Recently, the Foundation for the National Institutes of Health, hoping to harmonize the process of biomarker selection among the Food and Drug Administration, NIH, industry, academia and patient groups, released a report outlining the appropriate use of biomarkers in medical research and therapeutic development.1 Biomarkers are defined as any measure, from a blood test or biopsy to an imaging modality, that can be used to assess a physiological state. Often these provide a more quantifiable, rapid and cost-effective means of assessing disease modification but, in general, the FDA has resisted their use as primary tools in therapeutic approvals. This month, we consider how the evolution of technology has and will impact ophthalmic therapies going forward.
Biomarker Basics
The classic example of a biomarker is blood pressure: an easily measured biometric that provides direct information on the status of that aspect of a patient’s cardiovascular function and an indirect assessment of multiple organ systems. Like most biomarkers, using BP as a measure of patient health comes with a significant caveat: While reduction of elevated BP is associated with an improvement in patient health, the effect doesn’t mean the underlying cause has been addressed. In ophthalmology, elevated intraocular pressure presents a similar example of a biomarker with an unequivocal association with disease. In these cases, IOP-lowering drugs have been approved based solely on their ability to “treat the biomarker,” knowing that, while providing a beneficial effect, they may not fully prevent further damage of the optic nerve. Treatment of IOP in combination with monitoring other risk factors and metrics is likely to provide the best window on glaucomatous progression.2-4 Despite improvements in retinal imaging, intraocular pressure remains the only surrogate measure used by the FDA as the basis of approval for treatments for glaucoma, though the specific indication for topical glaucoma products most commonly reads, “For the reduction of elevated IOP in subjects with primary open angle glaucoma or ocular hypertension,” as opposed to, “For the treatment of glaucoma.”
In fact, BP and IOP are outliers in that they are the rare examples of biomarkers that are used as a basis for a therapeutic approval. More often, a direct effect on a disease state is required. For example, drug therapy for post-menopausal osteoporosis can be easily followed by radiographic measures of bone mineral density, but approvals have required demonstration of a clinically significant reduced risk of fracture. This example highlights the distinction made in Dr. Osler’s quote, and is the standard by which most drug approvals occur. Despite this, biomarkers can provide invaluable information in the course of diagnosis, and are keys to drug development programs even when they are not used as primary endpoints.
Surrogate biomarkers, used as diagnostic tests, are the stalwarts of medical diagnosis. For example, blood
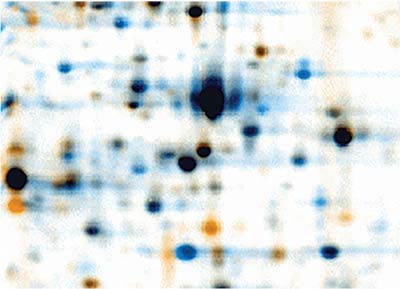 |
| Two-dimensional electrophoresis remains a valuable tool for identifying changes in tear fluid composition. Staining shows the separation of hundreds of different components that can be identified by subsequent mass spectroscopy. |
Biomarkers, Front to Back
The composition and relative concentrations of tear-fluid components provide insights into a number of ocular conditions, especially those involving innate immune defense responses to ocular surface pathophysiology. In conditions such as ocular allergy, dry-eye disease and keratoconus, the production of various tear film constituents may be amplified or diminished.5-7 For example, specific cytokine and chemokine profiles are associated with clinical subtypes of ocular allergy (allergic conjunctivitis, vernal keratoconjunctivitis or atopic keratoconjunctivitis).5 Patients with VKC show significantly higher levels of Interleukin-4 in their tear fluid than those with AC or AKC.6 In dry eye, the inflammatory biomarkers that have shown tear-film upregulation include IL-1, IL-6, matrix metalloproteinase-9, Chemokine CCL5 (also known as RANTES) and macrophage inflammatory protein-1.8-11 Though none of these biomarkers are specific for DE, they do confirm the inflammatory nature of the disease. A recent study identified another tear component, lysozomal proline-rich protein 4, that may be more relevant as a specific biomarker for DE; reduced levels of this protein are reproducibly found in tears of DE subjects, and the extent of reduced expression appears to correlate with the severity of a patient’s DE.12 This makes LPRP4 a potential candidate as a specific biomarker for DE; as such, it could be used to identify patients for a clinical trial or to track efficacy of a prospective therapy. Quantitation of tear components are notoriously difficult, however, so additional studies are necessary to evaluate this potential biomarker as a valid DE diagnostic.
