Year after year, the annual meeting of the Association for Research and Vision in Ophthalmology demonstrates that even though LASIK and PRK have been approved in the United States for more than a decade, surgeons are still developing new ways to improve their outcomes with the procedures. In this year’s refractive surgery section of the meeting, you’ll see studies on how to get the best results with laser procedures, as well as the latest data on cutting-edge techniques such as intrastromal ablations and corneal inlays.
Techniques and Outcomes
Surgeons from Mexico City say that the actual post-LASIK corneal tissue ablation depth may be greater than that predicted by the Abbott Medical Optics/Visx Star S4, and that this should be taken into account in patients with thin corneas.
The researchers retrospectively analyzed 36 eyes of 19 patients. They excluded seven patients who were lost to follow-up and excluded two eyes due to surgical complications. Their mean preoperative spherical equivalent was -4.07 ±1.92 D, which was decreased to 0.18 ±0.73 D postop. The researchers performed corneal ultrasonic pachymetry (Accupach V 24-5000; Accutome, Malvern, Pa.) before surgery and one month afterward in order to obtain the postsurgical corneal tissue ablation by subtraction. The mean predicted ablation depth was 49.11 ±28.07 µm, but the actual postoperative depth was 61.64 ±28.07 µm. The surgeons say this potential disparity should be considered in order to avoid residual stromal beds of less than 300 µm.3128
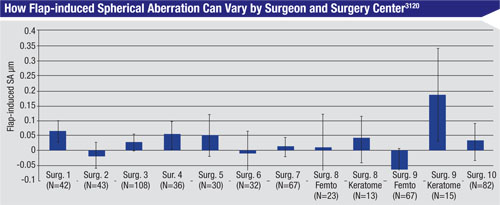
Researchers from AMO say that, after evaluating the data from controlled clinical refractive surgery studies, it may be possible to estimate the amount of aberration induced by the LASIK flap and then adjust the procedure’s treatment target.
The researchers say that flap-induced aberrations aren’t dependent on the amount of treatment, but instead can differ among surgeons, tools used and surgery sites. (See bar graph, p. 68.) They add that flap-induced aberrations can be measured directly or estimated statistically, pointing out that in the trend line for induced spherical aberration, with SA vs. preop spherical equivalent, SA usually crosses the axis SE=0 at some non-zero level. They say that this value quantifies the change in SA when the flap is created but no ablation is done. They add that the flap-induced aberrations may also be derived from a flap-creation model that accounts for site-specific parameters.
In practice, the researchers say that flap-induced aberrations may be taken into account during treatment planning, when surgeons can apply treatment target adjustments to compensate for them. These adjustments, the investigators say, can be derived statistically for each site, surgeon or tool. They say that the site-specific SA can be readjusted so that the adjusted scatter plot will become more compact, with tighter correlation and R2 values, allowing a better fit for the nomogram adjustment and more precise modeling of corneal healing.3120
|
In the study, 90 patients underwent normal LASIK, femtosecond lenticule extraction or SMILE, and were followed for over a year. The mean preoperative spherical refractive error was -7 D (r: -4.5 to -11 D), with a mean spherical equivalent of -7.28 D. Three months postop, the average spherical refraction was -0.32 ±0.63 D for the LASIK group, 0.00 ±0.38 D for the FLEX group and 0.06 ±0.51 D for the SMILE group. The average SE refraction was -0.49 ±0.71 D for the LASIK group, -0.13 ±0.45 for the FLEX group and -0.10 ±0.49 D for the SMILE group. An analysis of variance showed no significant change in the SE over the long term after the three-month visit. (Outcomes appear in Tables 1 and 2.) The uncorrected vision in the FLEX and SMILE, but not LASIK, patients improved significantly over the longer period, surgeons say. They add that best-corrected vision didn’t show any significant difference over the long term.3131
A group of surgeons from Mexico City are also sharing their experience with the learning curve of the new SMILE procedure for the treatment of myopia. One of the surgeons receives some financial support from Carl Zeiss Meditec.
|
Investigators from several research facilities and ophthalmology practices in Texas say that CustomVue LASEK is accurate in high myopia, but that surgeons need to make appropriate preoperative adjustments to the surgical plan or risk having to do an enhancement.
