While it’s interesting to drill down onto specific techniques in an article, it can also be very useful to pull back the camera to get a macro view of cataract surgery. Here, surgeons who responded to our 2022 cataract surgery technique survey share their thoughts on such topics as the best way to break up a nucleus, the ways they like to ensure postop inflammation and infection control, and how they manage astigmatism.
This year, 3,539 of the 11,366 surgeons receiving the survey opened it (31 percent open rate), and 95 completed the survey. To see how your techniques compare with theirs, read on.
Attacking the Nucleus
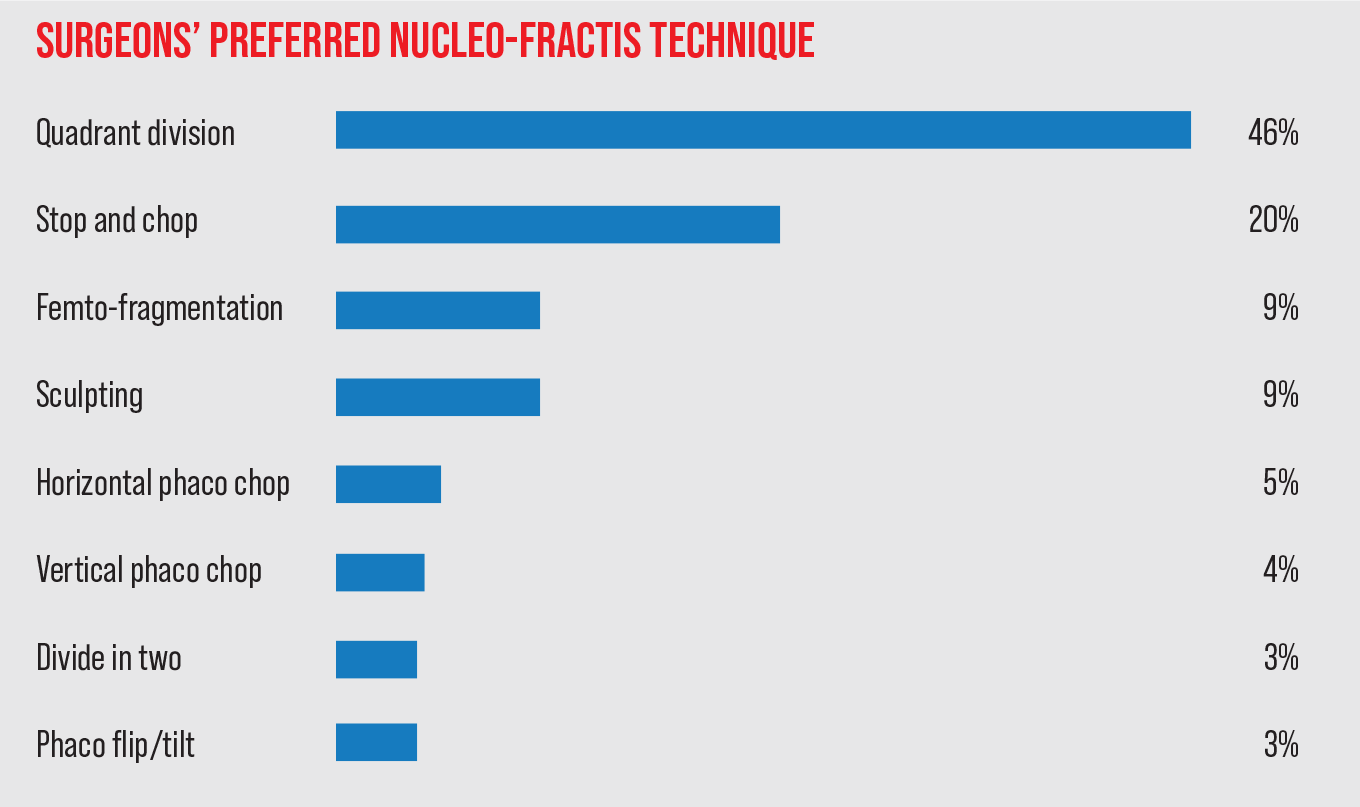 |
Continuing a trend from previous years, quadrant division is the most popular method for breaking up the cataract in this year’s survey, with 46 percent of the surgeons choosing it. The next most popular method is stop-and-chop, selected by 20 percent of respondents. These and the other options appear in the graph above.