Tear film lipids, including those originating from the meibomian gland, are another important potential source of ocular surface biomarkers.13,14 Variations in fatty acid compositions in the tears of patients with meibomian gland dysfunction and those with aqueous-deficient DE have been reported.15 Other studies have reported changes in meibum composition in DE patients, and showed that several lipid species were significantly increased in this demographic, especially sphingomyelin and phosphatidylcholine.16 If these changes can be functionally linked to MGD, then a modulation of lipid composition may ultimately represent both a marker of the disease and a goal of therapeutic remedy.
In keratoconus patients, elevations of the inflammatory mediators IL-6, MMP-9 and RANTES/CCL5 in tear fluids have been reported, but they’re also seen in other conditions associated with inflammation, such as DE.17,18 Recent identification of gross cystic disease fluid protein-15 (GCDFP-15), a novel, disease-specific biomarker, suggests that it may be possible to predict or track the disease process using it.19,20 Previously identified in breast cancer tissue, GCDFP-15 is downregulated in tear samples of keratoconus patients when compared to age-matched controls. It’s thought to be involved in extracellular matrix homeostasis, and is regulated by transforming growth factor-β, both of which are linked to the pathology of keratoconus.20
No single disease exacts a greater toll on ocular function than diabetes mellitus. Epidemiological studies indicate that diabetes mellitus afflicts 350 million people worldwide and is a prelude to heart disease, kidney disease, inflammatory diseases and diabetic retinopathy.5 DR is a leading cause of blindness in middle-aged people, accounting for about 5 percent of their blindness worldwide, and its prevalence mirrors the upward trajectory of diabetes mellitus cases, emphasizing the need for viable biomarkers that could pinpoint early stages of retinal pathophysiology.
Numerous inflammatory cytokines and chemokines (which are also associated with other ocular pathologies) have been identified in the aqueous humor, vitreous and plasma of diabetic retinopathy patients.21 In recent years, differences in levels of nerve growth factor and its active precursor pro-NGF have been identified in patients with diabetic retinopathy, with a shift in the balance toward the pro-NGF, a molecule known to promote nerve atrophy and other attributes of diabetic retinopathy.22,23 It’s possible that excess pro-NGF underlies part of the pathogenesis of diabetic retinopathy; therefore, changes in NGF levels in tears or in serum could be used as a disease marker.22 Consistent with this are the observed correlation between NGF levels, the duration of diabetes mellitus, and patient hemoglobin A1C levels. Each of these suggest that this peptide growth factor has potential application as a biomarker of diabetic retinopathy.22
Imaging/Composite Biomarkers
Imaging techniques are used to visualize changes in cellular morphology and tissue ultrastructure in almost every ophthalmic disease. In allergy and dry eye, confocal microscopy imaging has been used successfully to assess cellular changes in the cornea and conjunctiva by visualizing tissue immune-cell infiltration.24 Fundus camera and scanning laser ophthalmoscopy imaging can detect incremental structural changes in the retina over time, providing early interventional treatment opportunities for patients with glaucoma or DR.25
Dry age-related macular degeneration is a particular focus of image-based biomarkers, as there are few reliable indicators of the disease before significant damage to the retina has already occurred.26 Clinical assessments of complement inhibitors, for example, have used changes in size of retinal lesions as an endpoint in trials of drugs such as lampalizumab, an antibody directed at complement factor D.27 The search for early-stage indicators for dry AMD is ongoing, and the identification of such a biomarker would be a significant step forward.
