Corneal collagen cross-linking continues to be a mainstay of research reports in this year’s ARVO Cornea selections. Expanding the pool of patients who may potentially benefit from the procedure and improving various aspects of the technique are a big emphasis for researchers. Along with a look at dry eye, transplant techniques and other traditionally rich areas of corneal research, here are just a few of the representative abstracts from this year’s offerings.
Cross-linking—Technique
Italian researchers report that a new riboflavin formulation increased corneal penetration in pig eyes by 852 percent vs. the commercial riboflavin-5-phosphate (RFP). The new complex, riboflavin MDV1224, and commercial riboflavin-5-phosphate were placed in donor chambers with excised porcine cornea at 37 C for 360 minutes. The receiver chamber contained an isotonic phosphate buffer saline solution. Samples were collected from the receiver chamber every 60 minutes and quantitatively analyzed by high- performance liquid chromatography.
Trans-corneal permeability, cm/sec, was calculated by plotting the amounts (µg/cm2) of riboflavin in MDV1224 or RFP that permeated through the corneal cells over time (minutes). Riboflavin stability in MDV1224 was also monitored for six months in dark conditions and compared to RFP.
Trans-corneal permeability of MDV1224 (45.7 x 10-6 cm/sec) was almost tenfold greater compared to that of RFP (4.8 x 10-6 cm/sec). After six months, stability data at 40 C and 25 C showed high degradation values for both riboflavin in MDV1224 and RFP formulations, while at 2 to 8 C riboflavin in MDV1224 and RFP showed only 3 percent degradation.
The group call for in vivo studies to confirm that the higher delivery of MDV1224 vs. RFP is able to guarantee a correct corneal cross-linking in the intact human cornea.5259
|
The prospective, randomized clinical trial analyzed 41 eyes with KC and ectasia. All patients were initially treated with symmetric 350-µm Intacs segments. Patients were randomized into one group that received standard CXL immediately following the Intacs procedure (concurrent group, n=23), and a second group that received the identical CXL treatment three months after the initial Intacs procedure (sequential group, n=18). All outcomes were analyzed one year after CXL therapy. Outcomes included UCVA and BCVA, and maximum (Kmax), flat (Kf), steep (Ks) and average (Kavg) keratometry as measured by the Pentacam (See results, above). When the sequential vs. concurrent groups were compared at one year, there were no statistical differences between the changes in any of the visual or topographic outcomes except for Kflat. All patients who were treated with symmetric Intacs and CXL therapy experienced an improvement in corneal topography and UCVA one year after therapy. There was no meaningful difference between sequential vs. concurrent treatment at one year.5264
Epithelial thickness appeared to be greater in keratocones, possibly as a reaction to ectasia, researchers in New York City and Athens, Greece, say of their study that used imaging from anterior-segment optical coherence tomography and high-frequency ultrasound biomicroscopy.
Thickness mapping was studied in eyes in a normal group, keratoconic group (KCN) and keratoconic eyes treated with collagen cross-linking group (K CXL).
Substantial topographic variation in epithelium thickness was seen in the KCN group, however, there was an overall thickening of the epithelium, particularly over the pupil center onthe order of +3 μm, while the mean epithelial thickness was on average +1.1 μm compared to normals. No statistically significant difference was found between the normals and the K CXL group in terms of overall epithelium thickness. This finding was more pronounced among younger patients, and in agreement with HF ultrasound epithelial thickness imaging.
This researchers say the method may aid in sub-clinical screening, particularly among young patients.5294
Cross-linking—Pediatric
Surgeons in Switzerland conclude that cross-linking is very effective in stabilizing keratoconus in children. They evaluated tomographies (Pentacam) and topographies (TMS) of prospectively collected data after CXL in children younger than 18 years. Examinations were conducted prior to surgery at regular intervals during the first postoperative year, and at two, three and four years after the procedure. Twenty-five patients (33 eyes) were included (mean age, 14.9 years) with a mean follow-up of 27.3 months, and minimum follow-up one year. Progression was defined as an increase in Kmax (Pentacam) of at least 1 D in one year.
