Using a national database, researchers identified individuals with bevacizumab-treated AMD with diagnosis of MI prior to the first bevacizumab injection (delivered between September 2008 and October 2014 [n=2,100]). They then generated sub-groups treated within three months (n=11), six months (n=24), 12 months (n=52) and 24 months (n=124) after MI. Researchers compared those individuals to age- and gender-matched members who had MI at the same time but were never exposed to anti-VEGF. They performed a survival analysis using propensity score-adjusted Cox regression.
Bevacizumab-treated individuals were slightly and insignificantly older than controls (mean age, 83.25 vs. 83.19 year; p=0.75). Gender distribution was similar. Researchers reported increased mortality rates associated with the use of intravitreal bevacizumab in AMD cases after MI, compared with age- and gender-matched post-MI cases with no exposure to anti-VEGF agents. Researchers found the following differences in mortality:
• within three months between MI and initiation of bevacizumab treatment, OR=6.22 (CI, 1.08 to 35.97, p<0.05);
• within six months, OR=2.37 (CI, 0.93 to 6.02, p=0.071);
• within 12 months, OR=3 (CI, 1.44 to 6.28, p<0.01);
• within 24 months after MI, OR=2.24 (CI, 1.35 to 3.70, p<0.01); and
• MI any time prior to first bevacizumab injection, OR=1.71 (CI, 1.53 to 1.92, p<0.001).
They advised that caution should be taken when offering bevacizumab to individuals with AMD after MI.
Graefes Arch Clin Exp Ophthalmol 2018; Feb. 10. [Epub ahead of print].
Hanhart J, Comaneshter DS, Freier-Dror Y, et al.
Ultrasonography Assessment of Optic Nerve Sheath Diameter
Investigators wrote that the standard method for monitoring intracranial pressure can result in complications and pain, making noninvasive, repeatable methods a valuable option. They examined how ultrasonographic optic nerve sheath diameter correlated with noninvasive and dynamically monitored ICP changes.
Investigators measured the ONSD before lumbar puncture in 60 individuals on admission. Those with elevated ICP were divided into group one (200 < LP ≤ 300 mmH2O) and group two (LP > 300 mmH2O). Individuals underwent follow-up ONSD and LP measurements within one month. Investigators analyzed correlations between the ONSD and ICP on admission, and between changes in ONSD and ICP, i.e., respective changes in ONSD and ICP from admissions to follow-up.
Main outcomes and measures included the ultrasonographic ONSD and ICP measured at admission and follow-up, correlations between ONSD and ICP on admission, and changes in ONSD and ICP using Pearson correlation analyses.
Investigators reported that for 60 individuals (mean age 36.2 ±12.04 years; 29 [48 percent] female) at admission (group one), ONSD and ICP values were strongly correlated, with an r of 0.798 (CI, 0.709 to 0.867; p<0.001).
For 25 individuals with elevated ICP who completed the follow-up (group two):
• upon admission, the mean ONSD was 4.50 ±0.54 mm, and mean ICP was 302.40 ±54.26 mm H2O;
• upon admission, ONSD and ICP values obtained were strongly correlated with an r of 0.724 (CI, 0.470 to 0.876; p<0.001);
• the mean change in ICP was 126.64 ±52.51 mm H2O (range: 20 to 210 mm H2O) (CI, 106.24 to 146.07), and in ONSD was 1 ±0.512 mm (range: 0.418 to 2.37 mm) (CI, 0.83 to 1.20); and
• the change in ONSD was strongly correlated with that in ICP, with an r of 0.702 (CI, 0.425 to 0.870; p<0.001).
Follow-up evaluations revealed that elevated ICP and dilated optic nerve sheath diameters returned to normal, and no evidence of difference was found in the mean ONSDs between group one (3.49 mm; CI, 3.34 to 3.62 mm) and group two (3.51 mm; CI, 3.44 to 3.59 mm) (p=0.778) at follow-up.
Investigators found that the dilated ONSDs decreased along with the elevated ICP reduction. They concluded that ultrasonographic ONSD measurements may be a useful, noninvasive tool for dynamically evaluating ICP.
JAMA Ophthalmol 2018;Feb. 1 [Epub ahead of print].
Wang LJ, Chen LM, Chen Y, et al.
Trabeculectomy with MMC in Angle-closure Patients
Researchers from the University of California-Los Angeles’ Jules Stein Eye Institute say that, because there had never been a large study of trabeculectomy with the use of adjunctive mitomycin-C in patients suffering from primary angle-closure glaucoma, they undertook a study looking at the long-term tonometric results in these cases.