“[Quadrant division] is the safest,” says Lawrence Shafron, MD, FACS, of Denton, Texas, “and it’s easy on the corneal endothelium.” David Chandler, MD, of Mechanics-ville, Virginia, likes quadrant division because it’s “straightforward and works most of the time, and doesn’t require a lot of manipulation or zonular stress.”
“It’s suitable for most types of cataracts,” agrees a surgeon from California.
Christopher Papp, MD, a physician in South Lyon, Michigan, echoes a sentiment expressed by several surgeons on the survey: “I was taught [quadrant division] and have become proficient in it,” he says. “I adjust the technique as needed for difficult cases.”
The surgeons in the stop-and-chop camp like the method’s predictability and the control it affords them. “Stop-and-chop gives me good control of the nuclear halves after a single groove and cracking of the nucleus, which then allows vertical chopping,” says Salt Lake City’s Nick Mamalis, MD. A Maryland ophthalmologist says he prefers the technique because it “debulks and lowers CDE compared with divide and conquer.” Aric Aldridge, MD, of Dothan, Alabama, says stop-and-chop allows “controlled division with minimal risk to the bag.”
Treating Astigmatism
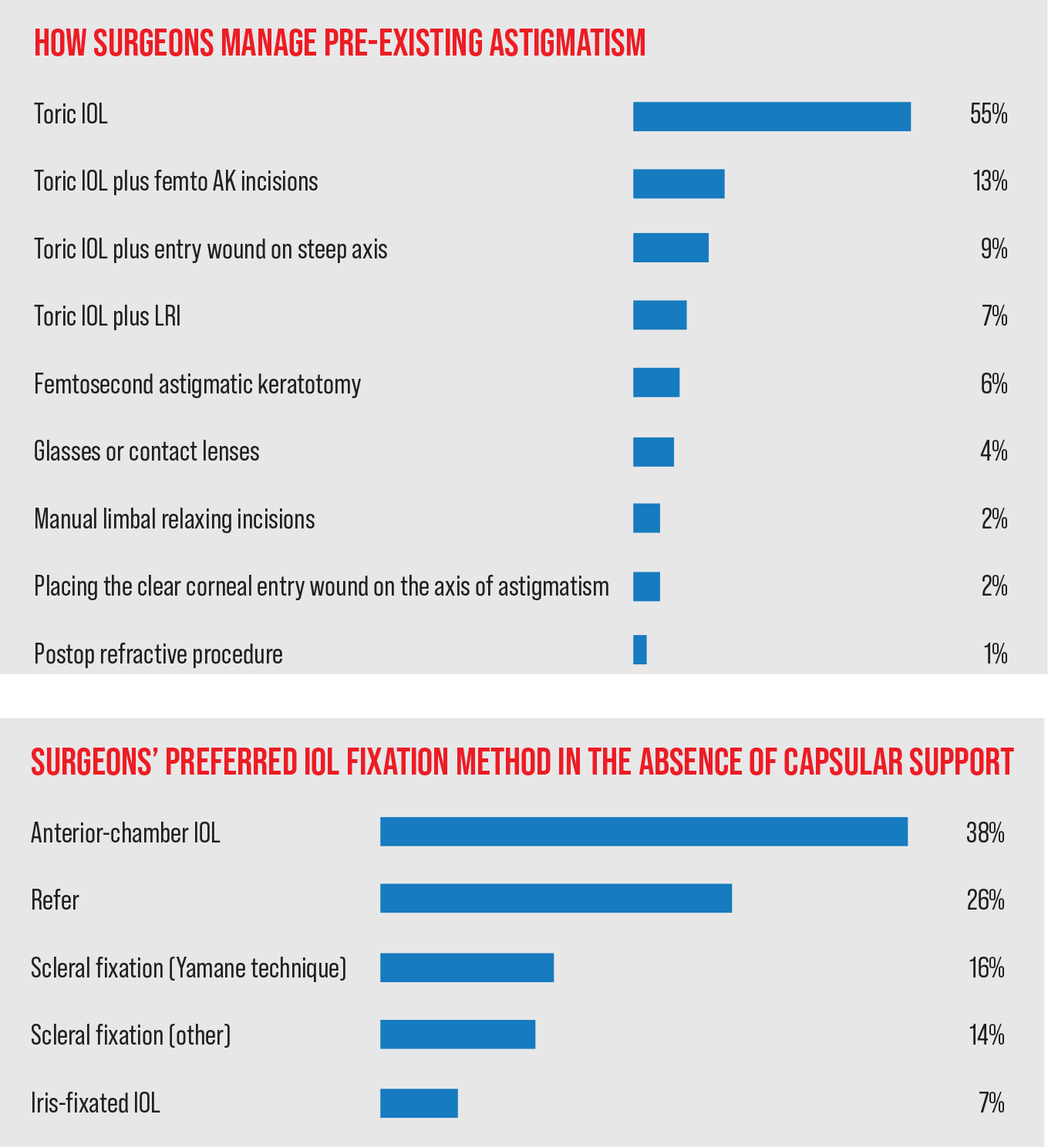 |
Surgeons also commented on their preferred approaches for managing preop astigmatism in their cataract patients.
