It’s been a little over a year since surgeons in the United States gained access to three FDA-approved non-diffractive/non-multifocal IOLs: the Acrysof IQ Vivity; Tecnis Eyhance; and RayOne EMV. There’s been an air of excitement about the potential in these lenses, which aim to give patients a wider range of vision with fewer side effects—but are they performing as expected? This article reviews each lens’s unique features and design, and how each is fitting into day-to-day operations nationwide.
Vivity
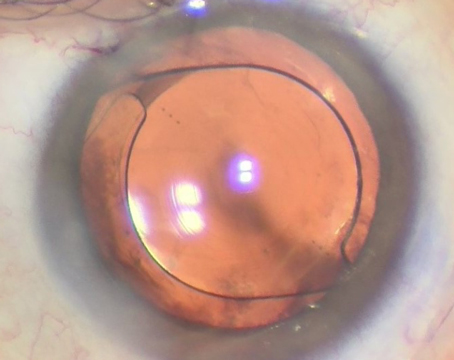
 |
| The Alcon Vivity is a non-diffractive EDOF IOL that delivers monofocal-quality distance vision and has improved acuities at intermediate ranges. |
The AcrySof IQ Vivity from Alcon was the first non-diffractive EDOF IOL available in the U.S. Using technology on the anterior surface of the IOL to achieve the extended-depth-of-field vision, this lens has a negative spherical aberration on the anterior surface, which compensates for the positive spherical aberration of the cornea. The Vivity is composed of a hydrophobic acrylate/methacrylate copolymer with a blue-light-filtering chromophore and standard UV-light filtration. It’s available in powers of +15 D to +25 D in 0.5-D increments, and also comes in a toric version.
Alcon says this lens delivers “monofocal-quality distance vision with excellent intermediate and functional near vision.”
“This really is a novel type of lens category for us,” says Brandon Baartman, MD, of Omaha, Nebraska, who was also part of the clinical trial as a surgical fellow. “We’ve had extended-depth lenses before, but not ones that were truly non-diffractive in the way they work.”
Instead of splitting light into multiple zones of vision as is done with traditional multifocal IOLs, the Vivity uses a central optical element to change the shape of the wavefront. “This lens was born out of the desire to achieve a more functional range of vision after cataract surgery, without some of the more glaring downsides of a light-splitting or diffractive-type multifocal lens,” Dr. Baartman continues. “The way patients are using this lens speaks to its strengths, which are distance and dashboard vision.”
The ideal candidate for Vivity is someone with a refractive mindset who desires more freedom from glasses, he says. “This is where the lens really shines. Compared to a monofocal lens, the defocus curve is such that it allows better acuities at intermediate ranges. Compared to a trifocal or bifocal, the Vivity will have the added benefit of fewer dysphotopsias—in particular fewer halos around lights at night, compared to true diffractive multifocals,” Dr. Baartman says.
It’s been a little more than a year since the FDA approved the Vivity. In the clinical study, only 1 percent of patients reported that they were bothered “very much” by halos, and there were no complaints of glare. The study also showed, at six months postop, 98 percent, 97 percent and 58 percent of patients reached 20/32 or better for binocular distance, intermediate and near vision, respectively.
Dr. Baartman believes there’s an opportunity to create a better blended monovision with a slight offset in the non-dominant eye. “That’s been an exciting newer use of this technology,” he says. “Whereas I would never offset one of the eyes for a near target with a true multifocal—there wouldn’t be a purpose—a lens like Vivity would help overcome some of the obstacles we face with monofocal monovision, namely an intermediate dead zone for patients who want good distance and near vision. Now you can get that with a little less of the reduction in intermediate vision.”
He says hitting the refractive target is important. “Early on, I thought that, perhaps with the extended focal depth, there might be a little bit more forgiveness with refractive error. But for those patients who are getting Vivity, keep in mind that these are refractive-minded patients who are expecting a lot. Excellent cataract surgery starts with excellent and meticulous biometry and care for the tear film and preparation of a patient’s eye for surgery,” Dr. Baartman says.
“Once you’re in surgery, I think the proper techniques for any refractive cataract surgery apply, including the use of the best available technology, whether it’s intraoperative aberrometry or femtosecond laser in that particular surgeon’s hands,” he continues. “And, treating any significant astigmatism with a toric lens or limbal relaxing incisions is beneficial at the time of surgery to help improve outcomes.”
