Epithelial basement membrane dystrophy is estimated to affect approximately 2 percent of the population, establishing it as the most common corneal dystrophy.1 Perhaps because of its high incidence rate, EBMD is relatively recognizable, and ophthalmologists have found reliable treatment methods. However, there’s always the chance of something unexpected happening, so we spoke with cornea experts about the standards of care for EBMD and why you should remember to approach each case individually.
Recognizing EBMD
One of the first things to know about EBMD is that it can have more than one name, yet they all represent the same condition, says Gerami Seitzman, MD, an associate professor of ophthalmology at the University of California, San Francisco.
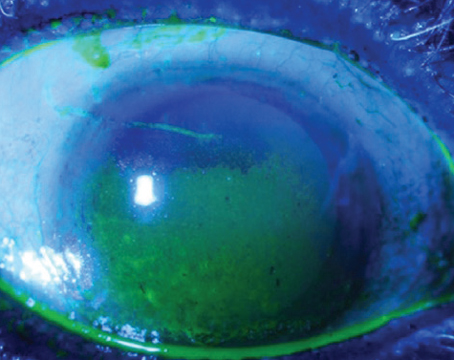
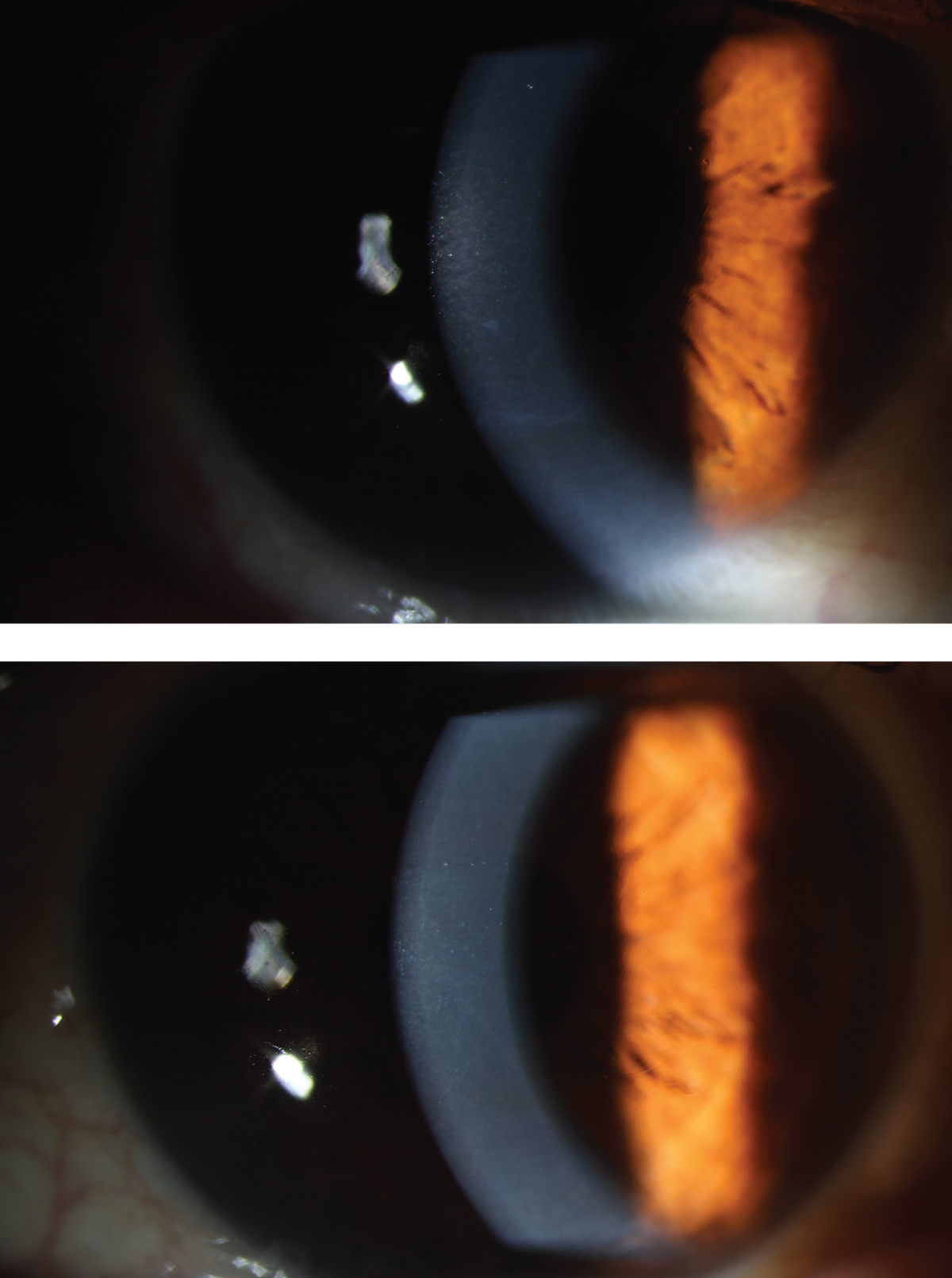 |
| Under slit lamp examination, the textbook presentation of EBMD is the descriptive map-dot-fingerprint dystrophy. Here, you can see a central “dot” (top) with an inferior “map line,” and central “map/fingerprint lines” (bottom). Photo: Angela Zhu, MD. |
“In addition to those who abbreviate it as EBMD, others refer to it as corneal anterior basement membrane dystrophy, or ABMD. Often, it’s referred to by its descriptive sign from the slit lamp: map-dot-fingerprint dystrophy; and if the prominent component of the examination are the dots of the map-dot-fingerprint dystrophy—it would be almost like a dot dystrophy—that’s called Cogan’s microcystic epithelial dystrophy. They all mean the same thing,” Dr. Seitzman says.
“When we’re talking about this dystrophy that has all of these names, we’re talking about a disorder of the attachment of the corneal epithelium to the underlying structures,” she continues.