Most of the surgeons (55 percent) say they manage patients’ astigmatism with a toric intraocular lens. The next most popular option is a toric IOL combined with femtosecond astigmatic keratotomy incisions (12.5 percent). In third is a toric lens with the entry wound on the steep axis (9.4 percent).
“Leave the cornea alone if possible,” says a Michigan surgeon who prefers using toric lenses. “However, I also do LRIs sometimes. Also use glasses if patient doesn’t want to spend the extra money for a toric.” St. Louis’ Bruce H. Cohen, MD, feels similarly, saying, “This is effective and far more predictable than LRI by manual or femto.”
“Toric IOLs are more precise now [thanks to] the newer formulas,” says a surgeon from North Carolina, “and LRIs’ effects regress over time.”
The surgeons who like IOLs combined with femtosecond cuts believe they’ve got the best of both worlds.
“Using AK for lower cylinder and a toric lens for higher cylinder is the most reproducible and consistent approach,” says Asim Piracha, MD, of Louisville, Kentucky. A surgeon from Georgia agrees, saying, “This gives the most accurate results.”
“It gives more repeatable outcomes,” says Dee Stephenson, MD, of Venice, Florida.
Alternative IOL Fixation
When an eye’s capsular support is lacking, surgeons have various methods they turn to in order to fixate the IOL securely and close the case. On this year’s survey, the most popular option is to implant an anterior-chamber IOL (38 percent). A close second is a sclerally-fixated lens (with or without using the Yamane technique) at 30 percent (16 percent of these surgeons say they prefer to use the Yamane). Twenty-six percent of surgeons say they’ll refer such a patient.
[An anterior-chamber fixated IOL] is quicker and easier,” says a surgeon from Texas.
“If there’s no glaucoma, an AC-IOL works well,” avers Jonathan Adler, MD, of Bradenton, Florida. “If a patient has glaucoma, then I’ll go with Yamane scleral fixation.”
Several surgeons say they’re simply more comfortable with an AC-IOL because of their training and background. “I’m not skilled in the other methods,” says Michael Loeffler, MD, of Lighthouse Point, Florida. A surgeon from Virginia feels the same, saying, “I’ve got insufficient experience in suturing them.”
“An AC-IOL is less prone to complications when done correctly,” a surgeon from California says.
Several surgeons, however, prefer the Yamane technique. “I like the aesthetics of it,” says Lancaster, Pennsylvania, surgeon Spage Yee, MD.
“It has the least pseudophakodonesis away from uveal tissue (hence a quieter eye),” says a surgeon from Florida.
“I prefer to use a modified Yamane using 27G ports ...” says another scleral suture fan. “An anterior chamber intraocular lens in older patients is also perfectly good solution.”
In the non-Yamane scleral-fixation camp, surgeons like the approach’s “good centration and stability,” according to Los Angeles surgeon Michael Colvard.
A cataract surgeon from New Jersey likes the method’s staying power in the eye. “9-0 prolene doesn’t fracture even after 20 years,” she says.