Applications of fluorescein angiography or indocyanine green angiography to fundus imaging have yielded high-contrast images of the retina and surrounding blood vessels, which, in combination with other imaging biomarkers, can greatly improve prognoses. Furthermore, the utility of combining imaging and non-imaging biomarkers may further refine their accuracy in identifying disease states. In glaucoma, the integration of images of optic disc cups and retinal nerve fiber layers taken by scanning laser tomography and scanning laser polarimetry, in addition to tracking IOP, may paint a more comprehensive picture of the patient’s glaucoma status than either technique alone.28
We all know the saying that the eyes are the windows to the soul, but they are also the windows to systemic disease. Hypertension is an excellent example of a systemic disease that can be tracked by internal eye imaging. By examining the arrangement and structure of the posterior microvasculature of the eye through a technique such as fractal dimension analysis, a long-term, integrated measure of systemic hypertension can be obtained.29 This metric can be used by clinicians when deciding the degree of intervention necessary for each patient. Systemic hypertension is known to damage the retinal blood vessel network, and images of the affected blood vessels have become a recognized diagnostic sign of long-duration hypertension among clinicians.30
Since the introduction of commercially available confocal scanning laser ophthalmoscopy and optical coherence tomography, there’s been an interest in imaging ocular biomarkers that may be of value in the diagnosis of Alzheimer’s disease. These high-resolution imaging techniques have played an important role in pinpointing pathological structural changes in the retina, optic nerve, retinal microvasculature and choroid.31 Imaging studies have also shown that beta amyloid deposits, a hallmark signature of Alzheimer’s, can be quantified on retinas and in crystalline lenses of Alzheimer’s disease cohorts.32
A composite score of multiple biomarkers might be a better choice for prognosis or for therapeutic assessment, particularly for conditions such as dry-eye disease that are difficult to objectively define. An integrated measure that incorporates both imaging and tear-assessment techniques may more reliably predict disease. An example of this is Ora’s OPI 2 system, which computes a ratio of tear-film breakup to blink rate using slit lamp video.33 The key with OPI 2 and other composite metrics is their incorporation into clinical testing in order to assess their utility and refine their value.
Merging ocular images and fluid biomarkers along with other types of biomarkers may help with diagnostic specificity and accuracy in other eye disorders and systemic diseases. In glaucoma, for example, the addition of quantified images of retinal structural changes to intraocular pressure or levels of proteins associated with glaucoma may provide a better assessment of the patient’s future outlook. While biomarkers can serve a useful purpose in evaluating an initial disease risk or diagnosis, on numerous occasions they don’t complete the narrative because of their lack of specificity for a particular disease state. Even with an extensive composite panel on hand, a larger quantity of biomarkers doesn’t necessarily guarantee accuracy in a physician’s prognosis.
Although biomarkers’ limitations mainly stem from a lack of a clear association with the clinical characteristics of a disease, continuing research, especially in the composite biomarker area, holds promise. Metrics that change before clinical manifestations of a disease are particularly helpful, as they allow for early intervention before injury has taken place. One key example of this is the search for an early indicator of dry age-related macular degeneration. Waiting for geographic lesions to progress or for changes in three lines of visual acuity doesn’t allow us to target patients at the earliest stages of disease, or to potentially treat these patients at a point in the disease when an intervention may have a greater impact. Ultimately, the goal of biomarker research, like all medicine, is effective care for our patients. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School. Dr. Dimopoulos is a medical writer at Ora Inc. Mr. Ousler is vice president for dry eye at Ora. Dr. Hollander is chief medical officer at Ora, and assistant clinical professor of ophthalmology at the Jules Stein Eye Institute at the University of California, Los Angeles.