It can occur for a number of reasons, whether idiopathic or sporadic, and occasionally there’s a genetic cause, Dr. Seitzman says. “The bottom line is, we don’t truly understand the mechanism of why it develops, but interestingly, the findings of EBMD are common in the general population. The estimates vary, but with careful observation at the slit lamp, it really is present in many people.”
In fact, a thorough slit lamp exam is one of the most valuable steps in identifying EBMD. “A lot of people sort of rush at the slit lamp. They don’t take the time to see it, because there are some little special tricks of lighting, such as indirect illumination, that often highlight the epithelial abnormality best,” continues Dr. Seitzman.
The good news is that the vast majority of people are totally asymptomatic, and no treatment is needed, she says. But this can be tricky when it comes to cataract or refractive candidates.
Angela Zhu, MD, who practices at the Bascom Palmer Eye Institute in Miami, says screening for EBMD is important for anyone undergoing refractive surgery. “Patients are going in expecting perfect visual outcomes, but because the pathology in this disease is that the epithelium doesn’t attach as well in the areas that are affected, or to the basement membrane, a procedure such as LASIK can actually worsen the condition,” she says. “We see patients come in after LASIK surgery with previously undiagnosed EBMD who are now experiencing severe recurrent corneal erosions, severe pain, and ongoing symptoms which can obviously affect their vision and become a problem.”
Calculations for cataract surgery may also be affected, Dr. Zhu continues. “EBMD can affect the regularity of the surface of the cornea, so the power calculations for the IOL implants may not be as accurate. Or, patients may still have other distortions in their vision afterwards, and they’re unhappy after surgery.”
For those who do experience symptoms, decreased vision isn’t the most common problem. Instead, the most common and most painful symptom of EBMD is recurrent corneal erosions.