Tech Choices
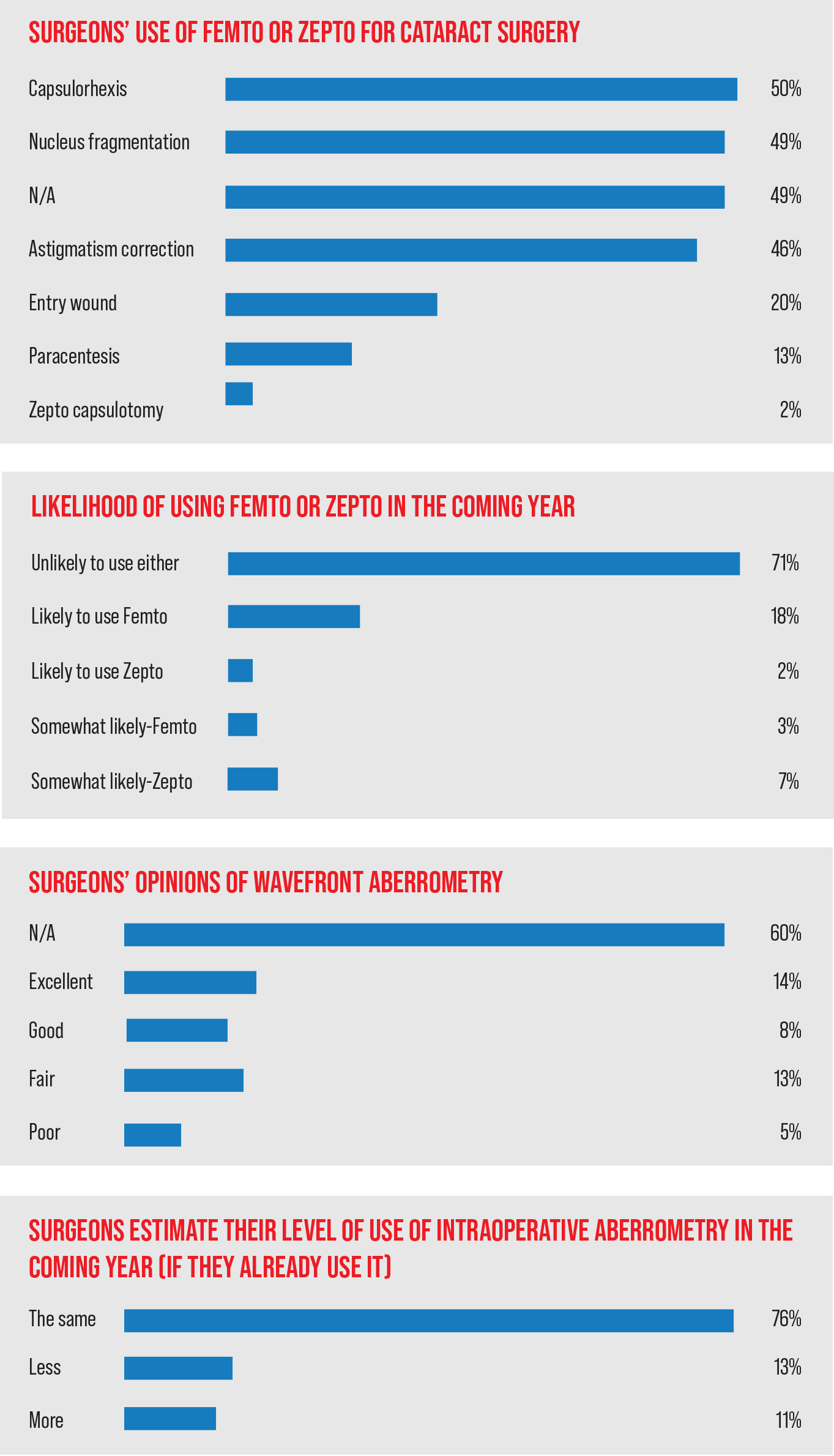 |
Two of the high-tech devices available to surgeons for a while have been the femtosecond laser for use in cataract surgery and the intraoperative aberrometer. Surgeons on the survey appear to use the former somewhat more than the latter, however.