The researchers made 669 KMax comparisons, resulting in four cases of progression identified. In one case, the keratoconus was extremely advanced prior to CXL (Kmax 78.2 D preop, and 79.3 D at one year). One case showed marked steepening of 3.4 D in the Pentacam between three and four years after CXL, but the TMS parameters were unchanged. Because of this discrepancy, the Pentacam exam was repeated and showed that Kmax was actually stable, i.e., no progression after all (50.8 D at three years and 50.7 D at four years). Two children with active limbal vernal keratoconjunctivitis worsened dramatically (46.4 D at one year and 48.3 D at two years; 53.6 D at one year and 54.9 D at two years). This progression was also seen in topography. After resolution of the limbal inflammation, the Kmax values returned to 46.3 D and 54.2 D, respectively.
True progression after CXL could only be verified in one out of 33 eyes, but that eye had already progressed to such an extreme extent prior to CXL that it was probably unrealistic to expect that CXL could arrest progression at such a late stage. Further, in assessing possible progression, the use of two different measuring devices can help detect discrepancies and thus prevent false conclusions. Moreover, limbal vernal changes can present a clinical picture of progression. However, this is actually a pseudo-progression that can be reversed with anti-inflammatory treatment.5262
Two-year results of cross-linking in pediatric patients with progressive keratoconus come from another group of Swiss and Italian surgeons.
Forty-eight eyes of pediatric patients (mean age 13.7 ±1.9 years, r: 4 to 18 years) with topographically and tomographically documented progressive keratoconus were treated with cross-linking. The standard treatment procedure was used, applying riboflavin 0.1% following epithelial abrasion. The corneas were then irradiated with UVA light. The eyes were monitored for a minimum of 24 months. CDVA, UDVA, refraction, topography, tomography and aberrations were documented at one, three, six, 12 and 24 months.
At 24 months after CXL, mean logMAR UDVA had significantly (p<0.05) improved from 0.81 ±0.25 to 0.61 ±0.23. Mean CDVA improved from 0.43 ±0.14 to 0.21 ±0.13 (p<0.05). Mean SE refraction had improved from -3.65 D ±3.49 D to -2.14 D ±2.26 D. Accordingly, mean SE refraction showed a significant decrease of 1.51 D, in line with the statistically significant reduction of both sphere and cylinder. Topography maps exhibited a statistically significant (p<0.05) reduction of mean simulated keratometry in the flattest meridian from 46.35 D to 45.28 D, and a near-significant decrease in the steepest meridian from 51.53 D to 50.20 D. Mean pachymetry, after an initial decrease, recovered by 12 months and remained stable through the follow-up period. There was a significant (p<0.05) decrease in total, corneal and higher-order aberrations at 24 months, but no significant change in endothelial cell counts at any time during the follow-up. Abrasion-related discomfort was reported by most patients in the immediate postoperative period, but there were no significant vision-related adverse effects.
The group concludes that CXL appears to stabilize keratoconus even long term in pediatric patients, the age group that shows the most dramatic progression when left untreated. The procedure further improves UDVA and CDVA. This improvement is likely due to the significant reduction of corneal asymmetry and corneal as well as total wavefront aberrations.5267
Surgeons in Rio de Janeiro, Brazil, studied a slightly older group of teenagers with progressive keratoconus, and report one-year outcomes of epithelium-off corneal collagen cross-linking.
The prospective, non-randomized, interventional clinical study enrolled 51 KC patients (84 eyes).