In a retrospective cohort study, the investigators used three criteria to judge the success of the procedure, with or without adjunctive drugs: intraocul
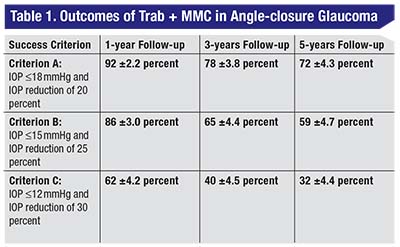 |
The qualified success rates of the surgery appear in Table 1.
The study also identified risk factors for failure of the procedure. The researchers say that eyes that had their crystalline lenses before their trabeculectomy procedure had a higher rate of failure for all criteria (hazard ratio of 1.9 for criterion A; HR of 2.9 for criterion B; HR of 3.6 for criterion C). A family history of glaucoma was associated with a higher rate of failure with criterion A (HR: 2.8). Eyes with no previous laser peripheral iridotomy had a higher risk of failure when criteria B and C were used to judge success (HR for both: 2.5). Worse baseline intraocular pressure was a risk factor for failure with criterion C (HR: 1.1).
Ultimately, the researchers say that trabeculectomy combined with MMC effectively reduces IOP in PACG, achieving long-term IOP levels in the mid-teens.
J Glaucoma 2018;27:2:101-107.
Romero P, Hirunpatravong P, Alizadeh R, et al.
Outcomes of Cataract Surgery In Epiretinal Membrane Cases
A team of researchers from different countries explored the outcomes of cataract surgery performed in patients with primary epiretinal membranes.
In a retrospective clinical database study, the investigators collected data from July 2003 to March 2015 from eight centers in the United Kingdom. They drew cataract surgery data from 217,557 eyes from the electronic medical record of the UK National Health Service. After excluding 57,561 eyes that had combined surgery, prior vitrectomy, co-pathology and/or complications, the researchers analyzed 812 eyes with primary ERM and 159,184 reference eyes. In the study, the primary outcome measures were visual acuity, the incidence of cystoid macular edema and the need for ERM surgery.
Epiretinal membrane eyes assessed at four to 12 weeks postoperatively gained 0.27 (0.32) logMAR (approximately three Snellen lines), with 200 of 448 (44.6 percent) improving by 0.30 logMAR or more (≥3 lines) and 32 of 448 (7.1 percent) worsening by 0.30 logMAR or more. The reference eyes’ vision gained a mean of 0.44 ±0.26 logMAR (approximately four Snellen lines), with 48,583 of 77,408 (62.8 percent) improving by 0.30 logMAR or more and 2,125 of 77,408 (2.7 percent) worsening by 0.30 logMAR or more. Although all eyes with preoperative VA of 20/40 or less improved, only reference eyes with preoperative visual acuity of better than 20/40 showed improvement.
Cystoid macular edema developed in 57 of 663 eyes that had epiretinal membranes (8.6 percent) (95% CI, 6.69-10.98) and 1,731 of 125,435 reference eyes (1.38 percent) (95% CI, 1.32-1.45) (p< 0.001). Epiretinal membrane surgery was performed in 43 of 663 of the eyes with membranes (6.5 percent).
JAMA Ophthalmol 2018;136:2:148-154.
Romero P, Hirunpatravong P, Alizadeh R, et al.
Replacing a Failed Ahmed Valve with a Baerveldt
Investigators analyzed outcomes in eyes that underwent surgery to replace a failed Ahmed valve with a Baerveldt glaucoma implant in the same quadrant, as part of a retrospective case series of nine glaucoma patients.
The parameters analyzed in the study included age, glaucoma type, prior surgery, complications, intraocular pressure, visual acuity, and number of glaucoma medications before and after the surgery. Surgical success was defined as an IOP measurement below 21 mmHg or a 20 percent IOP reduction, with or without a hypotensive agent.
The mean follow-up duration in the study was 47 months. After surgery, at the time of final follow-up, the mean IOP decreased from 29.9 to 16.7 mmHg (36 percent of mean IOP reduction, p=0.008). Investigators found a significant reduction of hypotensive agents, from a mean of 4.33 to 2.22 (p=0.02). Visual acuity didn’t show a significant deterioration (p=0.07). In the final office visit, five of nine individuals met the success criteria and two individuals were qualified successes. Two cases failed after 69 and 125 months of follow-up, respectively. The cumulative probability of success after six months was 76 percent, and this rate remained stable until the sixth year. One individual developed bullous keratopathy. Two individuals had early postoperative pressure spikes: The first individual was treated by trabeculectomy and the second underwent a vitrectomy.
Investigators suggested that replacing a failed Ahmed glaucoma valve with a new Baerveldt glaucoma implant in the same quadrant could be a reasonable choice to control refractory glaucoma.
J Glaucoma 2018; Feb.16. [Epub ahead of print].
Zuo W, Lesk MR.




