlying combination.6,7
Combination therapies also have some significant limitations deriving from the fixed-dose formulations. Some patients may benefit from a titration of one of the actives, and for these individuals a fixed-combination product is suboptimal. In addition, fixed-dose formulation can be an issue when the pharmacokinetics of components is significantly different, especially if each active drug component is indicated to treat a different symptom. In that situation, the component with the shorter pharmacokinetic profile may tend to drive more frequent patient use, leading to accumulation of the longer-acting component and increased adverse events. In the nonprescription drug setting, there is always the concern that patients may inadvertently choose to use a combination product for symptomatic relief when they don’t need all drug components of the product. For example, consumers with conjunctivitis and nasal congestion but no pain or fever may mistakenly choose to use a product containing an antihistamine, a nasal decongestant and an analgesic/antipyretic, thus exposing themselves to acetaminophen or a nonsteroidal anti-inflammatory drug unnecessarily.
Therapies for Unmet Needs
Dry eye and chronic ocular allergy are two areas in which there’s a need for new therapies, possibly including the use of combination therapies. Both conditions are primarily treated with topical agents, and both are subject to a significant placebo effect, since artificial tears (vehicle) can provide significant, if transient, relief from the signs and symptoms of both dry eye and allergic conjunctivitis. Combinations must surmount this hurdle in addition to demonstrating superiority to each active ingredient. Combination therapies have been used for allergy relief for many years, and while there are no currently available combination treatments for dry eye, there are some indications that this may soon be changing as well.
The two predominant symptoms and signs experienced by allergic conjunctivitis patients are ocular itching and redness. Alpha adrenergic agonists were among the first compounds used topically to treat AC, and they provided modest relief of itching combined with complete or nearly complete reduction in redness.8 Topical antihistamines exhibited a reciprocal pattern, with a nearly complete relief of ocular itching combined with a modest reduction in redness.9 The combination of active ingredients from each of the two drug classes should provide almost complete relief from both itching and redness.
Combination products currently available to treat ocular allergy include two actives: an antihistamine and a vasoconstrictor. These products are all marketed as over-the-counter formulations. All contain the first-generation antihistamine pheniramine and the vasoconstrictor naphazoline.10 These products are short-acting, designed for use up to four times per day, with a duration of relief of four hours or less.8 In contrast, newer antihistamines (including both OTC and prescription drugs) have a duration of eight hours or more.9 Similarly, alternative vasoconstrictors with substantially longer durations of action than naphazoline are available.11 Even in the OTC marketplace, where patients are making many of their own treatment decisions, a number of available potential components have a long history of safety and efficacy. Combining a well-matched, extended-dose antihistamine and a longer-duration vasoconstrictor could provide a longer-acting formulation for ocular allergy. Development of longer-acting, higher-efficacy combination therapies for allergic conjunctivitis seems like an idea whose time has come.
Chronic allergic conditions are often treated with short courses of corticosteroids, and it’s possible that the combination of an antihistamine and a corticosteroid may provide relief to those with perennial ocular allergy. There have been reports of some limited success using this approach to treat chronic rhinitis.12
How might combination therapies be used to treat dry eye? As with ocular allergy, dry-eye treatments are aimed at relief of both signs (such as corneal staining or tear production) and symptoms (discomfort, burning) of dry eye. Many treatments tested as potential dry-eye therapies have shown efficacy for one of these, but not both. When the variability of patients is factored in—some patients have signs but no symptoms and vice versa—the task of getting regulatory approval seems exceedingly daunting. Despite this, one recent study tested the combination of diquafosol, a secretagogue, and hyaluronic acid, a naturally occurring lubricant.13 After three months of q.i.d. dosing, the combination was statistically superior to either component for both fluorescein staining and for symptom scores measured with the Ocular Surface Disease Index score. This result suggests that combination therapies may be an important avenue for future dry-eye treatment.
As with all drug development, the design, formulation and testing of combination therapies is rife with both pitfalls and promises. Finding the right components, designing the appropriate trials and targeting a suitable patient population all play a role in the process. Despite the difficulties, we believe that devising formulas for new combinations of therapeutics is an approach that can and will yield valuable treatment progress in the coming years. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School. Dr. Leonard-Segal is President /CEO of Segal and Furness Consulting and assistant clinical professor of Medicine at George Washington University. Dr. McLaughlin is a Senior Regulatory writer at Ora. Dr. Hollander is CMO at Ora, and assistant clinical professor of ophthalmology at UCLA’s Jules Stein Eye Institute. Dr. Abelson may be reached at MarkAbelsonMD@gmail.com.
1. Heise T, Nosek L, Klein O, et al. Insulin degludec/insulin aspart produces a dose-proportional glucose-lowering effect in subjects with type 1 diabetes. Diabetes Obes Metab 2015;17:7:659.
2. Medical Letter Treatment Guidelines, “Some drugs to treat eye disorders” M Abramowitz, ed. 2012;10:123:79-86.
3. Craven ER, Walters TR, Williams R, et al. Brimonidine and timolol fixed-combination therapy versus monotherapy: A 3-month randomized trial in patients with glaucoma or ocular hypertension. J. Ocul Pharmacol Ther 2005;21:4:337-48.
4. Higginbotham EJ. Considerations in glaucoma therapy: Fixed combinations versus their component medications. Clin Ophthal 2010;4:1-9.
5. Georgopapadakou NH. Beta-lactamase inhibitors: Evolving compounds for evolving resistance targets. Expert Opin Investig Drugs 2004;13:10:1307-18.
6. Lu HQ, Wang EQ, Zhang T, Chen YX. Photodynamic therapy and anti-vascular endothelial growth factor for acute central serous chorioretinopathy: A systematic review and meta-analysis. Eye (Lond) 2016;30:1:15-22.
7. Arevalo JF, Espinoza JV. Single-session combined photodynamic therapy with verteporfin and intravitreal anti-vascular endothelial growth factor therapy for chronic central serous chorio-retinopathy: A pilot study at 12-month follow-up. Graefes Arch Clin Exp Ophthalmol 2011;249:8:1159-66.
8. Abelson MB, Allansmith MH, Friedlander MR. Effects of topically applied ocular decongestant and antihistamine. Amer J Ophthal 1980;90:254-257.
9. Abelson MB, McLaughlin JT, Gomes PJ. Antihistamines in ocular allergy: Are they all created equal? Curr Allergy Asthma Rep 2011;11:205–211.
10. Dockhorn RJ, Duckett TG. Comparison of Naphcon-A and its components (naphazoline and pheniramine) in a provocative model of allergic conjunctivitis. Curr Eye Res 1994;13:319-324.
11. Duzman E, Warman A, Warman R. Efficacy and safety of topical oxymetazoline in treating allergic and environmental conjunctivitis. Ann Ophthalmol 1986;18:28-31.
12. Wolthers OD. New patents of fixed combinations of nasal antihistamines and corticosteroids in allergic rhinitis. Recent Pat Inflamm Allergy Drug Discov 2013;7:3:223-8.
13. Hwang HS, Sung YM, Lee WS, Kim EC. Additive Effect of preservative-free sodium hyaluronate 0.1% in treatment of dry eye syndrome with diquafosol 3% eye drops. Cornea 2014;33:9:935-41.