Mean patient age was 16.50 ±1.68 years (r: 13 to 18 years). The UCVA improved from 0.65 ±0.41 to 0.55 ±0.42 (p=0.34) and the CDVA, from 0.26 ±0.21 to 0.16 ±0.16 (p=0.74). The flat K value decreased from 46.68 ±2.65 D to 46.31 ±2.6 D (p=0.61), and the steep K value decreased from 49.83 ±3.19 D to 49.45 ±3.09 D (p=0.74). The mean preoperative corneal pachymetry at the thinnest point was 456.26 ±52.50 µm. This value decreased to 393.26 ±76.96 µm at six months (p<0.001) and to 423.79 ±72.41 µm at 12 months (p< 0.001).5266
Cross-linking—Miscellaneous
Ultrasound treatment may facilitate the entry of topical riboflavin into the corneal stroma, achieving clinically useful concentrations of riboflavin without removing the corneal epithelium and reducing the risk profile of cross-linking procedures, based on a study at the University of California, San Francisco.
Rabbit eyes had a cup with riboflavin 0.1% placed over the central cornea and were treated with ultrasound 1 W/cm2 at 880 Khz for six minutes followed by the removal of the cup and the application of two drops of riboflavin solution every three minutes for 39 minutes. In the control eyes (no ultrasound), two drops of riboflavin solution were applied every three minutes for 45 minutes. The excised corneas were examined by confocal microscopy to detect the presence of riboflavin.
Fluorescence intensity was significantly higher in the treated corneas (p<0.05). At a depth of 200 µm, average fluorescence intensity of riboflavin was 216.24 in treated eyes (n=7), and 6.55 in control eyes (n=6).5269
Researchers at Avedro Inc. suggest that both pulsing UVA and performing the UVA irradiation in an oxygen-rich environment increased the amount of cross-linking achieved for the same energy dose. When combined, the two have an additive effect.
Pig eyes were brought to 37 degrees C in a humidity chamber, epithelium was removed, and an intraocular pressure of 15 mmHg was applied using a water column. Drops of 0.1% riboflavin in 0.85% saline were applied in a humidity chamber for 20 minutes. Eyes in oxygen groups had 100 percent oxygen pumped into the chamber for the final five minutes of pre-soak. Eyes were then placed under a UVA and irradiated at 30 mW/cm2 either with constant irradiance or pulsed at a rate of 1.5 seconds on, 1.5 seconds off, either in the ambient atmosphere or in the oxygen-enriched chamber, for a total UVA dose of 5.4 J/cm2. A central 9-mm diameter, 200-µm thick flap was cut by femtosecond laser from the anterior surface of the cornea. The corneal flaps stretched until either a maximum load of 5N was applied or the sample failed. Flaps were then removed and digested in papain. Papain solutions were excited at 360 nm in a fluorometer.
Mechanical analysis showed an increase in corneal stiffness and fluorometric analysis showed a higher response at 450 nm for cross-linking performed in an oxygen-rich environment. The result was the same for pulsed UVA. The combination of pulsed UVA and an oxygen-rich environment produced the most corneal stiffening and the highest fluorometric response.5281
Dry Eye, Tears, Ocular Surface
Researchers at the Wilmer Eye Institute at Johns Hopkins, Baltimore, evaluated the prevalence of associated inflammatory systemic diseases in patients with dry eye. They reviewed the records of 264 patients with a primary diagnosis of dry eye over two years and divided them into two groups: patients with clinically significant dry-eye disease (Schirmer test result without topical anesthesia ≤10 mm at five minutes in either eye, or bulbar conjunctival staining with lissamine green scored based on Oxford scale ≥1 in either eye) and patients with dry-eye symptomatology but without the clinical findings.
The majority of the patients (81.4 percent) were female; 217 (82.2 percent) had clinically significant dry eye. About half of the patients (45.8 percent) had an underlying inflammatory systemic disease on presentation; 109 of these (90.1 percent) had a clinically significant dry eye. Thirty one patients (11.7 percent) had primary Sjögren’s syndrome; 38 (14.4 percent) had thyroid disease; 13 (4.9 percent) had rheumatoid arthritis; 42 (15.9 percent) had other rheumatic diseases.
In 50 patients without a previously known systemic disease (regardless of the severity of the dry eye) a further workup was performed based on review of systems. In 12 of those patients (24 percent) a diagnosis based on the workup was established: 10 patients (20 percent) were diagnosed with thyroid eye disease; two patients (4 percent) were diagnosed with Sjögren’s syndrome or presumed Sjögren’s syndrome; and one (2 percent) was diagnosed with a mixed connective tissue disease.