The investigators performed a retrospective analysis of 113 eyes of 69 LASEK patients who had either a standard or a CustomVue ablation. The standard ablation group, in which the physicians used the system’s ability to make adjustments to the target refraction, included 63 eyes with an average error of -7.49 D and an average cylinder of -1.41 D. The CustomVue group, in which they also used the adjustments, was composed of 50 eyes with an average sphere of -6.56 D and an average astigmatism of -0.63 D. The researchers say that the use of mitomycin-C was slightly higher in the standard group (74 percent of patients vs. 54 percent) but wasn’t different between the preoperative <0.1 µm normalized polar Zernike coefficient and the >0.1 µm NPZE CustomVue spherical aberration groups.
The group says that the mean postop SE wasn’t significantly different between the two groups (standard group mean: +0.07 ±0.62 D; CustomVue mean: +0.15 ±0.58 D). When they removed the preop physician adjustments from the treatment, the researchers found that 32 percent of the CustomVue LASEK eyes would have had a final result of ±0.5 D or greater. Twenty-three of the 50 eyes had a preop positive spherical aberration >0.1000 µm NPZE, and without a physician adjustment these 23 eyes would have been responsible for 69 percent of the eyes with a postop refraction of ±0.5 D or more.
The researchers say that, though their results using physician adjustment factors for the ablations were good, patients with preop spherical aberration greater than 0.1 µm NPZE are at higher risk of needing an enhancement if a physician doesn’t use an adjustment in the surgical planning.3139
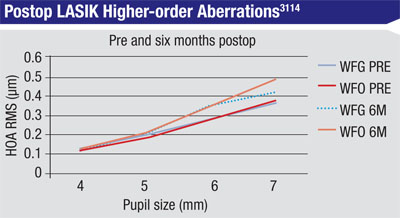
Surgeons from the U.S. Army Warfighter Refractive Surgery Research Center in Virginia, the Walter Reed Military Medical Center in Maryland, and the Wilmer Eye Institute say a small-scale, randomized study of wavefront-guided vs. wavefront-optimized LASIK shows little difference between the two in terms of quality of vision as defined by higher-order aberrations and patient satisfaction.
The surgeons randomized 18 patients, all around 30 years old, to WFG surgery and 17 to WFO. The average preop refraction was -2.96 ±0.97 D for WFG patients and -3.62 ±1.57 D for WFO. They analyzed the root mean square value of HOAs at four different pupil sizes, and administered a questionnaire to the patients preoperatively and at six months postop.
At six months postoperatively, the patients’ manifest spherical equivalent refraction was 0.04 ±0.27 D for WFG vs. -0.02 ±0.26 D for WFO (p=0.33). (The HOA results appear in the graph at left.) The researchers say there was no significant difference in RMS HOA when comparing WFG vs. WFO LASIK, and that the questionnaire didn’t show any differences in terms of the patients’ expected visual outcomes vs. what they achieved.3114
Surgeons from the same facilities also compared aberrations in PRK. In the study, they randomized 52 patients to receive either WFG or WFO PRK. Preoperatively, the WFG patients had an average spherical equivalent of -3.49 ±1.88 D vs. -3.31 ±1.79 D. At six months, the average SE was 0.09 ±0.38 D vs. -0.02 ±0.31 D for WFO (p=0.09). In terms of HOA RMS, however, there were significant differences between the two procedures over time, the surgeons say. They add that even though there was a significant increase in HOA RMS of WFO PRK patients, results from a questionnaire showed no significant difference in daily activities, glare, halo or satisfaction with the procedure compared to WFG PRK.3135
Implant Rundown
Employees of and consultants to ReVision Optics have provided an update on the company’s treatment for presbyopia, the Raindrop hydrogel corneal inlay.
|
After implantation, the surgeons found that, at three months, uncorrected visual acuity had improved by an average of five lines at near, three lines at intermediate and one line at distance when both eyes were measured separately. Near and intermediate vision improved in all the eyes. Eighty-six percent of the implanted non-dominant eyes and 95 percent of the implanted dominant eyes achieved at least 20/25 at near uncorrected vs. zero percent preop. At distance, the average uncorrected acuity was 20/21. Two patients lost a line of distance vision in their non-dominant eyes.
After the second inlay was implanted, at three months 95 percent saw 20/25 or better at near and intermediate uncorrected, and all saw 20/20 or better at distance. The researchers say that patients reported a significant improvement in task performance with bilateral inlays versus preop performance.3129
Refractive Issues
Researchers in China say that the amount of tear secretion after LASIK may depend greatly on the residual corneal nerve density at one month postop.