“This happens because the eyelids get hold of these tiny irregular ridges from the irregular attachment of the epithelium to the underlying cornea. The eyelid can hook onto these areas of corneal epithelial irregularity and scratch the cornea,” says Dr. Seitzman. “Any defect in its outer layer causes a tremendous amount of pain and tearing. Classically, recurrent erosion syndrome occurs in the morning. Though it can occur at any time of the day, typically, when your eyelids have been closed for the whole night, that leads to more opportunity for the eyelid to stick to these ridges. So, the classic symptom is that the patient says: ‘When I wake up in the morning, it feels like my eyelids are stuck to my eyeballs, and when I force them open I feel terrible pain and have a ton of tearing.’ ”
Dr. Seitzman notes that these open defects can put patients at risk for corneal ulcers if the tear is infected.
“[In patients with vision complaints] there are ridges and whorls and dots over the patient’s pupil. They don’t have pain at all, but they have blurred vision because, instead of light coming into the pupil in a perfect straight line to the back of the eye to be registered as sight, these little ridges and dots can induce irregular astigmatism,” says Dr. Seitzman. “These irregular areas of epithelial attachment over their pupil can register as blurry vision or shadow vision or little halos when they’re looking straight ahead at an object.”
Other subtle early signs may be similar to dry eye, meibomian gland dysfunction or blepharitis, Dr. Zhu adds.
How to Treat EBMD
According to Dr. Zhu, EBMD is one disease where there haven’t been too many notable advances in treatment, for good reason. “The treatments that have been established actually work very well,” she says.
She says EBMD treatment is a stepwise approach. “If the patient is rarely symptomatic, maybe one or two episodes a year or just a very rare kind of symptomatology in terms of the recurrent dry eye, then we may just treat it with recurrent lubrication and preventative measures,” she says.
Dr. Seitzman says patients can use a thick ointment on the inside of their eyelids before bed at night, which forms a mechanical barrier between the corneal epithelial layer and the eyelid. “Some patients use this ointment for the rest of their lives or for a prolonged period of time and they’re fine,” she says.
There’s some debate whether the ointment or similar lubricating drops should have salt in them, Dr. Seitzman continues. “The most common over-the-counter ointment is Muro, which is 5% sodium chloride. Some people think using this dehydrates the skin, allowing it to adhere better to the cornea,” she says. “However, we don’t have definitive large, randomized, control trials to show that any recurrent erosion treatment is better than another. Often what happens is the treatment has to be tailored to the individual patient and their unique presentation.”
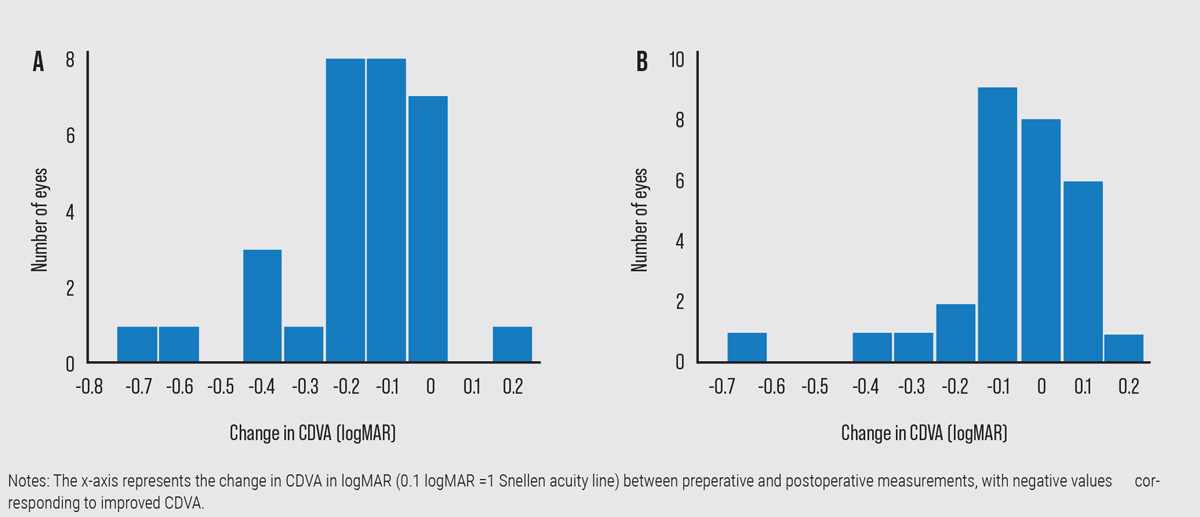 |
| Figure 1. Patients treated with PTK for visual disturbances (Graph A), had a mean final postop CDVA of ~20/25, with 14 eyes gaining ≥2 lines of visual acuity. Those who underwent PTK for painful recurrent erosions (Graph B) had a mean final postop CDVA of ~20/20.1 |