1. https://fnih.org/news/announcements/evidentiary-criteria-released “Framework for Defining Evidentiary Criteria for Biomarker Qualification” accessed 6 Feb 2017.
2. Medeiros FA, Zangwill, LA, Mansouri K, Lisboa R, Tafreshi A, Weinreb RN. Incorporating risk factors to improve the assessment of rates of glaucomatous progression. Invest Ophthalmol Vis Sci 2012;53:4:2199-2207.
3. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: A randomized trial determines that ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120:6:701-713.
4. Kalouda P, Keskini C, Anastasopoulos E, Topouzis F. Achievements and limits of current medical therapy of glaucoma. Developmental Ophthamology 2017;59:1-14.
5. Hagan S, Martin E, Enriqeuz-de-Salamanca. Tear fluid biomarkers in ocular and systemic disease: Potential use for predictive, preventive and personalized medicine. EPMA Journal 2016;7:15.
6. Uchio E, Ono SY, Ikezawa Z, Ohno S. Tear levels of interferon-gamma, interleukin (IL)-2, IL-4 and IL-5 in patients with vernal keratoconjunctivitis, atopic keratoconjunctivitis and allergic conjunctivitis. Clin Exper Allerg 2000;30:1:103-9.
7. Leonardi A, Curnow SJ, Zhan H, Calder VL. Multiple cytokines in human tear specimens in seasonal and chronic allergic eye disease and in conjunctival fibroblast cultures. Clin Exper Allerg 2006;36:6:777-84.
8. Boehm N, Reichardt AI, Weigand M, et al. Proinflammatory cytokine profile of tears from dry eye patients by means of antibody microarrays. Invest Ophthalmol Vis Sci 2011;52:7725-30.
9. Enriquez-de-Salamanca A, Castellanos E, Stern ME, Fernandez L, Carreno E, Garcia-Vasquez C, Herreras JM, Calonge M. Tear cytokine and chemokine analysis and clinical correlations in evaporative-type dry eye disease. Mol Vis 2010;16:862-73.
10. Choi W, Li Z, Oh HJ, Im SK,Lee SH, Park SH, You IC, Yoon KC. Expression of CCR5 and its ligands CCL3, -4, and -5 in the tear film and ocular surface of patients with dry eye disease. Curr Eye Res 2012;62:151-96.
11. Leonardi A, Borghesan F, Faggian D, Depaoli M, Secchi AG, Plebani M. Tear and serum soluable leukocyte activation markers in conjunctival allergic diseases. American Journal of Ophthalmology 2000;129:2:151-8.
12. Aluru SV, Agarwl S, Srinivasan B, Iyer GK, Rajappa SM, Tatu U, Padmanabhan P, Subramanian N, Narayanasamy A. Lacrimal proline rich 4 (LPRR4) protein in the tear fluid is a potential biomarker of dry eye syndrome. PLoS One 2012;7:12:e519794.
13. Butovich IA. Tear film lipids. Exp Eye Res 2013;117:4-27.
14. Ghosh A, Nishtala K. Biofluid lipidome: A source for potential diagnostic biomarkers. Clin Transl Med. 2017;6:1:22. Epub 2017 Jun 20.
15. Joffre C, Souchier M, Gregoire S, Viau S, Bretillon L, Acar N, Bron AM, Creuzot-Garcher C. Differneces in meibomian fatty acid composition in patients with meibomian gland dysfunction and aqueous deficient dry eye. British Journal of Ophthalmology 2008:92:116-9.
16. Lam SM, Tong L, Yong SS, Li B, Chaurasia SS, Shui G, Wenk MR. Meibum lipid composition in Asians with dry eye disease. PLoS One 2011;6:e24339.
17. Shetty R, Ghosh A, Lim RR, Subramani M, Mihir K, Reshma AR, Ranganath A, Nagaraj, et al. Elevated expression of matrix metalloproteinase-9 and inflammatory cytokines in keratoconus patients is inhibited by cyclosporine. Invest Ophthalmol Vis Sci 2015;56:2:738-50.