In his experience, patients with significant corneal or retinal pathology wouldn’t be good candidates. “People with ectasia, corneal scars or even significant post-refractive corneas may not be the best candidates, as well as those with severe glaucoma,” Dr. Baartman says. “But I think with Vivity, patients with a mild ERM, or early macular degeneration that’s been stable are patients who might be reasonable candidates.”
Eyhance
The Tecnis Eyhance from Johnson & Johnson Vision is a one-piece monofocal designed to extend the depth of focus compared to other monofocals. Its shape is unique, with a 6-mm biconvex, aspheric anterior surface and a frosted 360-degree posterior square edge. J&J Vision says the Eyhance IOL delivers a 30-percent improvement in contrast in low-light conditions at 5 mm vs. a standard monofocal. Its powers range from +5 D to +34 D in 0.5-D increments, and it comes in a toric version. The lens is available on the preloaded Tecnis Simplicity delivery platform.
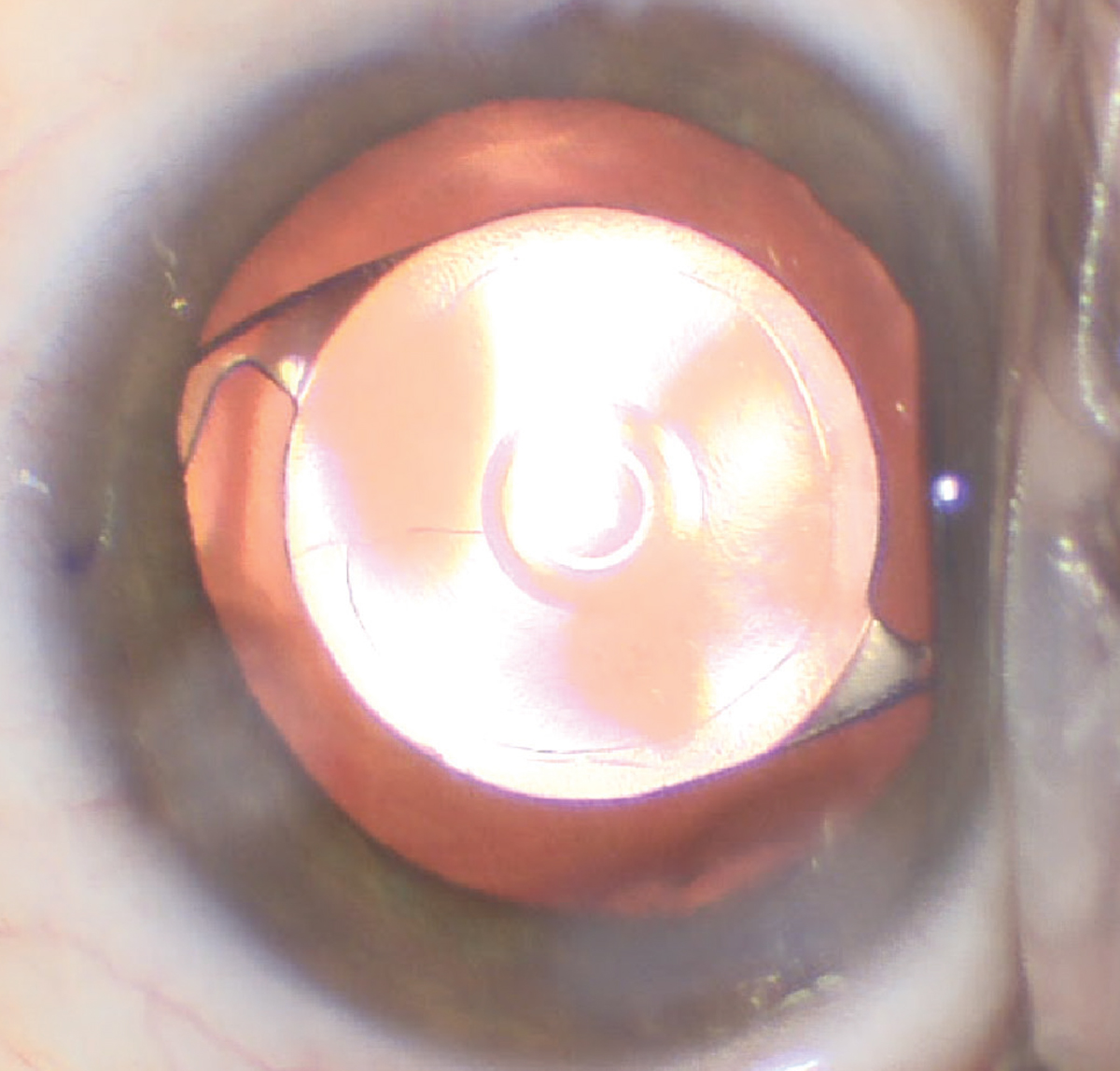
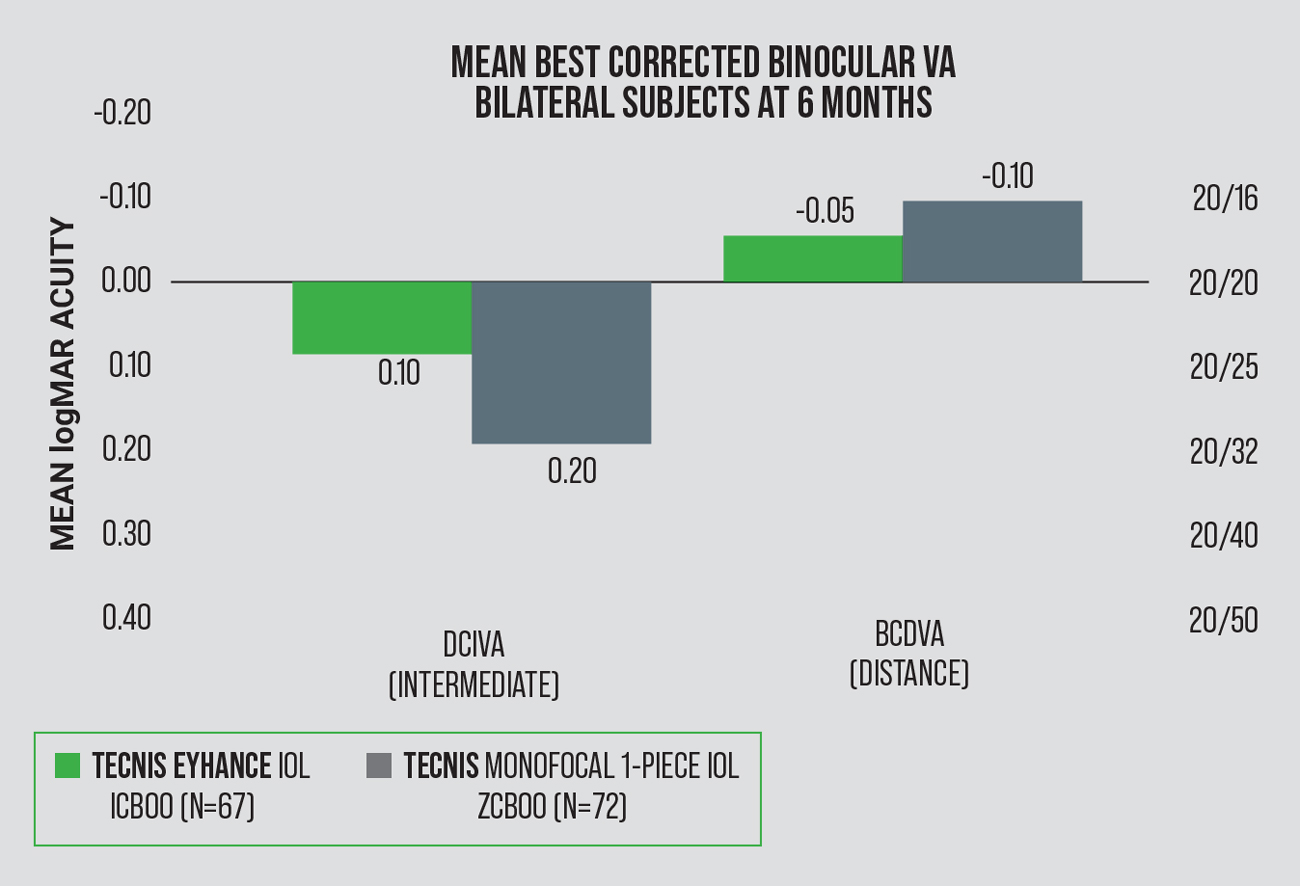 |
| Figure 1. Tecnis Eyhance IOL (ICB00) vs. Tecnis monofocal 1-piece IOL (ZCB00): Intermediate and distance vision at six months post-surgery. The Eyhance achieved a statistically significant, 1.1-line improvement in monocular and binocular intermediate vision at six months vs. a monofocal. The monofocal had 0.4-line better distance vision than the Eyhance. |
Douglas D. Koch, MD, a professor and Allen, Mosbacher and Law Chair in Ophthalmology at Baylor College of Medicine in Houston, has been closely involved with the development of this lens and says it’s essentially the first “monofocal plus” IOL.