Based on clinical suspicion and review of systems, further diagnostic testing might uncover some of these previously undiagnosed conditions, the authors say.931
Higher circulating plasma levels of sex hormones appear to play a role in increased symptoms of dry eye in females without ocular surface disease, but not in males, and appear not to be influenced by age, says a group of researchers in Germany and Australia.
The study involved 74 subjects without ocular surface disease, including 52 females (mean age 35.3 ±13.4 years, r: 18.8 to 70.3) and 22 males (mean age 34.2 ±13.8 years, r: 20.2 to 75.3). Subjects completed the Dry Eye Questionnaire (DEQ5) and numerical ratings of discomfort, dryness, foreign body sensation, burning and watering. Tear osmolarity and volume (Phenol Red Thread) were assessed. Venous blood was collected and plasma concentrations of oestradiol (E2) and total testosterone (TT) were determined using ELISA.
Mean group E2 concentration was 65.2 ±50.9 pg/ml in females and 40.7 ±23.8 pg/ml in males; TT concentration was 0.49 ±0.29 and 4.3 ±1.6 ng/ml respectively. All symptom measures were higher in females (p<0.05). Tear volume was reduced in females (p=0.02); there was no difference in tear osmolarity. In females, increased ocular symptoms correlated with higher levels of E2 (DEQ5 Rho=0.36, p=0.01; dryness Rho=0.36, p=0.01; FB Rho=0.37, p=0.01). Higher TT in females correlated with more FB sensation (Rho=0.30, p=0.03) and lower tear volume (Rho=-0.30, p=0.04). No association was found between tear osmolarity and hormone levels in females. In males, no evidence of a relationship between hormone levels and ocular symptoms or tear parameters was apparent. Although concentrations of E2 and TT were reduced with age in females (E2 Rho=-0.36, p=0.01; TT Rho=-0.37, p=0.01), there was no association between age and ocular symptoms in either males or females.
The group looks for more detailed analysis and exploration of factors such as levels of free testosterone to further explore these relationships in the pathophysiology of dry eye.969
Two Boston researchers developed the Korb-Blackie Lid Light Test to investigate the possibility that apparently normal, closed lids fail to create the necessary protective seal to prevent ocular surface dessication during sleeping. The test results, they report, are correlated with symptoms of eye discomfort upon awakening.
The subject rests his head against the head rest of a semi-reclined exam chair and closes his eyes as if falling sleep. A transilluminator is lightly placed against the closed outer upper eyelid of each eye. The apparently closed lids are examined for the presence of any light emanating from the lid area between the lashes. The examiner positions his eye level inferiorly in order to be looking up to optimize viewing of three regions of the lid: temporal; central; and nasal. The amount of visible light in each section was quantified on a scale of 0 to 3 where 0=no light, 1=minimal, 2=moderate and 3=severe. Eye discomfort upon awakening was quantified on a scale of 0 to 2 where as 0=no discomfort, 1=mild and 2=significant discomfort.
They studied 148 patients, mean age 53.9 ±16.2 years (50 males; 98 females), with no lid abnormalities or history of lid surgery, no current ocular disease and no ocular surgery within six months. The mean light score for each lid region was: temporal=0.3 ±0.5; central=1.0 ±1.0; nasal=0.5 ±0.7, indicating the central region is the least likely to close completely. The level of eye discomfort upon awakening was significantly correlated with the number of lid sections (0-3) emanating light during the test (p<0.0001).942
Researchers in Rome, Italy and Philadelphia collaborated to quantify the variability of tear osmolarity measurements in dry-eye patients and controls. Using the TearLab system, they studied 74 eyes of 37 subjects (18 Sjögren’s syndrome, 10 blepharitis and nine controls with no history of symptoms or signs of dry-eye disease); 94 percent of Sjögren’s patients and 80 percent of blepharitis patients were on systemic or topical dry-eye medications on enrollment. For all subjects, three consecutive osmolarity measurements were taken at one-minute intervals in each eye to assess the within-session variability. For 15 subjects, three measurements were taken at each of three time points throughout the day to examine the inter-session variability over the course of a day. The within-session and inter-session variability were assessed based on the standard error of measurement (SEM), calculated from the analysis of variance.