• Femtosecond laser-assisted cataract surgery. Fifty-one percent of the surgeons say they use the femto for some aspect of cataract surgery. The most popular use is for the creation of the capsulhorhexis (50 percent of FLACS users), followed by nucleus fragmentation (49 percent) and astigmatism correction (46 percent) (surgeons could choose more than one response). The full list of the uses and their percentages appears in the graph to the left.
“The femtosecond laser produces excellent, reproducible results,” says a surgeon from Atlanta. “It’s more precise, and makes surgery easier.” Dr. Piracha sees pros and cons to the laser. “I like the perfect capsulorhexis and fragmentation,” he says. “The AKs aren’t perfect, however, due to alignment and measurement issues.”
“I like the femto for its decrease in phaco power required for dense lenses, the precision of placing toric IOLs when combined with Cassini for iris registration, and for a perfect capsulorhexis, particularly for multifocal IOLs,” states a surgeon from Virginia. Another surgeon agrees, saying the use of the femtosecond results in “less ultrasound and less endothelial damage in shallow chambers.”
Taking a slightly different technological path, Ronald Wise, MD, of Denver uses the Zepto capsulotomy device. He says he appreciates the “round, central rhexis” it creates.
In terms of the surgeons’ FLACS volumes, a fifth of the surgeons say they’re volumes are increasing, 7 percent say they’re decreasing, and a quarter of the surgeons say they’re staying the same.
Looking ahead at FLACS’/Zepto’s future uptake, 71 percent of the respondents who don’t currently use the technology say they’re unlikely to use either of them. Eighteen percent say they’re likely and 3 percent are somewhat likely to use the femtosecond. Two percent are likely and 7 percent are just somewhat likely to try the Zepto.
Surgeons lay out the reasons they’re not interested: “Cost, availability, and [the fact that I] could do the steps by hand that the laser can do,” says a surgeon from Washington, D.C.
“I don’t need it, and haven’t seen any data suggesting improved outcomes,” opines a Michigan surgeon.
“This is great technology that solves no problem we were having previously,” says a surgeon from Ohio. An ophthalmologist from Oklahoma agrees, saying, “We have a very quick, successful, easy method already.”
Another surgeon, from Florida, says he’s somewhat likely to try the technology. “I would somewhat like either in certain instances,” he says. One surgeon says he’s interested in the Zepto, but hasn’t had any experience with it yet.
 |
• Intraoperative aberrometry. Sixty percent of the respondents don’t use intraoperative aberrometry. Of the surgeons who do use it, 14 percent think it’s excellent, 8 percent would call it good, 13 percent think it’s fair, and 5 percent think it’s poor.
“I’ve been using it for 10 years,” says Florida’s Dr. Stephenson. “It improves my outcomes.” Frank Burns, MD, of Louisville, Kentucky, agrees. “It helps with most IOL powers in post-refractive patients (post-LASIK, post-PRK and post-RK), and also helps with toric IOL alignment,” he says. San Diego’s Steven Fish, MD, can see the benefit, but only in certain spots. “It’s helpful post-refractive surgery,” he says. “Otherwise, modern formulas do a good job at predicting outcomes, so I rarely use it.”
“It’s stressful when it doesn’t agree [with your calculations], says a surgeon from Maryland. “Lots of variables can affect the reading intraoperatively.”
A surgeon from Tennessee has cooled on the technology. “I used to use it, but with improved preop biometry and formulas, it’s not necessary anymore,” she says.
Other Techniques
Surgeons also commented on specific technique/technologies as well as gave their best pearls for cataracts.
• Pupil management during surgery. Fifty-two percent of the respondents use intracameral epinephrine/lidocaine injection (“Epi-Shugarcaine”) to help promote a wide pupil during surgery. Nineteen percent use mechanical pupillary dilation, usually via a Malyugin ring, and 17 percent use Omidria (an injection of phenylephrine/ketorolac from Omeros).