In the prospective study, surgeons enrolled 16 patients who were undergoing bilateral myopic LASIK, and measured the height and area of the upper and lower tear menisci using real-time anterior segment optical coherence tomography before surgery, and then at one week, one month and three months. They also measured central, temporal and nasal subbasal nerve densities with confocal microscopy preop and at one month and three months postop. The investigators didn’t specify the technology that was used to create the flap in the LASIK procedures.
|
The investigators say that the study suggests that lower tear menisci recover continuously between one week and three months after LASIK surgery, accompanied by increased temporal and nasal corneal nerve densities. They note that the residual corneal nerves at the one month follow-up point seem to play a large role in tear secretion during the rest of the postop period.3142
Researchers from the Federal University of São Paulo and São Paulo Hospital in Brazil say that it pays to determine the quality of the water used to feed steam sterilization devices in order to avoid infection after refractive surgery.
The investigators collected water samples in three different surgery centers that each used the same model of steam sterilizer for their cases. Two of the centers used tap water that underwent filtration and distillation and was stored in non-sterile gallon containers. At those two facilities, samples were collected from the tap, filter hose, distillation outlet and collector, and the stored gallons. The third center used sterile water, so the researchers took a sample from the water bag.
In samples from the first center, the study doctors found Mycobacterium chelonae in the distilled water gallons and the steamer reservoir. From the tap water they found Mycobacterium mucogenicum. The researchers say that all the M. chelonae isolated colonies showed the same pulsed-field gel electrophoresis pattern, meaning that a single strain was in both the distilled water and the storage gallons. They also found other aerobic bacteria in the storage gallons and steamer reservoir. In the second center, they found M. chelonae in samples from the tap and filter hose, and identified other aerobic bacteria in samples from the distillation outlet and collector, storage gallons, steamer reservoir and hose. Samples from the third center, however, which used sterile distilled water, showed no evidence of microorganism growth.3145
Surgeons from the Massachusetts Eye and Ear Infirmary, the Boston Foundation for Sight and Harvard Medical School say that in vivo confocal microscopy can help surgeons identify the mechanism behind the long-term postoperative pain that can follow refractive surgery, including LASIK.
In the study, two masked observers analyzed laser in vivo confocal microscopy images of 17 patients with corneal pain after refractive surgery (28 LASIK eyes and five PRK eyes), and 62 controls. The patients reported constant pain and photophobia. Ninety-four percent of the subjects had sensitivity to air and 47 percent were sensitive to chemical fumes.
|
The researchers say that, though postoperative keratoneuralgia that some patients experience after LASIK may be associated with minimal findings on clinical exam, there are also microscopy findings that correlate with its symptoms and may help physicians better understand this syndrome.3711
Researchers from the United States and Optical Express in the United Kingdom, with funding from the National Eye Institute, That Man May See Inc., and Research to Prevent Blindness, have shed some light on the effects of temperature and humidity on LASIK by analyzing more than 200,000 cases done at Optical Express’ surgery centers in the United Kingdom and Ireland.
The study looked at the results of 202,394 eyes of 105,712 patients who had LASIK at Optical Express. The researchers found that an increase of 1 C during LASIK was associated with a refraction that was 0.003 D more hyperopic at one month postop (p=0.0094) and a 1-percent increase in humidity was associated with a 0.0004 D more myopic refraction (p<0.0001). The physicians say that the effects were considered clinically insignificant and remained the same or similar with myopic eyes, hyperopic eyes and subgroups of eyes stratified by age and the level of preop refractive error.3110
Researchers also analyzed 186,019 eyes of 95,523 Optical Express LASIK patients to assess the rate of microbial keratitis and any factors associated with it. In this group of patients, 16 had either culture-proven infection or a strong clinical suspicion of it (0.017 percent or 1:5,970). The investigators say that there was a higher incidence of infection in men vs. women (0.023 vs. 0.012 percent), in myopes vs. hyperopes (0.018 vs. 0.010 percent), in PRK vs. LASIK (0.032 vs. 0.015 percent) and mechanical-microkeratome vs. femtosecond laser-created flap patients (0.025 vs. 0.013 percent). However, they don’t indicate whether these rates reached statistical significance.3126
|
In the study, 58 patients (95 eyes) who had undergone myopic LASIK were tested with manifest refraction, H-S aberrometry and Pentacam scanning. Aberrations were measured under mydriatic conditions (pupil size greater than 8 mm) and the effective pupil size was acquired from the aberrometer.