Among all subjects, the within-session variation for a single osmolarity measurement was 14.4 mOsm/l (13.8 for SS, 8.8 for blepharitis, and 16.2 for controls). When the average of the three consecutive measurements in a single session was used, the variability of osmolarity measurement was 8.3 mOsm/l. Between-session variability was 17.2 mOsm/l for a single osmolarity measure, and 10.4 mOsm/l for an averaged measurement. The variability of osmolarity measurements between two eyes of the same subject was not correlated.959
A group in Houston has identified what it calls Zone A Posterior Lid Margin Vascularization and says it may be a helpful clinical sign of early ocular surface disease.
Their retrospective analysis included 49 patients >20 years old seen in a tertiary care center who completed the Ocular Surface Disease Index questionnaire and had a complete ocular surface evaluation, including anterior blepharitis, vascularization of the inferior lid margin, meibomian gland obstruction and turbidity. Previous surgery or current topical anti-inflammatory treatment were exclusions. Basal tear test, lissamine green staining and quantification of the Zone A (ZA) was graded based on the degree of vascularization noted on the everted posterior inferior lid margin. OSDI scores were grouped as normal: ≤12 vs. dry eye: >12; ZA was grouped normal and severe. Lower lid biopsy was obtained for histology.
Of 49 charts reviewed, 14 patients had normal OSDI and 35 had dry-eye OSDI. There was no significant statistical difference between OSDI groups and all OSD findings. Basal tear test and lissamine green staining were not statistically different between the two OSDI groups. Comparing the ZA groups, 10 patients had normal grading and 39 had severe grading. No significant statistical differences were found between ZA groups and OSD findings; basal tear test and lissamine green staining were not statistically different between the ZA groups. Patients with severe ZA grading were found to have normal to mild OSD findings (anterior blepharitis=84.2 percent, vascularization=82.1 percent, MG obstruction=56.4 percent, turbidity=32.4 percent), in contrast to patients with severe ZA grading that had severe OSD (AB=15.8 percent, V=18 percent, O=43.6 percent, T=67.6 percent). Histology showed inflammatory response and increased number of dilated vessels in the posterior lid margin.
The OSDI questionnaire did not correlate with any ocular surface disease clinical signs. ZA grading was noted to be severe even in the cohort with mild disease.968
Portland, Ore. researchers report that there is still a wide range of refractive outcomes with two current endothelial keratoplasty techniques in combination with cataract surgery. They evaluated refractive error after combined Descemet stripping automated endothelial keratoplasty or Descemet’s membrane endothelial keratoplasty coupled with cataract surgery to determine whether the intended target refraction was achieved.
In 117 eyes with Fuchs’ endothelial dystrophy and cataract that underwent combined DSAEK (n=88) or DMEK (n=29) with cataract surgery, the surgeons targeted emmetropia by choosing a lens power from IOLMaster that provided a refraction of -1.25 to -1.5 D for DSAEK and -0.3 to -0.6 D for DMEK. Postop best spectacle-corrected visual acuity and SE were measured pre- and one to six months postop. The difference in actual versus targeted SE was calculated.
After DSAEK, mean BSCVA was 20/26 (r: 20/20 to 20/70), and the mean SE was -0.44 D (r: -3.125 D to +1.625 D). After DMEK, mean BSCVA was 20/26 (r: 20/20 to 20/50), and mean SE was -0.37 D (r: -2.5 D to +2.125 D). Mean postoperative SE was not significantly different between DMEK and DSAEK (p=0.691).