It may also be wise to include a steroid and oral doxycycline, Dr. Seitzman says. “When you have recurrent erosion on the cornea, the ocular surface becomes quite inflamed. That becomes a cycle of further erosion, meaning when you have high levels of inflammatory proteins and cytokines in the tear film, that further disrupts the attachment of the epithelium to the underlying corneal tissue,” she says. “So not only do the corneal erosions themselves become inflammatory, but if you have other external disease conditions, commonly blepharitis or allergic conjunctivitis, and you already have an inflammatory ocular surface, the combination of all of this inflammation really inhibits epithelial adhesion.”
A retrospective single-observer case study published in 2008 looked at 21 patients with recurrent corneal erosion syndrome who were treated with 50 mg oral doxycycline twice a day, and topical fluorometholone 0.1% three times daily for a minimum of four weeks. At eight weeks, 15 were symptom free and all but one patient reported improvement in symptoms.2
“It’s very common as a medical therapy that we place patients on a steroid drop and oral doxycycline,” says Dr. Seitzman. “That combination is quite anti-inflammatory for the ocular surface. With medical therapy alone, many patients can have improved comfort without needing surgery.”
If topical treatments aren’t successful, it’s time to explore surgical treatment, of which there are various options.
“In general, a surgical treatment requires removal of the loose corneal epithelium and some procedure where the underlying tissue is roughened a bit,” Dr. Setizman says. “This roughening can cause micro scar tissues, and scarring promotes adhesion.”
There are two routes to go: either superficial keratectomy or phototherapeutic keratectomy. Both have been shown to have similar outcomes, perhaps making the decision a matter of personal surgeon preference. A 2002 study comparing PTK to SK with a diamond burr showed no statistically significant difference in symptoms returning or BCVA. However, the study authors hypothesized that diamond burr treatment may have an advantage, due to it being simpler and less expensive.3
Dr. Zhu says it can often come down to ease of scheduling. “I think it can depend on your practice, where you’re located in the United States, and what’s covered by insurance,” she says. “So the ability to send patients to a minor procedure room in your office where you essentially scrape the epithelium or go an extra step and do an anterior stromal puncture or diamond burr polish to roughen it up a bit may be preferable.” After the procedure, a bandage contact lens is placed over the eye to promote adherence of the cornea without the lid disrupting the growth of the new corneal epithelium.
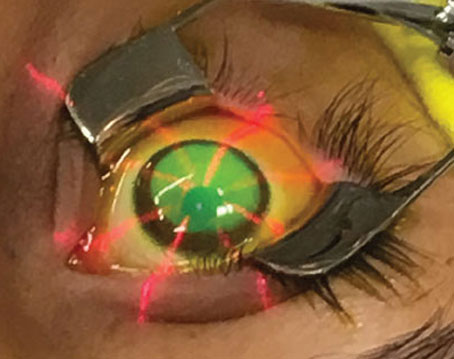
“The last type of surgical treatment is PTK, which is a very superficial excimer ablation of the top layer of the cornea, which promotes these micro scars from the laser essentially, and roughens up that area,” Dr. Seitzman says. “It can only be done in the central cornea, usually within the central 8 or 9 mm of the cornea.”