The researchers say that, in all patients, the effective pupil size in the study was smaller than the actual pupil size, with average sizes of 6.9 ±0.53 mm (mild myopia, n=15, p<0.01), 6.56 ±0.37 mm (moderate myopia, n=26, p<0.0001) and 5.84 ±0.55 mm (high myopia, n=54, p<0.0001). They found that the effective pupil size was correlated to the level of correction that was attempted in the surgery (correlation coefficient [r]=-0.8, p<0.0001), the ablation depth (r=0.65, p<0.0001), the optical zone (r=0.7, p<0.0001) and the postop corneal eccentricity (r=0.57, p<0.0001). They say all these attributes are independent factors in determining the effective pupil size, and that a mathematical model of the effective pupil size can be determined with the following formula: -0.81*Rx of ablation + 1.11*optical zone + 0.55*postop eccentricity value (r2 = 0.997).3118
Ectasia Screening Tools
Surgeons from Rio de Janeiro and São Paulo, Brazil say that an integrated analysis of clinical findings, topometric and tomographic data may be better at identifying eyes at risk for postop ectasia than a “classic” ectasia risk score system. One of the surgeons is a consultant to Oculus, maker of the Pentacam, which was used in the integrated analysis.
In a retrospective, non-randomized fashion, the researchers looked at 23 eyes that developed ectasia after LASIK and 266 eyes with stable LASIK outcomes (after a minimum of a year follow-up). In all cases, the preoperative clinical and Pentacam data were available. The surgeons used the ERSS based on age, SE, residual stromal bed, central thickness and a subjective classification of corneal topography’s front surface axial map. They also assessed the curvature of the front surface (topometry) and the thickness profile and front/back elevation (tomography). The researchers developed different factors that best distinguished ectasia from stable LASIK groups using Fisher’s linear discriminant analysis based on clinical parameters and topometric data individually, as well as on clinical parameters combined with tomographic data. The area under the receiver operating characteristic curve, in which a value of 1.00 is considered a perfect result, was calculated for each LDA function with pairwise comparisons.
The surgeons say they found statistically significant differences among the groups for all of the study’s parameters (p<0.001) except for preoperative SE. Using the ERSS, in which a score of 4 indicates high risk for ectasia and a zero indicates a patient at very low risk, 12 eyes from the ectasia group had a score of 3 or higher (sensitivity: 52 percent) and 48 eyes from the stable group scored a 3 or higher (specificity: 82 percent). The best parameters, using clinical and topometric indices as identified by the LDA function, used the index of height decentration, which had an area under the ROC of 0.98 (sensitivity: 100 percent; specificity: 93 percent). The best LDA function combining clinical and tomographic parameters, including the Belin-Ambrosio Deviation, which achieved 100-percent sensitivity and 97-percent specificity, had a statistically better area under the ROC of 0.994 than all individual parameters (p<0.001).
The surgeons say that the integrated analysis of clinical and objective topometric parameters was superior to the ERSS, and that tomographic data significantly enhanced the ability to screen for ectasia risk among LASIK candidates. The investigators add that clinical parameters, in turn, significantly improve the ability to detect ectasia susceptibility based on tomographic data, but that further validation is necessary for the LDA functions.3715
Researchers from Oregon Health & Science University and private ophthalmology practices in New York and San Diego, some of whom own patents for the technology discussed or are consultants to the companies that make the diagnostic imaging technology, say that anterior segment OCT images of corneal, epithelial and stromal thickness map patterns have potential as a screening tool for keratoconus.
The researchers developed a computer algorithm to calculate the corneal, epithelial and stromal thickness maps from the Optovue RTVue CAM OCT. In their analysis, they defined a “pattern map” as the thickness map divided by the average thickness of the map.
The surgeons designated 108 eyes of 57 patients as a “training” group (i.e., defining the pattern maps that would be considered normal), and 42 eyes of 22 patients as the “evaluation” group (i.e., they’d be used to evaluate the accuracy of the system). The OCT maps of the training group were then averaged and normalized to serve as the normal average pattern maps. The corneal, epithelial and stromal thickness map pattern standard deviation values were calculated by the RMS of the difference between the individual pattern maps and the normal average pattern maps. In the study, the accuracy of the method in distinguishing forme fruste KC eyes from normals was determined by the area under the ROC.
In terms of results, the researchers say that the PSD values for the subjects’ stromal, corneal and epithelial thickness maps were all significantly higher in the FFKC eyes compared to the normal evaluation group (p<0.001). The area under the ROC values were 0.988 (pachymetry map PSD), 1.00 (epithelial thickness map PSD) and 0.967 (stromal thickness map PSD).
After seeing the level of accuracy displayed by pattern map analysis, the investigators say the process may be useful in the detection of early keratoconus.2587 REVIEW
Dr. Probst is national medical director for TLC The Laser Center.