18. Kolozsvari BL, Petrovski G, Gogolak P, Rajnavolgyi E, Toth F, Berta A, Fodor M. Association between mediators in the tear fluid and the severity of keratoconus. Ophthalmic Research 2014;51:1:46-51.
19. Priyadaersini S, Hjortdal J, Sarker-Nag A, Sejersen H, Asara JM, Karamichos D. Gross cystic disease fluid protein-15/prolactin-inducible protein as a biomarker for keratoconus disease. PLoS One 2014;18;9:11:e113310.
20. Priyadarsini S, McKay TB, Sarker-Nag A, Karamichos D. Keratoconus in vitro and the key players of the TGF-β pathway. Mol Vis 2015;21;21:577-88.
21. Cheung CM, Vania M, Ang M, Chee SP, Li J. Comparison of aqueous humor cytokine and chemokine levels in diabetic patients with and without retinopathy. Molecular Vision 2012; 18:830-7.
22. Mohamed R, El-Remessy AB. Imbalance of the nerve growth factor and its precursor: Implication in diabetic retinopathy. J Clin Exp Ophthalmol 2015;6:5.
23. Barcelona PF, Sitaras N, Galan A, et al. p75NTR and its ligand ProNGF activate paracrine mechanisms etiological to the vascular, inflammatory, and neurodegenerative pathologies of diabetic retinopathy. J Neurosci 2016;36:34:8826-41.
24. Villani E, Mantelli F, Nucci P. In vivo confocal microscopy of the ocular surface: Ocular allergy and dry eye. Current Opinion Allergy Clinical Immunology 2013;13:50:569-76.
25. Gramatikov B. Modern technologies for retinal scanning and imaging: An introduction for the biomedical engineer. Biomedical Engineering Online 2014;13:52.
26. Hanus J, Zhao F, Wang S. Current therapeutic developments in atrophic age-related macular degeneration. Br J Ophthalmol 2016;100:1:122-7.
27.http://www.roche.com/investors/updates/inv-update-2013-08-27.htm. Accessed 19 July 2017.
28. Windisch BK, Harasymowycz PJ, See JL, Chauhan BC, Belliveau AC, Hutchison DM, Nicolela MT. Comparison between confocal scanning laser tomography, scanning laser polarimetry and optical coherence tomography on the ability to detect localized retinal nerve fibre layer defects in glaucoma patients. British Journal of Ophthalmology 2009;93:1-1.
29. Cheung CY, Thomas GN, Tay W, Ikram MK, Hsu W, Lee ML, Lau QP, Wong TY. Retinal vascular fractal dimension and its relationship with cardiovascular and ocular risk factors. Amer J Ophthalmol 2012;154:4:663-74.
30. Ponto KA, Werner DJ, Wiedemer L, et al. Retinal vessel metrics: Normative data and their use in systemic hypertension: Results from the Gutenberg Health Study. J Hypertens 2017;35:8:1635-1645.
31. Lim JKH, Li QX, He Z, Vingrys AJ, Wong VH, Currier N, Mullen J, Bui BV, Nguyen CT. The eye as a biomarker for Alzheimer’s disease. Front Neurosci 2016;10:1-14.
32. Kerbage C, Sadowsky CH, Tariot PN, Agronin M, Alva G, Turner FD, Nilan D, Cameron A, Cagle GD, Hartung PD. Detection of amyloid beta signature in the lens and its correlation in the brain to aid the diagnosis of Alzheimer’s Disease. Amer J Alzheimers Dis Other Demen 2015;30:738-45.
33. Abelson R, Lane KJ, Rodriguez J, Johnston P, Angjeli E, Ousler G, Montgomery D. Validation and verification of the OPI 2.0 System. Clin Ophthalmol 2012;6:613-22.



