For decades, clinicians have had to rely on their subjective evaluation of signs and symptoms in order to accurately diagnose and treat dry eye and ocular surface disease. Recent years have witnessed a flurry of developments in the realm of objective dry-eye diagnosis, however, with several devices becoming available around the same time. The newest addition to these objective measurement tools is the Tear Microassay System from Advanced Tear Diagnostics. Here’s a look at how the system works.
Lactoferrin Explained
The Tear Microassay System measures the amount of the protein lactoferrin on a patient’s ocular surface, using it as a marker for dry eye.
“Lactoferrin is a multifunctional protein that’s part of the transferrin family,” explains Terrence O’Brien, MD, professor of ophthalmology at the University of Miami’s Bascom Palmer Eye Institute. Dr. O’Brien has experience working with lactoferrin as a marker for dry eye, and is interested in seeing what this new test may bring to the clinic. “It’s more of a global marker, and it’s present not only in tears but also in saliva, mother’s milk and nasal secretions. It’s also one of the components of the immune response, has demonstrated significant antimicrobial activity and is part of the eye’s natural defenses. This antimicrobial aspect of it is one of the reasons why I’m interested in it. It’s been identified as one of the tear proteins that may be part of the innate defense of the mucosal surface, and it has bactericidal and even fungicidal properties. In addition to binding iron, which bacteria use as an element necessary for their growth, it also binds to the lipopolysaccharide of bacterial cell walls. The oxidized iron that’s part of lactoferrin oxidizes bacteria, forming peroxide. This action affects the membrane permeability and results in the breakdown of the bacteria.
“My interest in this stems from this antimicrobial mechanism being part of the innate immune system, and I think the test may have broader applications,” adds Dr. O’Brien. “For example, it may be that lactoferrin levels can tell us which patients might be at risk for developing an infection from wearing contact lenses.”
The Test
The lactoferrin test consists of introducing a micropipette into the patient’s canthus and harvesting a very small sample of tears, 0.5 µl. The sample is put in a diluent and the mixture is shaken, a step that amplifies the amount of lactoferrin. The mix is then placed in a small well on a strip, and, according to Advanced Tear Diagnostics’ Jeffrey Busby, the diluent chases the tear up the strip and, when the sample is placed in the microassay system, the system determines how much lactoferrin is in the sample.
A result of 1.4 is considered normal, and anything below that means the patient has dry eye. According to company studies, the test’s sensitivity is 83 percent, and it’s specificity is 98 percent. There is already a diagnostic code assigned to the test, as well. The system can also process different samples of tears to test for immunoglobulin E, to look for the presence of ocular allergy.
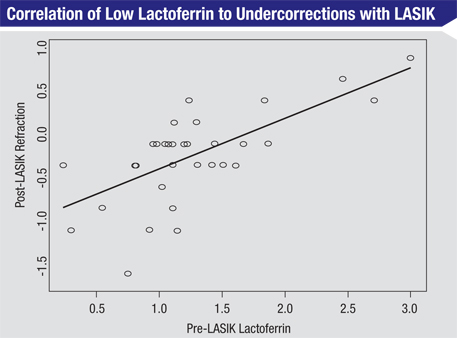 |
Now that clinicians can use lactoferrin levels to determine if a patient has dry eye, Dr. O’Brien says the next step is to study the results and see how they correlate with signs, symptoms and disease severity levels. “We need to figure out the correlation between the quantitative nature of this test result and the severity of the disease,” he says. Some progress has been made along these lines: In a small, non-published study that Dr. O’Brien conducted with Duke University’s Alan Carlson, MD, several years ago, they found lactoferrin levels may be associated with postop LASIK results. In the study, the researchers tested the lactoferrin of 32 patients before their LASIK procedures and then prior to their post-LASIK follow-up exams. Preoperatively, six patients had low lactoferrin, 21 had normal levels, and five had elevated lactoferrin. “We found that those patients who had lower levels of lactoferrin preoperatively were more prone to regression of effect and a lesser outcome of laser vision correction,” says Dr. O’Brien. Elevated lactoferrin suggested an increased risk for postop hyperopia. All of the low-lactoferrin patients had a postop refraction of -0.25 to -1.5 D; only 19 percent of the normal patients were outside the -0.25- to +0.25-D range; and 80 percent of the high-lactoferrin patients had hyperopic refractions of +0.5 D or greater. “It’s possible that an LVC surgeon, or a surgeon planning on implanting an advanced technology IOL, who uses the lactoferrin test to screen patients could uncover individuals who have mild to moderate disease that could impact the outcome,” says Dr. O’Brien. “So, this might be a broad screening tool for OSD as well as a perioperative screening tool that could be used in advance of surgery to uncover patients who may be at risk for a lesser outcome. The surgeon could then treat them preoperatively in an effort to improve the ocular surface.”
As for the steps after a clinician finds that a patient has low lactoferrin, there is some evidence that lactoferrin supplementation can help. In a non-published study outlined in a letter to the editor in Ophthalmology, physicians from Tokyo administered oral lactoferrin to 10 patients with Sjögren’s syndrome and used 14 eyes of seven other Sjögren’s patients as controls.1 The researchers reported that mean corneal sensitivity, tear breakup time, tear-film lipid layer thickness, vital staining, squamous metaplasia grades, symptoms and goblet cell densities all improved significantly after a month of lactoferrin supplementation. The parameters then worsened a month after supplementation ceased. The control group showed no significant changes. Dr. O’Brien cautions clinicians to evaluate oral supplements carefully, though. “If lactoferrin is low, there are supplements available,” he says. “But these aren’t tightly regulated by the FDA, so evidence is lacking in terms of trials to tell us which form of lactoferrin would be ideal, which dosage is best and if it’s harmful to take too much. We have this problem with other supplements that people may take without knowing their true safety.”
Making Sense of It All
Dr. O’Brien says clinicians now have to determine where lactoferrin testing fits into their dry-eye diagnostic paradigm.
“We’re finding out that dry-eye disease involves a complex biological system of multiple molecules, with each playing a different role in terms of normal homeostasis of tear function,” he says. “I think the lactoferrin will be complementary to other tests such as those for tear-film osmolarity and MMP-9 to help us screen for dry eye.
“Lactoferrin might also have other implications in terms of how the protein really functions in the natural prevention of infection from organisms that blow onto the tear film, in contact lens wearers and in surgery patients,” Dr. O’Brien continues. “However, more work needs to be done to bring a clinical meaning to the quantitative result of the test. To that end, studies are currently being coordinated and are getting under way, and I hope we’ll have some data soon in different clinical settings.” REVIEW
Dr. O’Brien has no financial interest related to Advanced Tear Diagnostics or its products.
1. Dogru M, Matsumoto Y, Yamamoto Y, et al. Lactoferrin in Sjögren’s syndrome. Ophthalmology 2007;114:12:2366-7.