DMEK appeared to have slightly more reliable results, though the sample size was small, the surgeons say. The results suggest the need for further study of the hyperopic shift and IOL selection in this population.3081
Keratoplasty
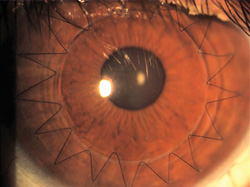
Italian surgeons offer a new anvil-like trephination pattern in penetrating keratoplasty assisted by femtosecond laser.
Thirty eyes underwent the procedure, in which anvil-shaped penetrating cuts are made with an IntraLase femtosecond laser on both donor and recipient corneas. A diode laser welding procedure was performed in order to improve the healing process.
|
They consider the short-term visual results and refractive results to be encouraging compared with those of conventional PK studies. Longer term follow-up and comparative studies are necessary to determine precise advantages of this technique.3077
Citing previous reports that avoiding overlap of the donor DMEK graft with the host Descemet’s membrane may promote graft adherence, surgeons at the Devers Eye Institute, Portland, Ore., retrospectively analyzed their results for a difference in the rate of re-bubbling procedures and primary graft failure between overlapped and non-overlapped cases.
They studied 52 DMEK cases performed for Fuchs’ dystrophy eyes; in 28 eyes, the host was stripped smaller than the graft, resulting in overlap of the graft and the host DM; in 24 eyes, the host was purposely stripped wider than the size of the graft to avoid overlap of the DMEK graft and host DM. The incidence of graft replacement and frequency of rebubbling was compared between the groups.
Fifteen of 28 (53.5 percent) grafts that overlapped with the host DM required rebubbling, significantly more than the 6/24 (25 percent) grafts without overlap of the host DM that required rebubbling (p=0.036). There was no significant difference in the rate of primary graft failure. There was a 10.7 percent PGF rate for the overlap group and 8.3 percent for the non-overlap group (p=1.0).
Avoiding overlap of the DMEK graft with the host DM appears to promote adherence of the graft and decrease the rate of rebubbling procedures. They call for a prospective, randomized study with a greater sample size to further validate this finding.3079
Air fluid exchange in DSAEK does not introduce a significant change in graft-host interface separation compared to the separation present after corneal sweeping, according to a group at the Cole Eye Institute, Cleveland.
DSAEK was performed by a single surgeon on 23 eyes in 23 patients, 18 with Fuchs’ endothelial dystrophy, two previously failed PK, and one each previously failed DSAEK, pseudophakic bullous keratopathy, and Brown-McLean syndrome. Intraoperative spectral domain OCT (iOCT) was executed after corneal sweeping and after air fluid exchange. Graft-host interface separation was digitally quantified in the axial and transverse dimensions and compared after corneal sweeping and after air fluid exchange using a paired t-test.
Average axial length of the graft-host interface was 34.6 +28.5 µm post-sweep and 59.6 +92.7 µm post-air fluid exchange (p=0.24). Average transverse length of the graft-host interface was 1.16 +1.15 mm post-sweep and 1.29 +1.65 mm post-air fluid exchange (p=0.62). No visible interface fluid was present in four eyes after corneal sweeping and in five eyes after air fluid exchange. iOCT, the group concludes, can evaluate the efficacy of surgical techniques in DSAEK by quantifying graft-host interface separation and confirming graft adherence in real-time.3083
For phakic and pseudophakic patients with bilateral Fuchs’ endothelial dystrophy, contrast sensitivity and BCVA were significantly improved in DMEK eyes compared to the untreated fellow eye, in a study from the Netherlands and Spain. Improvement of those parameters after surgery influenced the subjective perception of patients’ visual quality.
A total of 29 patients with a history of bilateral FED and unilateral DMEK were identified and divided into three groups, 12 phakic, 17 pseudophakic and 11 controls. Unilateral cataract, unilateral IOL, previous anterior segment surgery or any other concurrent ocular condition that may limit BCVA were exclusions. Pelli Robson contrast sensitivity test and Fansworth Munsell 100 Hue color vision test were used to assess contrast sensitivity and color vision. A specific questionnaire consisting of 11 questions was developed to measure the subjective visual quality. Individual variability was taken into account by measuring all visual parameters for the untreated (FED) and the treated eye (DMEK) of each subject. All parameters were compared between the phakic, pseudophakic and the control groups.