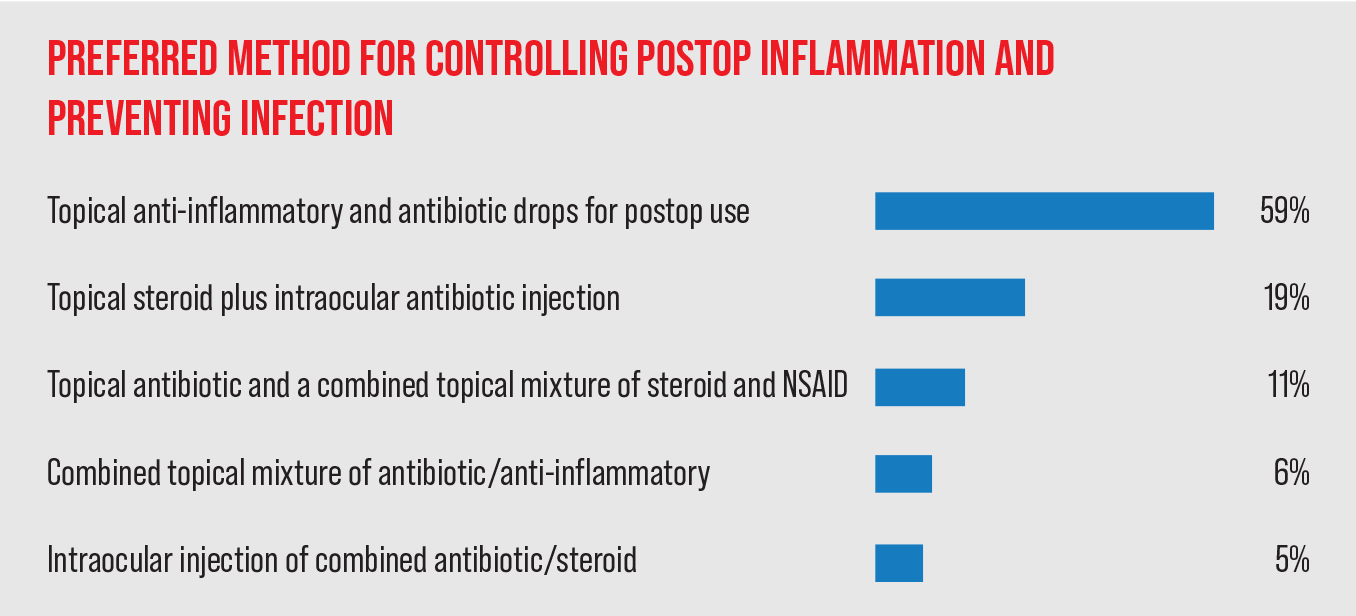
• Postop inflammation management/infection prevention. Most surgeons (59 percent) still prescribe topical anti-inflammatory and antibiotics for postop use. Nineteen percent prescribe topical steroids but give the antibiotics via an injection, and 11 percent prescribe a topical antibiotic and a topical combination of a steroid and an NSAID.
• Surgeons’ pearls. The surgeons were also asked to give their single best piece of surgical advice. Here are some of the answers:
— “Use of good, old-fashioned immersion A Scan and keratometry can still give you great results. Just use the appropriate IOL calculation.” (Lancaster’s Dr. Lee)
— “Treat dry eye and astigmatism.” (Dr. Stephenson)
— “Always have a Plan B and, for complicated cases, a Plan C. Though rare, if things don’t go to plan, it is usually better to take the time to assess the situation, ensure a safe outcome, and a happy ending ... even if it means a longer surgery or a slower recovery. If you’re asking yourself the question [about a possible complicating factor], then place that CTR and stain with triamcinolone to check for vitreous. Always be assessing and re-assessing.” (Jimmy Y. Hu, MD, of Manhattan)
— “Hydrodisect well. Make sure the nucleus is rotating well and make a round, 5-mm capsulorhexis that overlaps the implant.” (Bradenton’s Dr. Adler)
— “Drop your wrist, flatten your I/A tip and rotate the eye toward you for subincisional cortex removal.” (Anonymous)
— “Use a Malyugin ring in small pupil IFIS.” (Denver’s Dr. Wise)
— “Every step builds on the previous step. Be precise and efficient.” (St. Louis’ Dr. Cohen)
— “Treat every patient like your mother.” (David G. Gross, MD, Merrillville, Indiana).