“The lens gives you that monofocal-type sharpness of vision, with about one more line of near vision than a standard monofocal, on average. It does so by having a very subtle increase in steepness over the central zone (2 mm) so it just blends in, compared with a discrete zone,” Dr. Koch says. “The benefit I find is that many patients can get great distance vision and yet still see their cell phone at arm’s length. I’ve also found that there are no dysphotopsias associated with the optical benefits of this lens.”
The one-line advantage at near has been demonstrated in both laboratory and clinical studies, but Dr. Koch says it’s important to point out that he—and likely many other surgeons—don’t indicate that to the patient preoperatively. “Eyhance doesn’t meet the FDA criteria for EDOF, and some patients may get increased near and some may not. For example, if the patient is plano, you may have some near, but if the patient is +0.25, the patient may not have any near benefit. They may have great distance vision if they end up a little hyperopic because of the flatter landing zone, but they may not have the near benefit, so I don’t talk to them about it in advance. If the patient gets the one line of near vision postoperatively, then that’s a wonderful side benefit. But because it’s such a subtle amount, it’s hard to convey that to the patient, and we hate to raise expectations.”
When it comes to nailing the distance side, Dr. Koch says he’d be wary of aiming too far on the minus side. “I might aim for plano, or even +0.1, so that I get really good distance vision for the dominant eye. For the non-dominant eye, you can aim for, say, -0.5 and that will give them 20/25 at distance, yet they might get quite a bit of near benefit from it,” he says. “That’s one way to do a micro-monovision. Or you can aim for plano in both eyes. You can often get a near benefit, but it’s kind of nice to do a little bit of a variation in one eye versus the other.”
The bigger and flatter landing zone is an advantage for post-myopic-LASIK eyes, says Dr. Koch. “It’s a little more tolerant to defocus and you’re more likely to get 20/25 or even 20/20 uncorrected in post-LASIK eyes because of the flatter landing zone,” he notes. Dr. Koch says Eyhance may not be ideal for patients who have a lot of irregular astigmatism or who have had hyperopic LASIK because of the lens’s amount of negative spherical aberration.
Eyhance is delivered via the one-step Tecnis Simplicity system. “This platform has superb optical quality in terms of a very high Abbe number with reduced chromatic aberration. The surface is pristine and doesn’t deteriorate over time,” Dr. Koch says. “The toric version comes on the new Toric II platform with roughened or textured outer edges on the haptics.
“I haven’t heard of any adverse events, other than the occasional patient with glare,” he adds. “I haven’t seen anything that indicates there are any complications associated with the design.”
RayOne
The latest IOL to be approved is the RayOne EMV (“enhanced monovision”) from Rayner Global. This monofocal lens offers up to 2.25 D (with 1-D offset) of extended depth of focus. The single-piece design is 12.5 mm, made of Rayacryl hydrophilic acrylic, and available in powers of +10 to +30 D in 0.5-D increments. The lens is suitable for patients who aren’t candidates for diffractive trifocals and are looking for some spectacle independence and reduced dysphotopsia.