Comparing the eyes of each patient, statistically significant differences in BCVA and contrast sensitivity were found for the phakic and pseudophakic groups between FED and DMEK eyes. Contrast sensitivity of DMEK eyes in the phakic group did not significantly differ from the control group, while it differed significantly between the DMEK eyes of the pseudophakic group and the control group. No statistically significant difference was observed in the mean color vision of the FED and the DMEK eyes for the phakic and the pseudophakic groups. Subjective vision quality was rated significantly higher for the DMEK eye than for the FED eye in both the phakic and the pseudophakic groups.3092
Subtle, clinically undetectable residual interface fluid may be present at the end of DMEK surgery, possibly representing a risk for postoperative entire graft detachment or limitation in visual restoration, say researchers at the University of Cologne, Germany.
Ten patients (eight female) at the university were examined three to four hours, five to seven hours and seven to nine hours after DMEK surgery using both a time-domain OCT and a spectral-domain OCT. Parameters included presence, localization and potential reduction of graft detachment.
In all patients and at all time points, localized graft detachment and subtle, clinically undetectable interface fluid were observed. Graft detachments of differing degrees were localized at different positions of the cornea in between the examinations. Detachments were better visualized by SD OCT than by TD OCT.
Inconsistent localization of detachments is thought to be caused by interface fluid shift due to air bubble movement within the eye. These findings suggest considerable tissue rearrangements early after DMEK despite nearly complete anterior chamber air filling.3096
Researchers from the University of California, Irvine, have devised a “mini-bubble” technique that may be useful in both deep anterior lamellar keratoplasty and in donor tissue preparation for DSAEK. It features wide pulse spacing and very low pulse energy delivered in multiple passes, resulting in a smoother stromal plane in the deep cornea, compared to tight spot spacing and higher pulse energy levels.
Ten fresh human corneal scleral donors were mounted on artificial anterior chambers and exposed to femtosecond laser dissections 30 to 50 µm anterior to Descemet’s membrane using an iFS 150 kHz laser. Variables studied were spot separation, pattern of laser scanning and pulse energy. Key outcomes were ease of tissue separation, gross inspection of the tissue bed, SDOCT and Trypan blue/alizarin red staining of the endothelium.
Separation of the tissue plane was easiest with a combination of close spot separation (4x4 µm) and high pulse energy (3.5 microjoules). The smoothest bed was obtained with wide pulse spacing (10x10 µm); low pulse energy just higher than threshold (0.4 5 to 0.6 µJ) and eight alternating raster and spiral passes, rotated 45 degrees between each pair of passes. OCT revealed stromal separation either at or slightly anterior to Descemet’s membrane. Staining showed no evidence of endothelial injury.3100
Recognizing that DSAEK causes a transient increase in recipient corneal hydration, surgeons in Aarhus, Denmark wanted to learn whether structural changes in the recipient cornea also occur.
For at least one year after DSAEK, they followed 76 patients treated for endothelial dystrophy. At all visits, they measured central corneal thickness and calculated the difference in CCT from three days to one year
postop (ΔCCT=CCT3days–CCT1year) as a crude measure of postoperative corneal edema. At their latest visit, patients were examined with SD-OCT to determine recipient corneal thickness (RCT). SD-OCT was also used to determine CCT in a group of normal corneas.
From one to six years after DSAEK, RCT averaged 490 ±29 μm, which was significantly less than the CCT of 531 ±18 μm that was observed with SD-OCT in normal corneas (p< 0.001). RCT measured 487 ±28 μm after one year (n=43); 491 ±29 μm after two years (n=24); and 505 ±26 μm after three to six years (n=9), with a slight but significant increase over time. Correlating RCT with ΔCCT also showed a significant correlation between postop corneal edema and RCT, with more edema causing the recipient cornea to become thinner over time (p=0.006).