“Again, this is a little bit surgeon-preference and insurance dependent,” emphasizes Dr. Zhu. “Each approach has its own individual risks, but I think in general, most of us prefer starting with epithelial debridement and anterior stromal puncture and diamond burr polish. Then, if there are recurrent cases, we move to PTK. Sometimes, if it’s in the very central visual axis, or if we’re already planning another refractive surgery procedure, or if there’s also prolonged haze in that area that’s already causing scarring, that’s when I would jump to PTK first.”
As previously mentioned, undiagnosed EBMD could pose a challenge for cataract and refractive surgery. If a LASIK candidate is found to have asymptomatic EBMD, Dr. Zhu recommends considering PRK instead. “With PRK, you debride the epithelium, which is one of the fundamentals of treating this disease, so it offers a better alternative,” she says. “If surgeons just consider a slight change in their planning, it can essentially still lead to good outcomes and simultaneously treat this disease.”
Both Dr. Seitzman and Dr. Zhu say it’s important to address each case individually. “Even though the literature shows good efficacy for these treatments, there are also cases where it doesn’t work for some patients, and it’s hard to say which ones it will or won’t work for,” says Dr. Zhu.
“Some patients do really well with just one of the treatments that we discussed, while some patients actually have to cycle through more than one,” Dr. Seitzman says. “As with many eye conditions, it’s really hard to create a general rule for patients who have other diseases. For example, in ocular rosacea or atopic eye disease where there’s a lot of inflammation, that inflammatory ocular surface can promote more erosion. If one treatment doesn’t work, we can use another, and many times we use many at the same time. So, if it’s a very severe case, we may be talking about a surgical procedure but, at the same time, we’re also treating it with steroids and doxycycline, and all of these procedures can be repeated.”
Final Considerations
Dr. Zhu thinks general practitioners should keep EBMD on their differential.
“If patients say they’re always waking up feeling like their eyes are more dry, or every once in a while they wake up with significant pain, or they still feel like their vision isn’t quite that sharp all the time after refractive or cataract surgery, it’s worth taking another look and seeing if this underlying condition is actually causing their problems,” says Dr. Zhu. “Sometimes it’s easy to forget about EBMD because the signs can be very subtle, especially in the setting of the more common day-to-day dry eye, meibomian gland dysfunction and blepharitis type of issues.”
It’s also important not to confuse EBMD with other disorders or diseases, says Dr. Seitzman.
“The corneal epithelium can only heal properly if there’s adequate corneal sensation,” she says. “Sometimes, a non-healing corneal defect can be misattributed to EBMD when the underlying disorder is actually neurotrophic keratopathy. EBMD often occurs with neurotrophic keratopathy, and that gets a little trickier to heal because you really do need corneal sensation to promote adequate corneal healing.”
The pattern of healing could even be mistaken for herpes keratitis, continues Dr. Seitzman. “When you have an erosion in a patient with EBMD and the skin is healing, it heals in a funny/irregular pattern that can sometimes appear linear, and can also sometimes be misdiagnosed as herpes, because we associate herpes infections with linear shapes on the cornea. Sometimes, however, a healing EBMD erosion can heal in a linear pattern and mimic HSV keratitis.”
Dr. Seitzman is a consultant for Dompé Pharmaceuticals. Dr. Zhu is a consultant for Santen Therapeutics and an advisor for Eliksa Therapeutics.
1. Lee WS, Lam CK, Manche EE. Phototherapeutic keratectomy for epithelial basement membrane dystrophy. Clin Ophthalmol 2016;16:11:15-22.
2. Wang L, Tsang H, Coroneo M. Treatment of recurrent corneal erosion syndrome using the combination of oral doxycycline and topical corticosteroid. Clin Exp Ophthalmol 2008;36:1:8-12.
3. Sridhar MS, Rapuano CJ, Cosar CB, Cohen EJ, Laibson PR. Phototherapeutic keratectomy versus diamond burr polishing of Bowman’s membrane in the treatment of recurrent corneal erosions associated with anterior basement membrane dystrophy. Ophthalmology 2002;109:4:674-9.