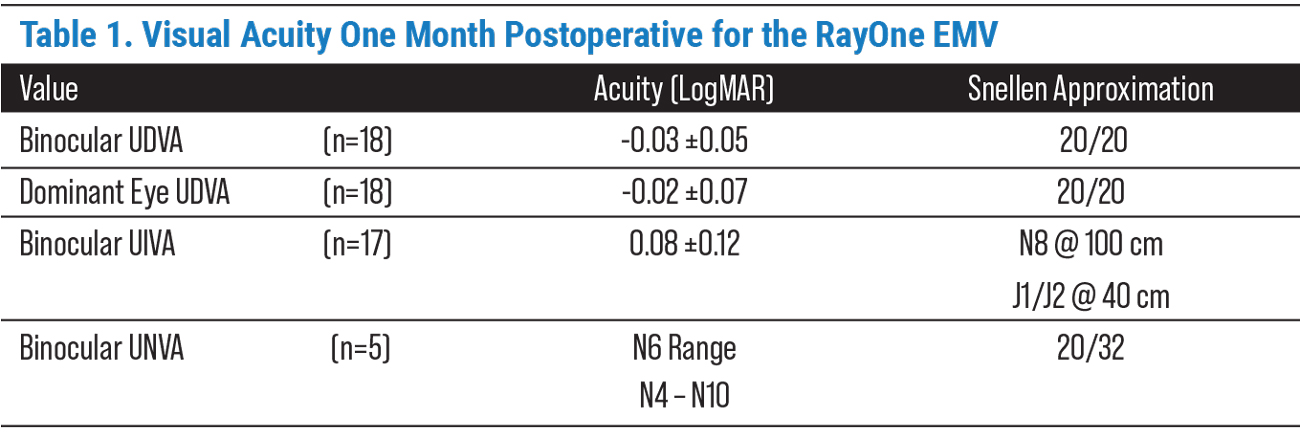 |
In the one-month postoperative period, patients in the clinical study reported high satisfaction with their refractive outcome, including 70 percent who said they had spectacle independence at distance, intermediate and near. One-hundred percent of patients in the study were dysphotopsia-free.
The company says that, like other IOLs in its catalog, the RayOne EMV has reduced sensitivity to decentration and tilt. “With the aspheric lens, there tends to be better centration so it’s less dependent on the pupil location and size,” says Lisa Nijm, MD, an assistant clinical professor of ophthalmology at the UIC Eye and Ear Infirmary. “This helps decrease the need for the lens to be exactly centered for the patient to achieve their optimal visual acuity after surgery.”
A study conducted in Madrid1 showed 100 percent of patients who received the RayOne EMV achieved spectacle independence in the distance and intermediate range. One in three had functional near vision without spectacles, and the average reading add power at 33 cm was reported to be +1.5 D.
Dr. Nijm says she tries to get as close to plano as possible for the visual target. “I usually go for the first minus, and that’s what I do with most of these lenses,” she says.
The lens demonstrates binocular distance vision and a smoother transition between the dominant and non-dominant eyes. Dr. Nijm adds, “The aspheric surface creates greater contrast sensitivity and improved visual acuity in lower-light situations.”
She says the enhanced square-edge design has been shown to create a barrier that reduces epithelial cell migration, which can cause posterior capsular opacification. “It may be that there is a decreased rate of needing a YAG capsulotomy after surgery with this lens,” Dr. Nijm speculates.
A study did show low incidences of YAG capsulotomy rates: 0.6 percent at 12 months, and 1.7 percent at 24 months.2
The RayOne EMV also comes pre-loaded on Rayner’s patented “Lock & Roll” technology, offering a smoother delivery. Dr. Nijm says this makes it easier for surgeons to implant the IOL in almost any setting.
“This pre-injector system makes it easy for the OR staff to be able to load the lens consistently each time, no matter where they are and no matter how much experience they have,” she says. “I think especially when you’re operating in different locations, or perhaps with newer techs—since we’ve had a lot of turnover and shortages—you may have people filling in, so having a pre-loaded system makes a difference.”
Dr. Nijm says this lens, as well as the other newcomers, are bringing exciting options to patients in the United States. “Europe has enjoyed a variety of lenses for years, and to be able to customize and personalize the lens choice for each patient is fantastic,” she says.
This article has no commercial sponsorship.
Dr. Baartman is a consultant for Alcon. Dr. Koch is a consultant for Alcon, Bausch + Lomb, Johnson & Johnson and Zeiss. Dr. Nijm is a consultant for Rayner.
1. RayOne EMV IOL receives FDA approval. Accessed May 12, 2022. https://rayner.com/rayone-emv-iol-rayner-receives-fda-approval/.
2. Mathew RG, Coombes AG. Reduction of Nd:YAG capsulotomy rates after implantation of a single-piece acrylic hydrophilic intraocular lens with 360° squared optic edge: 24-month results. Ophthalmic Surg Lasers Imaging 2010;41:6:651-5.