The correlation between postop edema and RCT may suggest that wash-out of stromal ground substances induce the thinning, with the subsequent gradual increase in thickness being caused by resynthesis of extracellular material, the authors hypothesize. However, the long-lasting nature of the observed changes could also suggest underlying structural abnormalities in endothelial dystrophy, they conclude.3101
Miscellaneous
In evaluating the product besifloxacin ophthalmic suspension, 0.6%, researchers have identified a number of new bacterial conjunctivitis pathogens. The study compared the prevalence and distribution of ocular pathogens encountered across five multicenter, randomized, double-masked, clinical studies evaluating besifloxacin in 2009 to 2011 versus 2004 to 2007.
A total of 2,348 baseline isolates from 3,379 patients were collected; 1,324 recovered in 2004 to 2007 and 1,024 in 2009 to 2011. Recovered isolates across all treatment groups were evaluated for baseline frequency, microbial eradication and antimicrobial susceptibility profiles.
Fifteen new bacterial conjunctivitis pathogens not recovered from study eyes between 2004 and 2007 were isolated in the later studies, including the potentially emerging pathogens Dolosigranulum pigrum (n=26) and Corynebacterium accolens (n=5). The five most frequently isolated species or taxonomic groups remained the predominant bacterial conjunctivitis pathogens across all five besifloxacin studies. Microbial eradication rates of pathogens isolated in besifloxacin-treated subjects in the more recent studies included 100-percent eradication of D. pigrum (14/14), Acinetobacter calcoaceticus/baumannii complex (3/3), and Elizabethkingia meningoseptica (2/2).
The most prevalent bacterial conjunctivitis pathogens remained consistent over the seven-year period; however, additional pathogens have emerged as causative agents of bacterial conjunctivitis. This emergence of additional pathogens may be due to improved methods for the identification of bacterial isolates, or changes in human or bacterial ecology that promote the spreading of these species to the ocular surface, the authors say.5450
Corneal decompensation is a known risk of anterior chamber implantation of older glaucoma shunts, but far less is known of this risk with Ex-Press shunts. In what they call the first case series to document corneal decompensation after Ex-Press placement, surgeons from New Orleans and Italy report that DSAEK surgery can be successful in treatment of corneal decompensation after Ex-Press valve placement.
The study reviewed all cases of DSAEK performed since 2005 that had prior Ex-Press shunt surgery from one corneal surgeon. Ocular history including number of surgical procedures, intraocular pressure and BCVA before and after Ex-Press surgery and before and after DSAEK, as well as surgical complications were reviewed.
The average age and average IOP prior to Ex-Press shunt placement was 63.8 years ±3.4 standard deviation and 24.6 mmHg ±0.4 SD respectively. BCVA prior to Ex-Press shunt placement was logMAR 0.64 ±0.16 SD. The average postoperative IOP after Ex-Press shunt was 16.8 mmHg ±1 SD. The mean number of surgeries prior to DSAEK was 2.8 ±1.64. Four of the five patients with corneal decompensation after Ex-Press placement had one or more prior filtering procedures with a mean of 1.75 ±0.83. One of these patients also had two prior failed Ex-Press shunts. Vision decreased to count fingers in all patients before DSAEK. The average age at which significant corneal decompensation was identified and DSAEK was performed was 66 years ±3.2 SD with average time of onset of corneal edema after Ex-Press shunt of 2.2 years ±0.44. The average BCVA after DSAEK was 0.78 ±0.18 with decreased vision resulting from optic nerve damage in all cases. All corneas remained clear. IOP was controlled in four patients; one required cyclocryotherapy for IOP control.
Long-term follow-up of patients who have had Ex-Press shunt surgery is needed to determine if the shunt device itself increases the risk of corneal decompensation, the authors say.3089 REVIEW
Dr. Afshari is a professor of ophthalmology and Chief of Cornea and Refractive Surgery at the Shiley Eye Center, University of California San Diego.